Approach
Patients typically present with cyanosis and/or a murmur. Echocardiography is the definitive investigation for diagnosis of TOF and should be ordered in any newborn with a suspected diagnosis of congenital heart disease.
History
Certain genetic syndromes are associated with an increased incidence of TOF, such as DiGeorge and Down's syndromes. There may be a history of abnormality on fetal echocardiogram that suggests cardiac pathology.
A typical infant presents in the newborn nursery with a murmur. Cyanosis is usually noted. The degree of cyanosis may vary and can be subtle, and some clinicians advocate routine screening of all neonates with pulse oximetry.[18]
Some infants may not present at birth but rather may present later with increasing cyanosis, murmur, or hypercyanotic (tet) spells. Hypercyanotic spells may present as episodic, increasing cyanosis in a baby with TOF. The baby is typically crying and breathing deeply and rapidly, but may not be in significant respiratory distress. The typical murmur of TOF may disappear during the spell. This presentation is potentially life-threatening and requires rapid intervention.
TOF with severe pulmonary obstruction is a more severe presentation and may present in a newborn who appears severely cyanotic at birth. Infants with severe pulmonary obstruction or a hypercyanotic spell may present with severe cyanosis and acidosis due to tissue hypoxia.
Physical examination
Can vary significantly depending on the degree of pulmonary obstruction. The infant with mild obstruction is typically comfortable, and cyanosis may be difficult to discover on physical examination. With moderate obstruction the cyanosis is likely to be apparent on examination and the infant is typically comfortable. With severe obstruction the baby may have significant tachypnoea and cyanosis.
The cardiac examination typically finds an increased right ventricular (parasternal) impulse. S1 is normal and S2 is single. There is typically a 3/6 harsh systolic ejection murmur, heard best at the left sternal border. The murmur on examination represents blood flow across the pulmonary outflow and not the ventricular septal defect. The intensity of the murmur depends on the degree of pulmonary stenosis and decreases with severe stenosis.
Investigations
Transthoracic 2-dimensional and Doppler echocardiography is the preferred technique for defining the anatomical diagnosis. In the vast majority of cases no further testing is needed pre-operatively. Sedation may be judiciously used if the child is not co-operative with the examination.
[Figure caption and citation for the preceding image starts]: Anatomy and pathophysiology of tetralogy of Fallot (TOF): normal heart structure (a) promotes unidirectional flow of de-oxygenated blood (blue) into the lungs and oxygenated blood (red) into the aorta; in TOF (b) pulmonary stenosis and narrowing of the right ventricular outflow tract (RVOT) impedes the flow of de-oxygenated blood into the lungs, and both the ventricular septal defect (VSD) and overriding aorta (*) promote the flow of de-oxygenated blood into the systemic circulation, to produce cyanosis (sometimes referred to as 'blue baby' syndrome), right ventricular hypertrophy (RVH) is also present; (c) a Doppler echocardiogram shows mixing of de-oxygenated blood from the right ventricle (RV) and oxygenated blood from the left ventricle (LV) as blood is pumped out the over-riding aorta (Ao) in a patient with TOF (RA=right atrium, LA=left atrium)Multimedia Library of Congenital Heart Disease, Children’s Hospital, Boston, MA, editor Robert Geggel, MD; used with permission [Citation ends].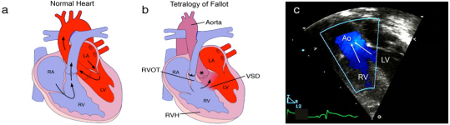
Pre-ductal and post-ductal (right arm and either leg) pulse oximetry should be ordered if there is any suspicion of a congenital cardiac malformation.[19] A hyper-oxygenation test can be used to determine whether hypoxaemia is from a pulmonary or a cardiac lesion.
ECG will often show evidence of right ventricular hypertrophy and may show right axis deviation beyond normal limits for age. [Figure caption and citation for the preceding image starts]: ECG in tetralogy of Fallot showing right ventricular hypertrophyFrom the collection of Dr Jeffrey Gossett; used with permission [Citation ends].
A chest x-ray is classically described as a boot-shaped heart, but most patients do not have this finding. The presence of a right aortic arch may be noted in a subset of patients, particularly those with 22q11 deletion.[9]
Cardiac catheterisation is usually unnecessary in diagnosing TOF and may induce hypercyanotic spells.[17] If there is significant concern for coronary artery anomalies that cannot be defined echocardiographically, then advanced imaging modalities including cardiac computed tomography angiography and magnetic resonance imaging are often used.[20] Anomalies in the distribution or course of the coronary arteries may be present in approximately one third of patients with TOF.[21]
Use of this content is subject to our disclaimer