Aetiology
Little is known about the exact aetiology of TOF. There is most likely to be interplay between genetic and environmental factors, but this has not been fully defined. One study of pregnant women with a first-degree relative with congenital heart disease (CHD) found 178 per 6640 (2.7%) pregnancies with CHD.[6]
There is a well-accepted association between certain genetic defects and CHD. Patients with trisomy 21, 18, or 13 have a higher incidence of TOF than infants without trisomy.[7] A retrospective analysis in patients with apparently non-syndromic TOF found 10 out of 21 patients to have deletions of chromosome 22q11 (DiGeorge's and associated syndromes), suggesting a region on this chromosome may harbour a TOF susceptibility gene.[8] In an earlier study comparing patients who had TOF with and without chromosome 22q11 deletion, every patient with TOF and 22q11 deletion was found to have an additional conotruncal anomaly.[9] Alagille's syndrome, a syndrome with cardiovascular phenotypes ranging from mild pulmonary stenosis to TOF with severe pulmonary obstruction, has been found to be due to mutations in the Jagged1 gene.[10] Additionally, mutations in Jagged1 have been associated with non-syndromic forms of TOF.[11] A prospective study looking for mutations in NKX2.5 in patients with known TOF found approximately 4% of patients with non-syndromic TOF to have a mutation in NKX2.5.[12]
Increasing evidence suggests environmental factors may play a significant role in some cases of CHD.[13] Maternal diabetes, maternal phenylketonuria, and maternal ingestion of retinoic acids or trimethadione have all been associated with an increased risk of CHD.[14][15][16]
Pathophysiology
In TOF, the pathophysiology and management are dictated by 3 specific anatomical factors:
1. Degree of right ventricular outflow tract obstruction
Typically occurs at multiple levels, including below the pulmonary valve (subvalvular or infundibular stenosis), at the level of the valve (valvular pulmonary stenosis), and above the valve (supravalvular stenosis). The degree of pulmonary obstruction determines whether the infant is cyanotic or acyanotic by affecting the amount of blood that shunts right to left at the ventricular septal defect (VSD).
TOF with mild pulmonary obstruction is typically not a cyanotic lesion. There is no significant restriction to the flow of blood into the pulmonary arteries and therefore the infant is well saturated.
TOF and significant pulmonary obstruction result in a cyanotic infant. This is because blood in the right ventricle has a higher resistance to overcome in order to enter the pulmonary circulation. Blood is shunted from the right ventricle to the aorta through the VSD and into the systemic circulation without being oxygenated in the pulmonary circulation.
2. Pulmonary artery anatomy
Pulmonary artery anatomy can dramatically affect the physiology.
Pulmonary atresia with VSD (TOF with pulmonary atresia) and absent pulmonary valve syndrome (TOF with absent pulmonary valve) are very different physiologically and are considered different disease processes from TOF. For that reason, they are not discussed here.
3. Non-restrictive, mal-alignment VSD
Anterior mal-alignment VSD in TOF is nearly always non-restrictive. With a large, non-restrictive VSD, the pressure in the right ventricle and left ventricle equalises. In this case, the VSD does not determine the degree of shunting. The degree of shunting in TOF is therefore due to the relative resistance to flow of the pulmonary versus systemic circulations.
Additional VSDs may be present and should be looked for as these may complicate the postoperative course.
Hypercyanotic spells, or tet spells, are episodes of severe cyanosis associated with hyperpnoea. They result from an increase in right ventricular outflow tract obstruction causing a decrease in the pulmonary blood flow and an increase in right-to-left shunting across the VSD. The exact aetiology of hypercyanotic spells is unclear, but they are thought to be initiated by increases in the right ventricular infundibular contractility. Hypercyanotic spells may be self-limited; however, if sustained, they can result in brain ischaemia or death.[17][Figure caption and citation for the preceding image starts]: Anatomy and pathophysiology of tetralogy of Fallot (TOF): normal heart structure (a) promotes unidirectional flow of de-oxygenated blood (blue) into the lungs and oxygenated blood (red) into the aorta; in TOF (b) pulmonary stenosis and narrowing of the right ventricular outflow tract (RVOT) impedes the flow of de-oxygenated blood into the lungs, and both the ventricular septal defect (VSD) and overriding aorta (*) promote the flow of de-oxygenated blood into the systemic circulation, to produce cyanosis (sometimes referred to as 'blue baby' syndrome), right ventricular hypertrophy (RVH) is also present; (c) a Doppler echocardiogram shows mixing of de-oxygenated blood from the right ventricle (RV) and oxygenated blood from the left ventricle (LV) as blood is pumped out the over-riding aorta (Ao) in a patient with TOF (RA=right atrium, LA=left atrium)Multimedia Library of Congenital Heart Disease, Children’s Hospital, Boston, MA, editor Robert Geggel, MD; used with permission [Citation ends].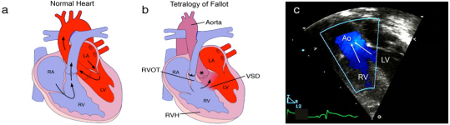
Classification
Variants of TOF
There is no standard classification for TOF, but many experts would use the following classification:
Cyanotic TOF (also known as blue tet): infants with TOF and moderate to severe pulmonary obstruction are cyanotic at birth due to right-to-left shunting of de-oxygenated blood from the right ventricle across the VSD to the body.
Acyanotic TOF (also known as pink tet): infants with TOF and mild pulmonary obstruction are commonly acyanotic because there is little or no right-to-left shunting of blood at the ventricular level. These patients still undergo complete intracardiac repair.
Pulmonary atresia/VSD: sometimes referred to as TOF with pulmonary atresia and is anatomically and physiologically very different. It is often associated with malformation of the central pulmonary arteries.
Absent pulmonary valve syndrome: sometimes referred to as TOF with absent pulmonary valve. It is often associated with tracheobronchial compression and malformation.
Use of this content is subject to our disclaimer