Approach
Pyloromyotomy is the definitive treatment.
Fluid resuscitation
Fluid and electrolyte replacement is paramount to the successful management of the infant with pyloric stenosis.
Surgery must be delayed until hypovolaemia and electrolyte disturbances are corrected. If alkalosis is not corrected, it will prolong the risk for postoperative depression of respiratory drive. Severely volume-depleted patients should receive a bolus of normal saline prior to initiating fluid replacement. Intravenous fluid replacement should be provided at 1.5 times maintenance rate with 5% dextrose plus 0.45% saline. Intravenous fluid should not contain potassium until the urine output is adequate (1-2 mL/kg/hour).
Surgical treatment
Pyloromyotomy involves the extramucosal longitudinal splitting of the pyloric muscle.[1][Figure caption and citation for the preceding image starts]: Laparoscopic port placement.From the collection of Dr Jeffrey S. Upperman; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Laparoscopic knife pyloric incisionFrom the collection of Dr Jeffrey S. Upperman; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Laparoscopic knife pyloric incisionFrom the collection of Dr Jeffrey S. Upperman; used with permission [Citation ends].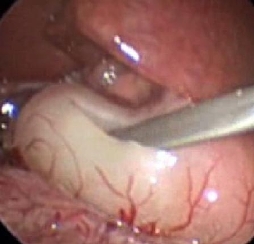 [Figure caption and citation for the preceding image starts]: Muscle-splitting manoeuvreFrom the collection of Dr Jeffrey S. Upperman; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Muscle-splitting manoeuvreFrom the collection of Dr Jeffrey S. Upperman; used with permission [Citation ends].
Meta-analyses suggest that open and laparoscopic approaches may be similarly safe and effective.[60][61][62][63][64] In a 2017 meta-analysis, comparable rates of post-operative complications were reported, with total complication rates of 9.2% (28/303) and 10.4% (31/297) for laparoscopy and open surgery, respectively (P=0.74).[62]
One 2021 meta-analysis concluded that the laparoscopic approach may result in a small increase in mucosal perforation (relative risk [RR] 1.60, 95% confidence interval [CI] 0.49 to 5.26), and an increased risk of incomplete pyloromyotomy (RR 7.37, 95% CI 0.92 to 59.11) compared with the open approach, but there is a low certainty of evidence and both effect estimates include the possibility of no difference.[63] This meta-analysis also reported that the certainty of evidence relating to the need for re-operation, post-operative wound infections or abscess formation, post-operative haematoma or seroma formation, incisional hernia occurrence, length of post-operative stay, time to full feeds, and operating time was very low, so reliable conclusions about these outcomes could not be made.[63]
In one randomised controlled trial, infants treated laparoscopically had improved postoperative pain control and better cosmetic appearance.[65] Laparoscopic pyloromyotomy was associated with shorter post-operative recovery time and fewer analgesia requirements than open pyloromyotomy in one large, multicentre international trial.[66]
In centres where laparoscopic surgery is readily performed, it may be the preferred approach.
As most infants with pyloric stenosis are otherwise healthy, there is no preference to perform open versus laparoscopic pyloromyotomy in different patient subsets based on comorbidities.
One study of the long-term effects of pyloromyotomy concluded that most patients operated on for pyloric stenosis during infancy in the 1970s have experienced no adverse effects into adulthood.[67]
Other treatments
Atropine treatment and endoscopic balloon dilatation should only be considered and performed in specialised centres and under very special circumstances (e.g., if an infant has an intractable condition that precludes surgery). Results may be suboptimal and there is an increased risk of complications.
Atropine given orally and/or intravenously may lead to resolution of the condition based on ability to tolerate feedings and normalisation of ultrasound measurements.[68] The overall success rate is 85% versus 100% for pyloromyotomy and the average hospital stay is significantly longer for medical treatment (13 days vs. 5 days).[69] One subsequent study reported a 25% failure rate for non-operative management.[70]
Endoscopic balloon dilatation is seldom used. There is a high rate of perforation and unsuccessful dilatation with this procedure.[71]
Use of this content is subject to our disclaimer