Differentials
Common
Vaginitis and vulvovaginitis
History
burning sensation with coitus, vulvar/vaginal oedema, vaginal discharge, pruritus
Exam
erythematous and oedematous vaginal/vulvar mucosa; vaginal discharge (thick and adherent for Candida infection, frothy for trichomoniasis); strawberry cervix suggests trichomoniasis
1st investigation
Other investigations
- trichomonal and candidal culture:
positive
More
Herpes simplex infection
History
intense vulvar pain; dysuria; burning; pruritus; fever and general malaise with primary infection
Exam
primary outbreak: lesions may coalesce and be diffuse, and accompanied by inguinal lymphadenopathy; recurrent outbreak: discrete vesicular lesions
1st investigation
- HSV polymerase chain reaction (PCR) or other nucleic acid amplification test (NAAT):
positive
More
Other investigations
- viral culture:
virus detected
More
Vaginal atrophy
History
vaginal dryness; feeling of tearing during intercourse, post-coital burning, vaginal spotting if small lacerations are present
Exam
vaginal mucosa is pale and lacks rugation, may have evidence of small lacerations
1st investigation
- none:
diagnosis is clinical
Other investigations
Iatrogenic
History
difficulty with penetration, onset of pain after medication use or radiotherapy initiated, and history of therapy with radiation, combined oral contraceptives, antidepressants, or some antihypertensives
Exam
vaginal mucosa is dry
1st investigation
- none:
diagnosis is clinical
Other investigations
Primary inadequate lubrication
History
difficulty with penetration, pain at the onset of sexual activity, possible difficulty with arousal due to relationship difficulties and possible history of sexual abuse
Exam
vaginal mucosa is dry
1st investigation
- none:
diagnosis is clinical
Other investigations
Vestibulodynia/vulvodynia
History
pain with tampon insertion or removal; pain with manual stimulation; painful gynaecological examination
Exam
intense pain in the vestibule upon direct palpation with a cotton bud; mucosa may be normal-appearing or erythematous[31]
1st investigation
- wet prep and potassium hydroxide:
negative
More
Other investigations
- trichomonal and candidal cultures:
negative
More
Endometriosis
History
typically presents with deep thrust dyspareunia; may also include significant dysmenorrhoea, and/or pain between menses; pain with defecation can occur (dyschezia); symptoms may progress over time
Exam
cul-de-sac nodularity; uterosacral ligament thickening, tenderness, or nodularity; a fixed and retroverted uterus; lateral cervical deviation due to tethering of the uterosacral ligament
1st investigation
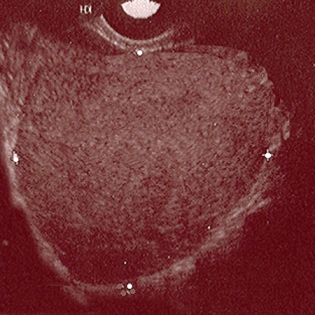
- pelvic ultrasound:
may show ovarian endometrioma (homogenous low-level echoes) or evidence of deep pelvic endometriosis such as uterosacral ligament involvement (hypoechoic linear thickening)
More
Other investigations
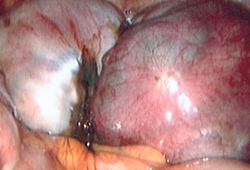
- diagnostic laparoscopy:
direct visualisation with biopsy: confirmed endometrial glands or stroma outside uterine cavity
More
Adenomyosis
History
deep thrust dyspareunia; progressive dysmenorrhoea and menorrhagia; parous; onset after childbirth
Exam
tender, slightly enlarged uterus in the absence of signs of infection
1st investigation
- pelvic ultrasound:
enlarged uterus with heterogeneous texture, no well-defined masses
Other investigations
- pelvic MRI:
hyperintense myometrial foci on T2-weighted images
- endometrial biopsy:
negative
More
Leiomyomas
History
deep thrust dyspareunia; achy pain; progressive dysmenorrhoea and menorrhagia
Exam
tender, enlarged, irregular uterus, no signs of infection
1st investigation
- pelvic ultrasound:
enlarged uterus with discrete masses
Other investigations
- pelvic MRI:
discrete masses
More
Uncommon
Interstitial cystitis
History
dyspareunia, urinary frequency and urgency, chronic pelvic pain
Exam
intolerance of pelvic examination, extreme tenderness over the anterior vaginal wall
1st investigation
Other investigations
- urine cytology:
negative
More
Urinary tract infection
History
urinary frequency and urgency; dysuria; haematuria may be reported
Exam
may be normal
1st investigation
- urinalysis:
positive for leukocyte esterase, nitrites, and/or WBC and blood
- urine microscopy and culture:
growth of >10⁵ colony-forming units per mL (CFU/mL)
More
Other investigations
Bartholin's gland abscess
History
vulvar lump; intense pain and tenderness with toileting, intercourse, or movement
Exam
Bartholin's gland is found at the junction of the vulva and vagina at 4 or 8 o'clock position; abscess will be firm and tender, purulent drainage may also be noted; overlying cellulitis is common
1st investigation
- none:
diagnosis is clinical
Other investigations
Seminal plasma hypersensitivity
History
post-coital pruritus, burning, swelling, possible systemic response (angio-oedema of face, throat, lips)[28]
Exam
post-coital erythema and oedema of vulvar/vaginal mucosa, possible blistering
1st investigation
- allergen avoidance:
resolution of symptoms
More
Other investigations
- allergy testing:
positive
More
Contact dermatitis
Atopic dermatitis
Bartholin's gland mass
History
vulvar lump with little or no associated pain
Exam
Bartholin's gland cyst will be a smooth, mobile mass at the junction of the vulva and vagina at 4 or 8 o'clock position
1st investigation
- none:
diagnosis is clinical
Other investigations
Imperforate hymen
History
cyclic pelvic pain, amenorrhoea, oligomenorrhoea, difficulty with tampon/penis insertion
Exam
thin to moderately thick membrane at the opening of the vagina, may or may not have small perforations allowing the passage of menstrual flow; if no small perforations, haematocolpos may be present
1st investigation
- none:
diagnosis is clinical
More
Other investigations
Traumatic perineal injuries
History
pain began after childbirth or other trauma (e.g., sexual assault, female genital mutilation/cutting); may have history of episiotomy, advanced obstetric laceration
Exam
pain on palpation of the scar
1st investigation
- none:
diagnosis is clinical
Other investigations
Vulvar dystrophies
History
external pruritus; vulvar soreness and irritation; post-coital burning; postcoital spotting
Exam
vulvar skin can be thickened from hypertrophy or thinned, lesions can be diffuse or patchy, fissuring from itching can be present
1st investigation
- vulvar biopsy:
whitened epithelium
More
Other investigations
Vaginismus
History
inability to allow penetration of objects vaginally; often begins after episode of penetration (speculum examination, intercourse)
Exam
pelvic examination should be deferred in suspected vaginismus until appropriate rapport is developed; examination may be normal, or may demonstrate varying degrees of difficulty with insertion of either the speculum or examining fingers due to muscle spasm and contraction; levator ani spasm may occur during the examination, as a response to the anticipated pain
1st investigation
- none:
diagnosis is clinical
Other investigations
Psychosexual disorder
History
may be accompanied by difficulties with interpersonal relationships or arousal, or mood disturbances such as depression and anxiety; possible history of sexual abuse; sudden onset of symptoms
Exam
normal pelvic examination if no acute abuse or assault episodes
1st investigation
- none:
diagnosis is clinical
More
Other investigations
Cervicitis
History
deep thrust dyspareunia, vaginal discharge
Exam
mucopurulent cervical discharge, cervical motion tenderness, friable and erythematous cervix
1st investigation
- cervical NAAT for Neisseria gonorrhoeae, Chlamydia trachomatis, Mycoplasma genitalium:
positive
Pelvic inflammatory disease
History
deep thrust dyspareunia; fever, diffuse lower abdominal pain; high-risk sexual behaviour; abnormal uterine bleeding, vaginal discharge
Exam
cervical motion tenderness; uterine tenderness; adnexal tenderness; purulent cervical discharge
1st investigation
Hydrosalpinx
History
history of PID
Exam
adnexal tenderness on pelvic exam, palpable adnexal mass
1st investigation
- pelvic ultrasound:
tubal mass
Other investigations
Levator ani spasm
History
pain on penetration; spasm-type pain; sensation of something pushing outwards from the inside
Exam
distinct levator ani spasm and/or pain during bimanual exam
1st investigation
- none:
diagnosis is clinical
Other investigations
Use of this content is subject to our disclaimer