Approach
A complete gynaecological history, including sexual history as well as any history of abuse, and pelvic examination are the key components in the approach to a patient with dyspareunia.[9] Frequently, the history and physical examination are sufficient to diagnose the underlying aetiology. However, the overlap between physical, psychological, and social factors can often make it difficult to identify the primary underlying cause.[9]
Historical considerations
In addition to the features listed below, the practitioner must be attuned to the possibility that some women will not voluntarily report difficulties with sexual relations.[9][10] The use of open-ended questions, such as 'Are you sexually active?', and if so, 'Are you having any sexual difficulties or problems at this time?' can open the door of communication about sexual dysfunction.[9][10]
Onset of symptoms: symptoms of primary dyspareunia begin with the first sexual encounter and persist, and may indicate a congenital anomaly or psychosexual condition.
Location of symptoms: pain on penetration is a symptom of superficial dyspareunia, suggestive of a disorder of the vulva or vestibule. Discomfort during deep penetration, with no difficulty during initial penetration, is associated with deep dyspareunia, possibly indicating a pelvic pathology.
Associated symptoms: presence of pruritus may indicate eczema or vulvar dystrophy. Pruritus accompanied by discharge may indicate vulvovaginitis. Deep thrust dyspareunia accompanied by dysmenorrhoea 2 to 3 days before and during menses, and sometimes associated with pain during defecation (dyschezia), may suggest endometriosis.
Quality of pain: sharp pains associated with deep dyspareunia may indicate endometriosis, whereas achy pain may represent leiomyomata. A sensation of tearing may suggest vaginal atrophy, due to a variety of conditions.
Alleviating factors: pain that has improved with oral contraceptives may indicate endometriosis or adenomyosis. Oestrogen therapy improves atrophy related to oestrogen deficiency, whereas topical lubricants may improve vaginal dryness caused by drugs or treatments.
Medical history: a history of cancer that required chemotherapy or pelvic radiotherapy may have resulted in atrophy due to oestrogen deficiency, fibrosis, or adhesions. Medications for other chronic illnesses may result in decreased lubrication (e.g., oral contraceptives, antidepressants, some antihypertensives).
Obstetric history: traumatic birth injuries or episiotomies can result in dyspareunia.
Of note, symptoms consistent with superficial dyspareunia related to levator ani spasm and vaginismus will be found in association with many of the other conditions, as women instinctively tense these muscles in anticipation of discomfort.
Psychosexual evaluation
May be considered, particularly if the patient describes sudden onset of symptoms.[9] An open consultation style may help to identify psychological causes; the 'LOFTI' (listening, observing, feelings, thinking, interpreting) psychosexual assessment can be a useful guide.[9][11]
Physical examination
Careful inspection enables diagnosis of dermatological and infectious/inflammatory conditions of the vulva and vestibule. A thin to moderately thick membrane at the opening of the vagina, with or without small perforations, points towards imperforate hymen (potentially with accumulation of menstrual blood in the vagina [haematocolpos]).
Careful examination of the vulva with a cotton swab may lead to the diagnosis of vestibulodynia/vulvodynia if light pressure reproduces the pain.[12]
Pale vaginal mucosa that lacks rugation is characteristic of vaginal atrophy due to oestrogen deficiency.
Mucopurulent cervical discharge accompanied by cervical motion tenderness may be suggestive of cervicitis. The presence of uterine tenderness may indicate pelvic inflammatory disease (PID).
On bimanual examination, an enlarged, smooth, tender uterus may indicate adenomyosis, whereas an enlarged, irregular uterus is indicative of leiomyomata. Examination findings consistent with endometriosis include rectovaginal nodularity; shortening and/or thickening of the uterosacral ligaments; a fixed, retroverted uterus; and reproduction of pain on palpation of suspected endometriosis lesions. The presence of an adnexal mass on pelvic exam may suggest endometrioma or hydrosalpinx.[Figure caption and citation for the preceding image starts]: Bulging, bluish imperforate hymen with haematocolposBMJ Case Reports 2009 [doi:10.1136/bcr.08.2008.0722] Copyright © 2009 by the BMJ Publishing Group Ltd. [Citation ends].
 [Figure caption and citation for the preceding image starts]: Cervicitis and vaginal discharge due to gonorrhoeaCDC Image Library [Citation ends].
[Figure caption and citation for the preceding image starts]: Cervicitis and vaginal discharge due to gonorrhoeaCDC Image Library [Citation ends]. [Figure caption and citation for the preceding image starts]: Cervicitis due to Herpes simplex virus; erosive inflammation with accompanying paracervical purulency is seenCDC Image Library / Dr Paul Wiesner [Citation ends].
[Figure caption and citation for the preceding image starts]: Cervicitis due to Herpes simplex virus; erosive inflammation with accompanying paracervical purulency is seenCDC Image Library / Dr Paul Wiesner [Citation ends]. [Figure caption and citation for the preceding image starts]: Trichomonas vaginitis with copious purulent discharge emanating from the cervical osCDC Image Library [Citation ends].
[Figure caption and citation for the preceding image starts]: Trichomonas vaginitis with copious purulent discharge emanating from the cervical osCDC Image Library [Citation ends].
Laboratory evaluation and imaging studies
In many cases of dyspareunia, laboratory and imaging studies will not be required to make the diagnosis. However, they are essential in certain situations.
Vaginal samples for vaginal pH and amine ('whiff') test, and for normal saline and potassium hydroxide slides, will aid in the identification of organisms responsible for vulvovaginitis. Gram stain for bacterial vaginosis and genital cultures for trichomonads and Candida may be useful in women with vulvovaginal symptoms (e.g., burning sensation with coitus, vaginal discharge, pruritus), but negative wet prep slides.
Nucleic acid amplification testing (NAAT) of genital samples for gonorrhoea and Chlamydia is more sensitive than culture and recommended as first-line method of testing in suspected PID. Mycoplasma genitalium is associated with PID and cervicitis; guidelines recommend NAAT of genital samples.[13][14]
Cervical cultures for gonorrhoea and Chlamydia should be taken when there is a clinical suspicion for cervicitis (e.g., history of deep thrust dyspareunia and vaginal discharge) or PID (e.g., history of deep thrust dyspareunia, fever, diffuse lower abdominal pain).
Herpes simplex virus polymerase chain reaction (PCR) or other NAAT should be ordered when investigating herpes simplex virus infection. Tzanck smear may be used as an alternative diagnostic test if PCR is not readily available.[15][16] Viral culture may be considered if NAATs are not available.[15]
Urinalysis is essential if urinary tract infection (UTI) is suspected (e.g., urinary frequency and urgency, dysuria, haematuria). Urine microscopy and culture is indicated when investigating UTI or interstitial cystitis.
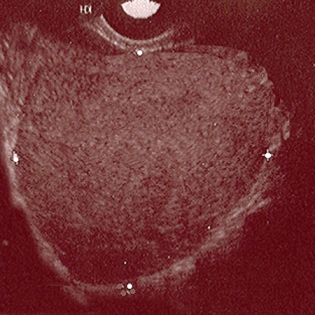
Pelvic ultrasound can be useful in characterising leiomyomata and evaluating adnexal masses suspicious for endometriomas, or for hydrosalpinx.[17][18][19] During transvaginal ultrasound, localisation of painful areas (site-specific tenderness) is possible.[20][21][22] Magnetic resonance imaging (MRI) can be more useful when congenital structural abnormalities are suspected (e.g., adenomyosis is visualised as hyperintense myometrial foci on T2-weighted images), or to diagnose deep endometriosis and assess its extent.[17][23][24][25]
Diagnostic laparoscopy may be useful if endometriosis is suspected (e.g., deep thrust dyspareunia, significant dysmenorrhoea), even if the ultrasound scan or MRI scan was normal.[17]
Cystoscopy should be ordered initially in all patients with a suspected diagnosis of interstitial cystitis (e.g., urinary frequency and urgency, chronic pelvic pain, intolerance of pelvic exam). In addition, patients at high risk of bladder cancer (smokers, women exposed to aniline dyes) should have urine cytology.
Patients with suspected seminal plasma hypersensitivity (e.g., postcoital pruritus, burning), contact dermatitis (e.g., history of allergic response to latex or spermicidal agent), or atopic dermatitis (e.g., pruritus, dry scaly skin) may demonstrate resolution of symptoms following allergen avoidance. However, should this not occur or the allergen be difficult to identify, allergy testing is recommended.
Vulvar/vaginal biopsies should always be done for suspicious lesions and skin changes of unclear aetiology, to exclude precancerous or cancerous conditions.[Figure caption and citation for the preceding image starts]: Ultrasound of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Laparoscopic image of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Laparoscopic image of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].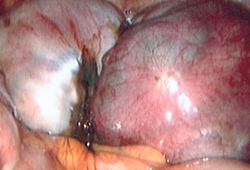
Use of this content is subject to our disclaimer