Differentials
Common
Pneumothorax
History
sudden onset of dyspnoea and/or pleuritic chest pain; more common in patients with asthma or COPD, or those using positive pressure ventilation
Exam
sudden deterioration in gas exchange and BP; decreased breath sounds with increased resonance on percussion; deviation of trachea away from affected side indicates a tension pneumothorax
1st investigation
- chest x-ray:
evidence of a pleural line beyond which no parenchymal or vascular markings can be seen
More
Other investigations
- CT scan chest:
visceral pleural line easily identified
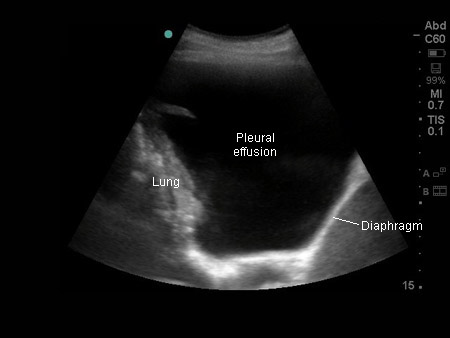
More - thoracic ultrasound scan:
absent lung sliding
Bacterial pneumonia
History
fever, cough, purulent sputum production, rhinorrhoea
Exam
reduced breath sounds on auscultation if effusion present; dullness to percussion; increased vocal fremitus over consolidated lung (decreased over effusion); egophony; crackles may be evident in areas of effusion with nearby parenchymal consolidation; friction rub may be heard
1st investigation
Other investigations
- FBC:
elevated WBC count with leftward shift (polymorphonuclear cell predominance or band forms)
- CRP:
elevated
- blood cultures:
positive growth of offending organism
More - sputum cultures:
positive growth of offending organism
More - thoracocentesis:
exudative effusion; pleural fluid cultures may show growth of the offending organism (empyema)
Pulmonary embolism
History
sudden onset of chest pain; history of prolonged immobility; prolonged travel by plane or automobile; hypercoagulable syndromes; recent leg trauma; history of malignancy; history of prior deep vein thrombosis (DVT) or pulmonary embolism; recent surgery; haemoptysis, dyspnoea, pleuritic pain; can be asymptomatic
Exam
tachypnoea; haemoptysis; syncope; tachycardia; hypotension; jugular venous distention; pleural rub; examination may be normal
1st investigation
Other investigations
- V/Q scan:
presence of one or more segmental or subsegmental defects in perfusion in corresponding areas of normal ventilation[57]
More - Doppler ultrasound of lower extremity:
deep veins above the popliteal fossa that are non-compressible due to clot and without flow augmentation with compression on Doppler analysis[57]
More
Non-mesothelioma malignancy
History
primary lung, breast, gastrointestinal, or genitourinary cancer; lymphoma; constitutional symptoms such as malaise, weight loss, anorexia
Exam
specific to the primary malignancy
1st investigation
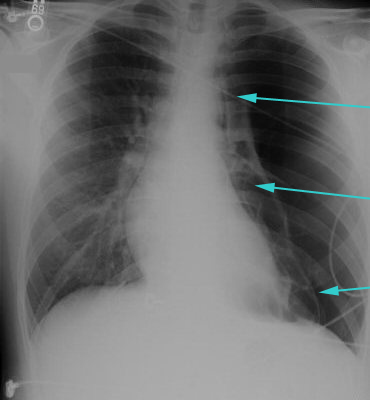
- chest x-ray:
may see primary or metastatic lung lesions; pleural effusion
More
Acute coronary syndrome
History
central chest pressure, squeezing, or heaviness; radiation to jaw or upper extremities; associated nausea, vomiting, dyspnoea, dizziness, weakness; occurs at rest or accelerating tempo (crescendo); risk factors: smoking, age (men >45 years, women >55 years), positive family history of premature coronary artery disease, hypertension, hyperlipidaemia, diabetes, stroke, or peripheral arterial disease
Exam
jugular venous distention, S4 gallop, holosystolic murmur (mitral regurgitation), bibasilar crackles; hypotensive, tachycardic, bradycardic, or hypoxic depending on severity of ischaemia
1st investigation
- ECG:
ST-elevation myocardial infarction (STEMI): ST segment elevation of >1 mm in ≥2 anatomically contiguous leads or new left bundle branch block; non-ST elevation myocardial infarction (NSTEMI) or unstable angina: non-specific; ST segment depression or T wave inversion
More - chest x-ray:
normal or signs of heart failure, such as increased alveolar markings
More - cardiac enzymes:
elevated in STEMI and NSTEMI; not elevated in unstable angina
More
Viral pleuritis
History
prodrome of viral illness (myalgias, malaise, rhinorrhoea, cough, nasal congestion, low-grade temperatures); sick contacts
Exam
pleural friction rub with or without low-grade fever; sometimes reproducible tenderness to palpation of chest when perichondritis or pleurodynia accompanies pleuritis
1st investigation
- chest x-ray:
usually normal but can uncommonly have effusion
More
Other investigations
- FBC:
normal, or leukocytosis with lymphocytic predominance
- CRP:
may be normal or elevated
- viral culture:
detection of virus or viral antigen
More
Uncommon
Asbestos-related benign pleural disease
History
history of exposure to asbestos; occupation in construction or ship building or repair
Exam
no specific findings distinguish asbestos-related pleural disease such as benign asbestos pleural effusion from other forms of pleural disease
1st investigation
- chest x-ray:
pleural plaques, effusion, pleural thickening
Other investigations
- thoracocentesis:
exudative effusion
Mesothelioma
History
may be a history of exposure to asbestos; chest pain; cough; dyspnoea; weight loss; fatigue; fevers and sweats
Exam
unilateral dullness to percussion at the lung base; may be palpable lymph nodes; palpable chest wall masses
1st investigation
- chest x-ray:
pleural based mass; unilateral pleural effusion; irregular pleural thickening
Other investigations
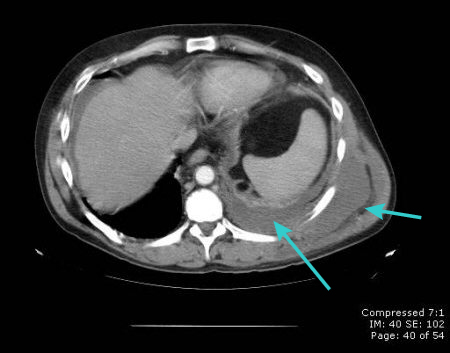
- CT scan chest:
irregular thickening of pleura; pleural effusion
More - thoracocentesis + pleural biopsy:
exudative effusion; malignant cells on cytology and histology; elevated mesothelin levels
More - immunohistochemistry:
positive results for certain markers (e.g., calretinin, keratins 5/6, and nuclear WT1) make mesothelioma more likely, while positive results for other markers (e.g., carcinoembryonic antigen [CEA] epithelial cell adhesion molecule [EPCAM], claudin 4, thyroid transcription factor [TTF-1]) make mesothelioma less likely
More
Pulmonary/extrapulmonary tuberculosis (TB)
History
TB infection in past; contact with patients with active TB; history of time spent in shelters or incarceration; origin in area of endemic TB; chronic cough with sputum production; fevers; night sweats; weight loss; failure to thrive; history of purified protein derivative (PPD; tuberculin) positivity
Exam
dullness to percussion; diminished breath sounds in area of effusion; rarely, directly draining sinus tract of empyema necessitans (chronic untreated empyema that has eroded through the thoracic cage and formed a subcutaneous abscess)
1st investigation
- chest x-ray:
may demonstrate atelectasis from airway compression, pleural effusion, consolidation, pulmonary infiltrates, mediastinal or hilar lymphadenopathy, upper zone fibrosis
More - sputum acid-fast bacilli smear and culture:
presence of acid-fast bacilli (Ziehl-Neelsen stain) in specimen
More - acid-fast bacilli smear and culture of extrapulmonary biopsy specimen:
positive
More - nucleic acid amplification (NAAT):
positive for M tuberculosis
More
Other investigations
- bronchoscopy and bronchoalveolar lavage:
positive for acid-fast bacilli
More - lateral flow urine lipoarabinomannan (LF-LAM) assay:
positive
More - contrast-enhanced chest computed tomography scan:
primary TB: mediastinal tuberculous lymphadenitis with central node attenuation and peripheral enhancement, delineated cavities; post-primary TB: centrilobular nodules and tree-in-bud pattern; effusion sometimes seen
More - thoracocentesis:
exudative effusion with lymphocytic predominance
More
Connective tissue disorders
History
prior diagnosis of connective tissue disease; arthritis; joint deformities; rash; alopecia; dry eyes or mouth
Exam
malar rash; alopecia; joint tenderness; tenderness to muscle palpation (systemic lupus erythematosus [SLE]); joint deformities; synovitis (rheumatoid arthritis); dry mucous membranes (Sjogren syndrome)
1st investigation
- chest x-ray:
pleural effusion
Other investigations
- thoracocentesis:
for rheumatoid pleuritis, effusions are exudative with low glucose <60 mg/dL (<3.33 millimol/L), low pH, and high LDH >1000 IU/L;[69] pleural effusions of SLE are exudative with higher glucose and lower LDH than those associated with rheumatoid arthritis[70]
- specific serological disease markers:
positive
More
Drug reactions
History
recent use of hydralazine, procainamide, isoniazid, methyldopa, or chlorpromazine (lupus pleuritis); use of minoxidil, beta-blockers, amiodarone, bleomycin, methysergide, methotrexate, cyclophosphamide, valproic acid, phenytoin, or nitrofurantoin
Exam
non-specific; essentially those signs seen with any pleural effusion (dullness to percussion over area of effusion, diminished breath sounds in the same distribution)
1st investigation
- chest x-ray:
pleural thickening; pleural effusion
Other investigations
- thoracocentesis:
eosinophils constituting >10% of cells in pleural fluid can be found in drug reactions[20]
Aortic dissection
History
acute substernal tearing sensation, with radiation to interscapular region of the back; pain may migrate with the propagation of the dissection; stroke, acute myocardial infarction due to obstruction of aortic branches; dyspnoea due to acute aortic regurgitation; history of hypertension, Marfan syndrome, Ehlers-Danlos syndrome, or syphilis
Exam
unequal pulses or BPs in both arms, hypotension due to cardiac tamponade; new diastolic murmur due to aortic regurgitation; muffled heart sounds if the dissection is complicated by cardiac tamponade; new focal neurological findings due to involvement of the carotid or vertebral arteries
1st investigation
Post-cardiac injury syndrome (PCIS)
History
fever and chest pain within 2 to 3 weeks after myocardial infarction (MI), or from 3 days to 1 year after coronary artery bypass surgery; chest pains usually precede fever and can vary from dull ache to pleuritic sharp pain or even agonising crushing chest pain mimicking MI
Exam
pericardial friction rub; approximately 80% will have accompanying pleural effusions (dullness to percussion and decreased breath sounds at the lung bases)
1st investigation
- FBC:
peripheral leukocytosis
- erythrocyte sedimentation rate:
elevated (often in excess of 100 mm/hour)[73]
Other investigations
- chest x-ray:
occasionally double density sign; pleural effusions in 80% of cases, usually bilateral (50% of the time); left-sided effusion when unilateral[73]
More - thoracocentesis:
exudate with normal pH and normal glucose; bloody in 30% of patients; differential cell count may reveal polymorphonuclear leukocyte predominance or mononuclear cell predominance, depending on acuity[74]
More
Uraemia
History
known renal impairment, malaise, itch
Exam
sallow skin, confusion; examination may be normal
1st investigation
- basic metabolic profile (including urea and creatinine):
elevated serum creatinine and urea, high serum potassium, metabolic acidosis
Other investigations
- thoracocentesis:
transudative effusion
Cirrhosis
History
history of alcohol misuse, intravenous drug use, unprotected sexual intercourse, obesity, blood transfusion, known hepatitis infection; fatigue, weakness, weight loss, or pruritus
Exam
may include oedema, jaundice, ascites, collateral circulation with distended abdominal veins (caput medusae), hepatosplenomegaly, leukonychia, palmar erythema, spider angiomata (spider naevi), telangiectasia, jaundiced sclerae, hepatic foetor, altered mental status
1st investigation
- serum ALT and AST:
elevated with ALT:AST ratio ≥1 if hepatocellular damage; normal in cholestasis
- serum alkaline phosphatase and gamma-GT:
elevated in cholestasis
- serum sodium:
commonly reduced in patients with associated ascites
- serum albumin:
reduced
- platelet count:
reduced (platelet count <150,000 mm³)
- prothrombin time:
prolonged
Other investigations
- thoracocentesis:
transudative effusion
- abdominal paracentesis:
transudative ascitic fluid
- abdominal ultrasound:
liver surface nodularity, small liver, possible hypertrophy of left/caudate lobe, ascites, splenomegaly, increased diameter of the portal vein (≥13 mm), or collateral vessels
Acute pancreatitis
History
pleuritis occurs in patients with severe acute illness associated with liver failure and/or renal failure, especially those who require multiple blood transfusions; risk factors: middle-aged women, young-to-middle-aged men, gallstones, high alcohol consumption, hypertriglyceridaemia, drugs, endoscopic retrograde cholangiopancreatography procedure, HIV/AIDS, SLE, and Sjogren syndrome; nausea, vomiting, anorexia, epigastric pain
Exam
Grey-Turner sign, Cullen's sign, Fox's sign, Chvostek's sign, Trousseau's sign, tachycardia, hypotension, abdominal distention
1st investigation
- serum lipase or amylase:
elevated (3 times the upper limit of the normal)
More
Other investigations
- abdominal ultrasound:
may see ascites, gallstones, dilated common bile duct, and enlarged pancreas
More - CT scan of abdomen with oral and intravenous (IV) contrast:
may show pancreatic inflammation, peri-pancreatic stranding, calcifications, or fluid collections; confirms or excludes gallstones
More - MRI/magnetic resonance cholangiopancreatography (MRCP):
findings may include stones, tumours, diffuse or segmental enlargement of the pancreas with irregular contour and obliteration of the peri-pancreatic fat, necrosis, or pseudocysts
More
Chronic pancreatitis
History
history of alcohol misuse, nausea, vomiting, epigastric abdominal pain radiating to the back, steatorrhoea, malnutrition, diabetes mellitus
Exam
weight loss, jaundice
1st investigation
- abdominal CT scan:
pancreatic calcifications, focal or diffuse enlargement of the pancreas, ductal dilatation, and/or vascular complications
Other investigations
Use of this content is subject to our disclaimer



 ]
]