Aetiology
The pleura and the pleural space are affected by a variety of systemic disease processes as well as local diseases affecting the lung.[3] Some rarer causes arise from the pleural space itself.
Pulmonary
Two-thirds of pleural infections arise from underlying lung infections or penetrating thoracic trauma. Other sources of pleural infections are vascular dissemination or extension from an intra-abdominal source.[4]
Pneumothorax: when the pleural space is disrupted air collects between the parietal and visceral pleura. This is seen as a pleural line beyond which no parenchymal markings are visible on a chest radiograph. When this occurs in the setting of accompanying pleural fluid (a hydropneumothorax), the fluid exposed to air will often have increased eosinophils as a result.
Viral: coxsackie B virus is a common cause of infectious pleuritis.[3] Echovirus can cause the syndrome Bornholm pleurodynia, manifesting as pleuritis, fever, and chest muscle spasms; the condition occurs in the late summer and affects adolescents and young adults. Other viral aetiologies are influenza, parainfluenzae, respiratory syncytial virus, COVID-19, and cytomegalovirus.
Bacterial: Streptococcus species, Staphylococcus aureus, enteric gram-negative bacilli, and anaerobes are the principal organisms causing pleural infections. They invariably result in the formation of empyema if not promptly drained.[5]
Pulmonary embolism: when an effusion develops because of nearby lung infarction, the fluid is typically sanguineous or serosanguineous and may have predominance of neutrophils or eosinophils.[6][7]
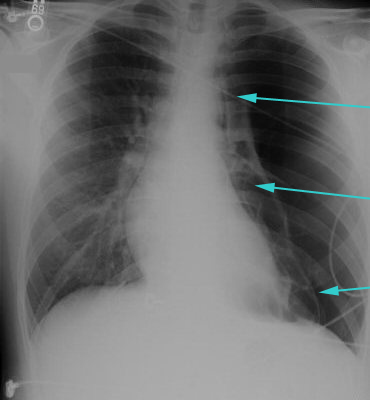
Asbestos-related benign pleural disease: asbestos exposure can result in parietal pleural plaques or diffuse pleural thickening, usually many (>18) years after exposure. Benign asbestos pleural effusions, however, can occur as early as 1 year after exposure and are exudative with elevated eosinophils.[8] These usually self-remit but may do so slowly over many months. Initial presentation is usually with dyspnoea on exertion. Rarely patients can present with pleuritic chest pain.[9][Figure caption and citation for the preceding image starts]: Large left pneumothorax with visible pleural line and absence of lung markings beyond the lineFrom the collection of Dr Ami Rubinowitz; used with permission [Citation ends].
Systemic
Infection: tuberculous pleuritis is the most common form of extrapulmonary tuberculosis (TB) infection.[10] It is uncommon in the US, but is increasingly prevalent worldwide.[11] A definitive diagnosis of TB pleuritis can only be confirmed by identification of Mycobacterium tuberculosis by microscopy; culture of sputum, pleural fluid, or pleural biopsy specimens; or nucleic acid amplification tests (NAATs).[12][13][14] Unfortunately, acid-fast smears and culture of sputum samples have poor sensitivity in patients with pleural TB.[15][16] NAATs should be performed on at least one respiratory specimen, or specimen collected from sites of suspected extrapulmonary TB, when a diagnosis of TB is being considered.[14][17] The pleural fluid biomarker, adenosine deaminase, has a high sensitivity and specificity for the identification of pleural TB (92% and 90%, respectively), and could facilitate prompt initiation of treatment in areas of high TB prevalence.[12]
Malignancy: primary lung cancer, mesothelioma (as a result of asbestos exposure), or metastasis from lung, breast, lymphoma, gastrointestinal, or genitourinary tumours.[18]
Connective tissue disorders: a major cause of autoimmune pleuritis. The most common connective tissue disorders are systemic lupus erythematosus, rheumatoid arthritis, and Sjogren syndrome. In one retrospective review, 8.5% of patients with non-specific pleuritis on thoracoscopic biopsy were diagnosed with Sjogren syndrome.[19]
Drug reactions: drugs such as hydralazine, procainamide, isoniazid, methyldopa, or chlorpromazine are associated with development of lupus pleuritis. Other drugs such as minoxidil, beta-blockers, amiodarone, bleomycin, methysergide, methotrexate, cyclophosphamide, valproic acid, or nitrofurantoin also cause pleuritis through unclear mechanisms.[20] Pneumotox: drug-induced respiratory diseases Opens in new window
Other conditions that may cause pleuritis, although it is rarely the primary presenting symptom, include uraemia, familial Mediterranean fever, and other intra-abdominal processes such as cirrhosis or pancreatitis.[21][22][23]
Cardiovascular
Post-cardiac injury syndrome: an autoimmune inflammatory process involving pleura and pericardium secondary to cardiac injury (either acute coronary syndrome or cardiac surgery/trauma).[24]
Aortic dissection: rare cause of pleuritis and is due to blood leaking into the pleural space.
Use of this content is subject to our disclaimer