Aetiology
Aetiology is not completely understood; several factors may be involved:
Ultraviolet radiation (UVR) exposure: UVR, both from natural sunlight and from artificial sources (sun-tanning beds or medical phototherapy units), is the main trigger, causing activation of the immune system (contrary to UVR-induced immunosuppression that occurs in people unaffected with PLE).[24] The exact mechanism of action remains under debate, but UV-A appears more heavily implicated. Approximately 75% of patients develop PLE after UV-A exposure, compared with 10% after UV-B exposure, and 15% after exposure to both spectra.[6][25][26][27][28]
Oxidative stress: UV-A exposure in the skin generates free radicals (reactive oxygen species), for example, the singlet oxygen. The alteration of the redox status of the skin may play a key role in the manifestation of PLE.[29][30][31]
Photosensitiser: as the clinical picture of PLE shows features of a delayed immune reaction, the influence of an endogenous or exogenous photo-allergen has been implicated; however, its exact nature remains elusive.[32]
Family history of PLE: although no candidate genes have been characterised, a positive family history can be found in up to 50% of the cases.[17] Twin studies indicate that there is a strong inherited component, but more work must be done to characterise the specific gene, or genes.[15] Regulatory T cell dysfunction is implicated in the pathophysiology of PLE, and this is likely to be via pathways regulated by factors other than vitamin D.[33][34]
Female sex: as women are more commonly affected by PLE, the influence of oestrogens has been considered. There is a reduction in severity of PLE symptoms subsequent to the menopause, suggesting that 17 beta-oestradiol might play a role.[1][20][35] It has been shown that oestrogens can inhibit the release of interleukin-10 (IL-10) from keratinocytes, thus allowing aberrant inflammatory reactions such as in PLE to occur.[36]
There is one case report of association with common variable immunodeficiency syndrome.[37]
Physiological reactions of the skin to UVR exposure, such as development of erythema and pigmentation, are typically normal in PLE patients, with average values for minimal erythema doses and minimal pigmentation doses, according to skin type.[38][39]
Pathophysiology
The pathogenesis of PLE may be based on a failure of ultraviolet radiation (UVR)-induced immunosuppression, which could result in an abnormal response to photo-induced antigens.[40] This is shown by the persistence of Langerhans cells within the epidermis after UVR exposure, leading to reduced immune tolerance and also, interestingly, reduced rates of skin cancer.[41]
Studies have investigated the role of the skin microbiome in the pathogenesis of PLE. A theory has been suggested for UVR-induced alteration of antimicrobial peptides (AMPs) as the potential source of antigens that lead to keratinocyte apoptosis in PLE; an increased expression of psoriasin and ribonuclease 7 (RNase7, mostly in stratum granulosum of the epidermis), human beta-defensin 2 (HBD-2) and cathelicidin (LL37) in PLE lesional skin has been described.[42]
Ultraviolet A (UV-A) irradiation leads to increased oxidative stress and induction of pro-inflammatory molecules, such as the interleukins IL-1-alpha, IL-6, and IL-8, and intercellular adhesion molecule-1 (ICAM-1).[40][43][44] Up-regulation of ICAM-1 is regulated by the transcription factor activator protein-2 (AP-2). Both UVR and reactive oxygen species (ROS) activate AP-2 and lead to activation of ICAM-1.[45] Patients with PLE might have a genetic predisposition that leads to an abnormal induction of AP-2 and a subsequent de-regulation of pro-inflammatory genes such as ICAM-1.[30] Also, a stronger activation and/or delayed down-regulation of ICAM-1 may lead to a sustained inflammatory response and ultimately to the skin changes seen in PLE.[31][46]
A 2017 genome-wide expression analysis, attributed 14 genes with lower expression in PLE compared to healthy controls, including complement 1s subunit (C1s), scavenger receptor B1 (SCARB1) fibronectin (FN1), immunoglobulin superfamily member 3 (IGSF3), caspase-1 (CASP1) and paraoxonase 2 (PON2), all genes associated with apoptotic cell clearance.[47]
Modification of potential proteins during apoptosis could lead to the formation of neo auto-antigens, exacerbated by reduced expression of these genes.[48] Accumulation of apoptotic cells post-UV-A and ultraviolet B (UV-B) irradiation has been demonstrated in vivo.[49]
Classification
Morphological criteria for PLE
There are 3 main types.
Papular type consists of small erythematous, occasionally urticarial papules on patchy erythematous skin, disseminated over the individual predilection site; this is the most common type.
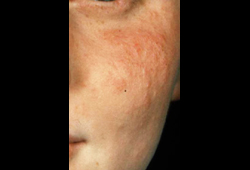
Subtype 1 (small papular type): pinpoint-size papules that are densely aggregated.[Figure caption and citation for the preceding image starts]: Small papular type of PLE with densely aggregated pinpoint size papules on the faceImage provided by Dr Hadshiew; used with permission [Citation ends].
Subtype 2 (haemorrhagic type): rare variant with papules and petechiae.
Plaque type consists of sharply defined, infiltrated erythematous plaques, more common on the face. [Figure caption and citation for the preceding image starts]: Typical presentation of extensive plaque-type PLE on the chestImage provided by Dr Hadshiew; used with permission [Citation ends].
Subtype 1 (erythema exudativum multiforme type): figurate plaques forming cockaded lesions; rare.
Papular-vesicular type is a combination of papules and vesicles, occasionally bullae. [Figure caption and citation for the preceding image starts]: Papular-vesicular type on the commonly affected V-neck areaImage provided by Dr Hadshiew; used with permission [Citation ends].
Subtype 1 (ictus type): typically a central vesicle is surrounded by multiple scarcely disseminated urticarial papules.
Subtype 2 (vesiculobullous type): rare and more extreme variant with papules and bullae.
Use of this content is subject to our disclaimer