Approach
The clinical presentation of bursitis is variable, as it depends on the affected bursa and the duration of symptoms. Imaging studies are not usually required, as the diagnosis can be made on clinical grounds.
History and examination
Patients with acute bursitis typically complain of pain localised to the site of the bursa, particularly on movement. There may be a history of trauma, repetitive occupational activity, autoimmune disease, or crystal arthropathy. Infection may follow a penetrating injury or foreign body. If the bursa is superficial, swelling and erythema may be evident. In bursitis secondary to crystal deposition, the bursa is usually particularly erythematous, painful, and warm to the touch.
Chronic bursitis may last for several months and flare up many times. If inflammation persists near a joint, the patient is likely to have a limited range of active movement.[5][6][7][8] Typically in bursitis, the passive range of motion is preserved, whereas active movement is limited.
Septic bursitis is most common in the prepatellar and olecranon bursae due to their superficial position. Symptoms suggestive of septic bursitis include a low-grade temperature, local erythema, swelling, and warmth, sometimes with local cellulitis.
Subacromial bursitis: classically in subacromial bursitis, the patient will complain of a painful arc on abduction of the arm due to impingement of the bursa under the coracoacromial arch. This can also occur with rotator cuff tears, and the two conditions may coexist.
Trochanteric bursitis: there may be risk factors present causing an alteration in gait. Trochanteric bursitis is often referred to as ‘greater trochanteric pain syndrome’ in recognition of the complex anatomy of the area and that pain is not always from a true bursitis. Diagnostic criteria have been proposed, but their sensitivity, specificity, and predictive value have not been established.[5][12] The criteria propose that lateral hip pain and tenderness around the greater trochanter must be present in combination with 1 of the following:
Pain at the extremes of rotation, abduction, or adduction
Pain of contraction of the hip abductors against resistance
Pseudoradiculopathy: pain radiating down the lateral aspect of the thigh.
Bursae of the knee: with anserine bursitis, the patient will typically complain of tenderness on the upper medial tibia at a point 3 cm to 5 cm distal to the medial knee joint line.[7] A valgus deformity may be noted.
With prepatellar and infrapatellar bursitis, the prepatellar bursa is located between the skin and patella, and the infrapatellar bursa is between the skin and tibial tuberosity. Swelling and erythema are common, and the patella may be impalpable if a lot of fluid is present.
Anserine bursitis, and sometimes prepatellar bursitis, may be difficult to differentiate from knee osteoarthritis on history and examination.
Olecranon bursitis: a superficial bursa, susceptible to infection and usually accompanied by significant swelling. The patient may recall direct trauma to the elbow. [Figure caption and citation for the preceding image starts]: Clinical presentation of a patient with olecranon bursitisFrom the personal collection of Nicola Maffulli, MD, MS, PhD, FRCS(Orth); used with permission [Citation ends].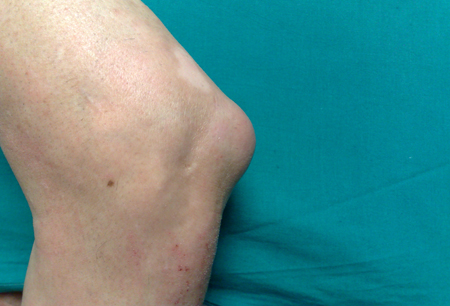
Retrocalcaneal bursitis: tenderness along the distal portion of the Achilles tendon associated with swelling is typical.[13] There may be a palpable bump, and poorly fitting shoes may play a role.
Investigations
If septic bursitis is suspected, the fluid should be aspirated and sent for laboratory analysis with Gram stain and culture. If fluid is aspirated, it is recommended that some also be sent for crystal analysis, especially if there is a history of gout or calcium pyrophosphate deposition disease. Aspiration should be carried out in an aseptic manner. Superficial bursae such as the prepatellar and olecranon bursa can easily be drained, but ultrasound (US) guidance may be useful if the bursa is deeper.
The American College of Radiography (ACR) recommends plain x-rays for investigating chronic hip, knee, or shoulder pain, where bursitis is suspected, and for excluding less common causes of chronic pain such as bone tumours.[14][15][16] Where radiography is non-diagnostic and a hip or shoulder bursitis is suspected, non-contrast magnetic resonance imaging (MRI) or US may be useful for identifying changes in soft-tissue structures and evaluating fluid collection.[14][16] MR or computed tomography (CT) arthrography may also be subsequently considered for suspected subacromial subdeltoid bursitis in shoulder pain.[16] US or MRI of the knee is not usually useful, although MRI may help in the diagnosis of deep infrapatellar bursitis.[15]
Use of this content is subject to our disclaimer