Differentials
Common
Non-secretory adrenal adenomas
History
asymptomatic
Exam
no examination findings
1st investigation
- CT abdomen:
lipid-rich adrenal adenomas typically have ≤10 Hounsfield units attenuation characteristics on non-contrast CT; lipid-poor adrenal adenomas typically have contrast-medium washout ≥60% at 15 minutes on contrast-enhanced CT scan
More
Other investigations
- chemical shift MRI:
any lipid-containing tissue shows a signal loss caused by cancellation of the signal from fat and water on opposed-phase compared with in-phase images; visual analysis of in-phase and opposed-phase images detects lipid within adrenal masses
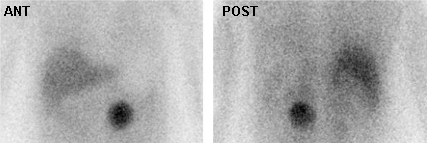
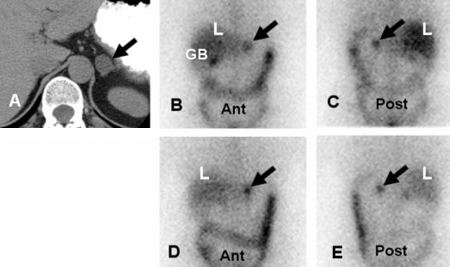
More - 131-I radioiodine-labeled norcholesterol (NP-59) scintigraphy:
concordant tracer uptake (uptake greater on the side of the mass); the contralateral gland may appear normal or show variable degree of suppression
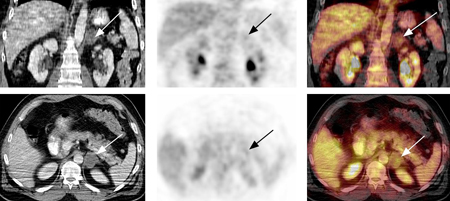
More - 18-fluoro-2-deoxyglucose (FDG) PET:
typically displays low FDG uptake; however, 16% of benign adrenal lesions have FDG uptake >background liver uptake
More
Uncommon
Cushing syndrome
History
weight gain with central obesity, facial rounding, easy bruising, thin skin, poor wound healing, purple striae, cognitive and emotional changes, acne, hirsutism, diabetes mellitus
Exam
hypertension, supraclavicular and dorsocervical fat pads, proximal muscle weakness
1st investigation
Phaeochromocytoma
History
may be asymptomatic; episodic or severe hypertension, forceful heartbeat, pallor, severe anxiety, headache may be spontaneous or precipitated by postural change, anxiety, medications such as metoclopramide or anaesthetic agents, or manoeuvres that increase intra-abdominal pressure such as lifting, exercise, pregnancy, trauma
Exam
hypertension (paroxysmal or sustained), tachycardia, orthostatic hypotension, pallor, retinopathy, tremor, fever
1st investigation
- fractionated plasma metanephrines:
plasma metanephrine ≥0.5 nanomol/L; plasma normetanephrine ≥0.9 nanomol/L
More
Other investigations
- 24-hour urine collection for total metanephrines and catecholamines:
total metanephrines ≥6.8 nanomol/24 hours; adrenaline (epinephrine) >191 nanomol/24 hours; noradrenaline (norepinephrine) >1004 nanomol/24 hours; dopamine >4566 nanomol/24 hours
More - CT abdomen:
heterogeneous adrenal mass; haemorrhage and cystic areas are common; >10 Hounsfield units on unenhanced CT; vascular mass on contrast-enhanced CT with contrast washout <50% at 10 minutes[5]
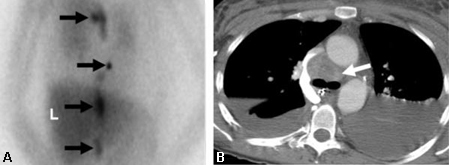
- MRI abdomen:
markedly hyperintense mass in relation to the liver on T2-weighted image
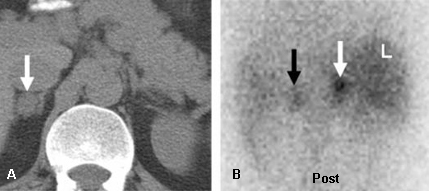
- 123-I or 131-I metaiodobenzylguanidine (MIBG) scintigraphy:
intense focal uptake in the lesion
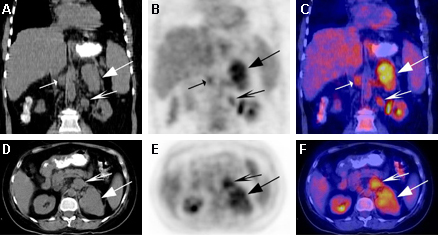
More - 18-fluoro-2-deoxyglucose (FDG) PET:
intense focal uptake in the lesion
More - fluorine-18-L-dihydroxyphenylalanine PET:
intense focal uptake in the lesion
More
Primary hyperaldosteronism
History
hypokalaemia-related symptoms include nocturia, polyuria, muscle cramps, palpitations
Exam
hypertension
1st investigation
Other investigations
- plasma aldosterone concentration on an unrestricted salt diet:
>2.2 picomoles/L (>10 nanograms/dL)
More - 24-hour urinary aldosterone excretion:
>58.2 nanomol/24 hours
More - saline infusion test (saline suppression test):
post-saline plasma aldosterone concentration >0.14 nanomol/L
More - CT abdomen:
aldosteronoma: homogeneous mass, usually ≤3 cm, with unenhanced CT attenuation ≤10 Hounsfield units and CT contrast-medium washout ≥60% at 15 minutes;[5] bilateral adrenal hyperplasia: the adrenal glands may be normal or have a nodular or multinodular appearance; the adrenals may appear asymmetrically enlarged, with unilateral or bilateral nodules
- MRI abdomen:
homogeneous mass with isointense signal in relation to liver on T2-weighted images[5]
- 131-I radioiodine-labeled norcholesterol (NP-59) scintigraphy (after dexamethasone suppression 1 mg orally every 6 hours for 7 days):
focal uptake in unilateral pattern (aldosteronoma) or bilateral pattern (adrenal hyperplasia)
More - adrenal venous sampling:
confirms that the adrenal mass (and not bilateral adrenal hyperplasia) is the source of aldosterone excess in patients with primary aldosteronism[5]
Adrenal cysts
History
asymptomatic, presents in fifth or sixth decade, female preponderance
Exam
no examination findings
1st investigation
- CT abdomen:
unilateral, solitary, low-density lesions with a smooth, thin wall; peripheral curvilinear calcifications are seen in 15% cases; occasionally (<20% cases) benign cysts may demonstrate hyperattenuation (>60 Hounsfield units) due to intracystic haemorrhage
More
Other investigations
Adrenal myelolipomas
History
typically asymptomatic, may present with abdominal pressure or pain if large
Exam
no examination findings
1st investigation
- CT abdomen:
appearance is variable, depending on the histologic composition of myelolipoma, ranging from a fat-dominant mass to a completely non-fatty soft-tissue mass; the mass typically has low attenuation (-30 to -115 Hounsfield units), may contain small calcifications (in up to 20% cases), and heterogeneously enhances after contrast administration
Other investigations
Adrenal haemangiomas
History
typically asymptomatic, may present with abdominal pressure if large
Exam
no examination findings
1st investigation
- CT abdomen:
hypoattenuating or heterogeneously attenuating mass, with calcifications present in 66% of cases; the presence of phleboliths within the lesion is characteristic of a haemangioma
Other investigations
- contrast CT abdomen:
characteristic marked peripheral nodular enhancement due to progressive contrast filling of vascular lakes[24]
Adrenal ganglioneuroma
History
typically asymptomatic, may present with abdominal pain
Exam
no examination findings
1st investigation
Granulomatous infiltrative adrenal lesions
History
weakness, fatigue, anorexia, nausea, vomiting, weight loss, history of immunocompromise
Exam
hyperpigmentation of skin and mucous membranes
1st investigation
- CT abdomen:
bilateral adrenal enlargement with central hypoattenuation and peripheral contrast enhancement
More
Other investigations
Adrenocortical carcinoma
History
abdominal pressure or pain, acne, hirsutism, amenorrhoea or oligomenorrhoea, gynaecomastia, diabetes mellitus
Exam
Cushingoid features may be present, such as hypertension, supraclavicular and dorsocervical fat pads, proximal muscle weakness
1st investigation
- CT abdomen:
large and heterogenous mass, usually >4 cm, with irregular contour and >10 Hounsfield units on unenhanced CT; vascular mass on contrast-enhanced CT with contrast washout <60% at 15 minutes
Other investigations
- MRI abdomen:
hyperintense mass in relation to liver on T2-weighted images
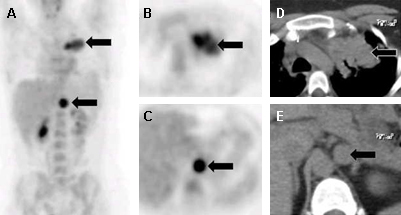
- 18-fluoro-2-deoxyglucose (FDG) PET:
focal activity in the lesion, may display central photopenic area surrounded by rim of intense activity if large tumour with necrotic centre
More
Adrenal metastases
History
weakness, fatigue, anorexia, nausea, vomiting, weight loss, history of cancer
Exam
hyperpigmentation of skin and mucous membranes, hypotension
1st investigation
- serum electrolyte panel:
hyponatraemia
- fasting blood glucose:
hypoglycaemia
- CT abdomen:
heterogeneous, irregular mass of variable size (frequently <3 cm), often bilateral, with unenhanced CT attenuation >10 Hounsfield units and CT contrast-medium washout <50% at 10 minutes[5]
- serum electrolyte panel:
hyponatraemia
- fasting blood glucose:
hypoglycaemia
Other investigations
- MRI abdomen:
hyperintense lesion in relation to liver on T2-weighted image, with occasional haemorrhage or cystic areas[5]
- 18-fluoro-2-deoxyglucose (FDG) PET:
focal activity in the lesion
More - CT-guided fine needle aspiration (FNA) biopsy:
used to differentiate between adrenal tissue and non-adrenal tissues (e.g., metastases or infection)
More
Adrenal malignant melanoma
History
may be asymptomatic; abdominal pressure and/or pain
Exam
no examination findings
1st investigation
- CT abdomen:
large, unilateral adrenal mass; possible central necrosis and calcification
- 18-fluoro-2-deoxyglucose PET/CT:
metabolically avid lesion with possible central photopenia
Other investigations
- adrenal biopsy:
definitive diagnosis is on demonstration of melanin in the tumour
Use of this content is subject to our disclaimer