Differentials
Common
Skull fracture (excl. base of skull)
History
history of a high-velocity, direct impact to skull, a fall from height, or motor vehicle-related injury
Exam
evidence of scalp haematoma, crepitance, laceration or bony deformity; Glasgow Coma Scale score and focal deficits vary depending on underlying intracranial injury
1st investigation
- head CT (non-contrast):
will detect most skull fractures using the bone windows, and most underlying injury using the brain windows; compared with a suture, a fracture tends to be wider at the centre and more narrowed at the ends, more than 3 mm in width, and runs in straight lines with angulated turns; a fracture can be linear or comminuted, and may be depressed through the inner table
More
Other investigations
- skull x-ray:
skull fracture
More
Base of skull fracture
History
history of high-velocity impact to the back of the head; may report clear fluid or blood draining from nose or ears; may report facial numbness, vertigo, or hearing deficits
Exam
post-auricular or periorbital ecchymosis, cerebrospinal fluid otorrhoea or rhinorrhoea, haemotympanum, cranial nerve VII and VIII deficits
1st investigation
- head CT (non-contrast):
will detect most skull fractures using the bone windows, and most underlying injury using the brain windows
More
Cerebral contusion
History
history of direct impact or acceleration/deceleration typically due to fall or motor vehicle-related injury; may have history of loss of consciousness
Exam
scalp trauma may be present; depending on severity; Glasgow Coma Scale score may be normal or decreased; if severe may have focal deficits, seizures, or signs of increased intracranial pressure
1st investigation
- head CT (non-contrast):
single or multiple parenchymal lesions, contusions commonly found on the frontal and temporal poles; approximately half are haemorrhagic: a focus of hyperdensity, surrounded by a hypodense area representative of oedema; non-haemorrhagic lesions may be difficult to see on initial CT
More
Other investigations
- head MRI:
haemorrhagic contusions are hyperdense on T1-weighted imaging and hypodense on T2-weighted imaging; non-haemorrhagic lesions are hypodense on T1-weighted imaging and hyperdense on T2 imaging
More
Intracerebral haemorrhage
History
history of direct impact or rapid acceleration/deceleration typically due to fall or motor vehicle-related injury; witnesses may report lucid period, followed by progressive altered mental status
Exam
evidence of scalp trauma is common; seizures or focal neurological deficits related to area of haemorrhage may be present; evidence of raised intracranial pressure and herniation: altered mental status, pupillary irregularity, extension to pain, respiratory irregularity, papilloedema, fundal haemorrhage
1st investigation
- head CT (non-contrast):
hyperdense area of haemorrhage, surrounded by a hypodense area of oedema
More
Other investigations
- head MRI:
acute haemorrhage is hyperdense on T1-weighted imaging and hypodense on T2-weighted imaging
More
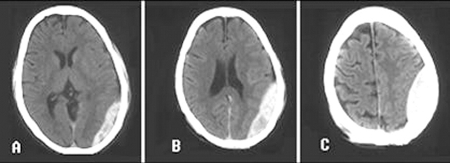
Subdural haematoma
History
history of direct impact or rapid acceleration/deceleration due to fall or motor vehicle-related injury; increased risk in patients with bleeding diathesis, anticoagulant medications, alcohol misuse; history of a fall is more common in patients with significant cerebral atrophy
Exam
scalp trauma may be present; focal neurological deficits may develop, altered mental status depending on size of lesion; may have signs of increased intracranial pressure as haematoma size increases
1st investigation
- head CT (non-contrast):
characteristically crescent-shaped; blood does not cross the midline; in the setting of acute bleeding, areas of hypodense and hyperdense haematoma produce a swirling appearance
More
Other investigations
- head MRI:
T1-weighted MRI will appear as hypointense or iso-intense acutely; T2-weighted imaging will display SDH as hyperintense within the first few hours, progressing to a hypointensity over the ensuing week
More
Epidural haematoma
History
history of direct impact, patient may have had a lucid interval and then progressive deterioration of Glasgow Coma Scale
Exam
commonly scalp trauma over the temporal bone; focal neurological deficits and progressive altered mental status
1st investigation
- head CT (non-contrast):
a hyperdense extra-axial lesion with smooth margins on CT; a lentiform appearance, forming a biconvex shape as blood pushes on the brain surface; blood does not cross suture lines; swirling areas of varying density indicates active bleeding
More
Other investigations
- MRI head:
can aid in the visualisation of small EDH; signal intensity as similar to that seen with subdural haematoma
Intraventricular haemorrhage
History
history of direct impact or rapid acceleration/deceleration due to fall or motor vehicle-related injury; depending on degree of hydrocephaly, the patient may present with headache, vomiting, and ataxia or have progressed to an altered mental status
Exam
signs are due to secondary obstructive hydrocephalus and raised intracranial pressure: papilloedema, fundal haemorrhage, decreased consciousness; signs of herniation include pupillary dilation, bilateral ptosis, impaired upgaze, extension to pain, and respiratory irregularity
1st investigation
- head CT (non-contrast):
blood in the ventricles will appear as hyperdense, commonly seen in the lateral ventricles; often other associated pathology; hydrocephalus may be seen
More
Other investigations
Traumatic subarachnoid haemorrhage
History
history of direct impact or rapid acceleration/deceleration, can occur due to a fall, but must rule out aneurysmal subarachnoid haemorrhage (SAH); aneurysmal SAH more likely if history of sudden onset of severe headache, meningeal symptoms, nausea; an be mild with minimal symptoms, or severe with symptoms of increased intracranial pressure (ICP): altered mental status, decreased consciousness
Exam
can be mild with minimal signs, or severe with signs of increased ICP: papilloedema, fundal haemorrhage, altered mental status, decreased consciousness; signs of herniation: pupillary dilation, bilateral ptosis, impaired upgaze, extension to pain, respiratory irregularity
1st investigation
- head CT (non-contrast):
SAH on CT can be subtle; the basilar cisterns (suprasellar and quadrigeminal cisterns) should be inspected carefully for the presence of SAH, which appears hyperdense compared with cerebrospinal fluid
More
Other investigations
- CT angiography (CTA):
may be performed if aetiology of SAH as traumatic is uncertain; visualises potential vascular abnormalities or active bleeding sites
- head MRI:
SAH present
More - ECG:
non-specific; ischaemic ECG changes in SAH include ST elevation or depression, abnormal T-wave morphology, prolonged QTc interval and U-waves.[142]
Penetrating injuries
History
history of high-velocity impact or missile injuries; symptoms depend on nature of injury and brain regions affected
Exam
should visualise and palpate for scalp defect, crepitance, obvious skull deformity or protruding foreign body; may have localising neurological deficits or seizures
1st investigation
- head CT (non-contrast):
the initial test of choice and can demonstrate the nature of the intracranial pathology and presence or absence of fractures and foreign bodies
More
Other investigations
- CT angiography:
may be required to evaluate further vascular injuries
- MRI:
contraindicated if there is any suspicion that a metal object has penetrated the skull
Diffuse axonal injury
History
history of direct impact or rapid acceleration/deceleration of head; depending on severity, may complain of headache or vomiting, or have had a rapid progressive deterioration of Glasgow Coma Scale and coma
Exam
patients with severe diffuse axonal injury (DAI) present with altered mental status or coma; classically have physical examination findings disproportionate to CT findings
1st investigation
- head CT (non-contrast):
initially normal in more than half of patients with DAI; should look for oedema and petechial haemorrhage, at the grey/white junction, within the corpus callosum, and the brainstem
More
Other investigations
- MRI:
indicated when CT does not explain patient’s symptoms; more sensitive for micro-haemorrhage and oedema
Mild traumatic brain injury
History
history of blunt trauma or acceleration/deceleration forces; can result in confusion, disorientation, or impaired consciousness, dysfunction of memory around the time of the injury, loss of consciousness lasting 30 minutes or less, post-traumatic amnesia for less than 24 hours; can cause observed signs of neurological or neuropsychological dysfunction such as seizures acutely following injury; symptoms include headache, dizziness, fatigue, irritability, and poor concentration (typically referred to as 'post-concussive symptoms')
Exam
Glasgow Coma Scale score of no worse than 13 after 30 minutes post injury or later upon presentation for health care; other transient neurological abnormalities such as focal signs, seizure, and intracranial lesion not requiring surgery may be present
1st investigation
- head CT (non-contrast):
usually normal
More
Other investigations
- head MRI:
usually normal
More
Use of this content is subject to our disclaimer