Investigations
1st investigations to order
lupus anticoagulant
Test
Diagnosis of lupus anticoagulant is based on coagulation assays and involves an initial detection stage, followed by a confirmation stage.[36][37]
The principle of the assay is the prolongation of a phospholipid-dependent coagulation test by the antibody. In the confirmation stage, addition of negatively charged phospholipid binds the antibody and thus the coagulation time is shortened. Whenever possible, lupus anticoagulant testing should be performed before initiation of anticoagulation as anticoagulants may lead to false-positive results. When this is not possible, testing can be performed on unfractionated heparin or low molecular heparin as long as the assay contains a heparin neutraliser and drug levels are not supra-therapeutic.[38] Testing for lupus anticoagulants in patients on direct oral anticoagulants is not recommended unless they are removed or neutralised.
Result
positive on 2 occasions, 12 weeks apart
anticardiolipin antibodies
Test
Anticardiolipin antibody of IgG or IgM isotype in serum or plasma present in medium or high titre (>40 IgG phospholipid [GPL] units or IgM phospholipid [MPL] units, or >99th percentile) on 2 or more occasions, at least 12 weeks apart, by standardised enzyme-linked immunosorbent assay (ELISA).[1][2][39]
Result
elevated on 2 occasions, 12 weeks apart
anti-beta2-glycoprotein I antibodies
antinuclear antibody, double-stranded DNA, and extractable nuclear antigen antibodies
Test
Presence of these antibodies may suggest underlying associated systemic lupus erythematosus.
Result
elevated in systemic lupus erythematosus
FBC
Test
Thrombocytopenia may be present in antiphospholipid syndrome, often due to an immune mechanism or the presence of another autoimmune disease (idiopathic thrombocytopenic purpura). Anaemia may be due to an immune mechanism and present as haemolytic anaemia.
Result
may show thrombocytopenia or anaemia
creatinine and urea
Test
Creatinine and urea levels should be performed to assess renal function.
Rarely nephropathy (manifesting as oedema and proteinuria) can be due to microangiopathic thrombosis secondary to antiphospholipid syndrome.[31]
Result
elevated if nephropathy is present
Investigations to consider
venous Doppler ultrasound
Test
Presence of a deep vein thrombosis (DVT) or arterial thrombosis is considered a clinical criterion for the diagnosis of antiphospholipid syndrome; the clot must be documented by imaging studies.
Result
variable; may show evidence of DVT if not already confirmed
venography or MRI
Test
Presence of a deep vein thrombosis (DVT) or arterial thrombosis is considered a clinical criterion for the diagnosis of antiphospholipid syndrome; the clot must be documented by imaging studies.
Result
variable; may show evidence of DVT if not already confirmed
MRI of thrombosis
Test
Presence of a deep vein thrombosis (DVT) or arterial thrombosis is considered a clinical criterion for the diagnosis of antiphospholipid syndrome; the clot must be documented by imaging studies. [Figure caption and citation for the preceding image starts]: Magnetic resonance direct thrombus imaging of bilateral proximal DVTFrom the personal teaching collection of Professor Hunt; used with permission [Citation ends].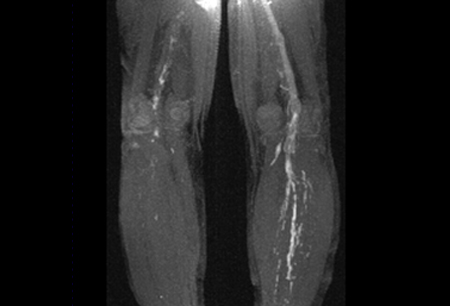
Result
variable; may show evidence of DVT if not already confirmed
CT angiogram of the chest
Test
Presence of a pulmonary embolus is considered a clinical criterion for the diagnosis of antiphospholipid syndrome. To be considered a clinical criterion, the clot must be documented by imaging studies.
Result
variable; may show evidence of a pulmonary embolism if not already confirmed
ventilation-perfusion (V/Q) scan
Test
Presence of a pulmonary embolus is considered a clinical criterion for the diagnosis of antiphospholipid syndrome. To be considered a clinical criterion, the clot must be documented by imaging studies.
Result
variable; may show evidence of a pulmonary embolism if not already confirmed
cranial MRI
Test
This is neither sensitive nor specific for antiphospholipid syndrome, but arterial thrombosis is considered a clinical criterion and must be documented by imaging studies.
Result
variable; may show evidence of an ischaemic stroke if not already confirmed
echocardiography
Test
Echocardiography is indicated in patients with clinical features indicative of heart valve lesions or vegetations. A transoesophageal echocardiogram is the most sensitive study to identify these lesions and should be performed if there is a high index of suspicion.
Vegetations, valve thickening, and heart valve dysfunction seem to be more frequent in antiphospholipid syndrome (APS) than in patients with systemic lupus erythematosus alone. This is known as Libman-Sacks endocarditis and may relate to fibrin deposition on the valves. The mitral valve is most commonly affected. Up to 20% of patients with APS have valve abnormalities, although they rarely cause haemodynamic problems.[40]
Result
variable; may demonstrate valve vegetations
inherited thrombophilia test
Test
May be considered in patients presenting with a first venous thromboembolism (VTE) at an early age or who have family history of VTE to exclude an inherited thrombophilia.
Includes protein C level, free protein S level, activated protein C resistance, antithrombin level, factor V Leiden, and/or polymerase chain reaction for prothrombin gene mutation (G-20210-A).
Result
usually negative, inherited thrombophilia in patients with APS are rare
Use of this content is subject to our disclaimer