Renal artery stenosis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
atherosclerotic RAS
antihypertensive therapy + lifestyle modification
The majority of patients with RAS have refractory or difficult-to-control hypertension. Thus, first-line treatment in this condition involves BP control to a target of <130/80 mmHg, given the high likelihood of concomitant cardiovascular disease.
Renin-angiotensin blockade with an ACE inhibitor or angiotensin II receptor antagonist is an attractive first-line antihypertensive strategy, as their actions target the mechanism of hypertension in RAS. However, it is recommended that BP, kidney function, and electrolytes be followed closely after initiating therapy.
Patients may require referral to a hypertension consultant (e.g., cardiologist or nephrologist).
Some commonly prescribed antihypertensives are shown below. Doses should be started low and increased according to response.
Lifestyle changes include weight loss, low-salt diet, and smoking cessation.
Primary options
captopril: 12.5 to 25 mg orally three times daily
OR
enalapril: 10-20 mg orally once daily
OR
valsartan: 80-160 mg orally once daily
OR
losartan: 25-100 mg orally once daily
Secondary options
hydrochlorothiazide: 25 mg orally once daily
OR
furosemide: 40 mg orally once daily
OR
atenolol: 50-100 mg orally once daily
OR
amlodipine: 10 mg orally once daily
OR
nifedipine: 30 mg orally (extended-release) once daily
OR
prazosin: 2.5 mg orally once daily
Tertiary options
clonidine: 0.1 mg orally twice daily
OR
hydralazine: 10-50 mg orally four times daily
OR
methyldopa: 250-500 mg orally twice daily
OR
minoxidil: 5-40 mg orally once daily
statin
Treatment recommended for ALL patients in selected patient group
As atherosclerotic RAS is a type of vascular disease, statins should be considered for all patients.
Although direct evidence is lacking for this recommendation, the high prevalence of concomitant peripheral vascular disease (PVD) and coronary artery disease (CAD) makes this recommendation reasonable. However, there are no published studies evaluating particular statin drugs, doses, or LDL cholesterol targets in this population.
Weak evidence suggests that statins may slow the progression of atherosclerotic RAS.[46]Cheung CM, Patel A, Shaheen N, et al. The effects of statins on the progression of atherosclerotic renovascular disease. Nephron Clin Pract. 2007;107(2):c35-42. http://www.ncbi.nlm.nih.gov/pubmed/17713349?tool=bestpractice.com [47]Hanzel G, Balon H, Wong O, et al. Prospective evaluation of aggressive medical therapy for atherosclerotic renal artery stenosis, with renal artery stenting reserved for previously injured heart, brain, or kidney. Am J Cardiol. 2005 Nov 1;96(9):1322-7. http://www.ncbi.nlm.nih.gov/pubmed/16253607?tool=bestpractice.com
Any statin may be used, with a target LDL cholesterol <1.813 to 2.59 mmol/L (70 to 100 mg/dL).
Baseline and periodic evaluation of liver function tests is recommended.
Primary options
atorvastatin: 10-80 mg orally once daily
OR
fluvastatin: 20-80 mg/day orally (immediate-release) given in 1-2 divided doses
OR
lovastatin: 10-80 mg/day orally (immediate-release) given in 1-2 divided doses
OR
rosuvastatin: 5-40 mg orally once daily
OR
simvastatin: 5-40 mg orally once daily; increased risk of myopathy with 80 mg/day dose
antiplatelet agent
Treatment recommended for ALL patients in selected patient group
Aspirin should be considered for all patients with atherosclerotic RAS.[16]Anderson JL, Halperin JL, Albert NM, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Apr 2;127(13):1425-43. http://circ.ahajournals.org/content/127/13/1425.long http://www.ncbi.nlm.nih.gov/pubmed/23457117?tool=bestpractice.com
Primary options
aspirin: 75-300 mg orally once daily
renal artery stenting + continuation of medical therapy
There are no data supporting routine renal artery stenting in asymptomatic patients in whom RAS is incidentally found.[2]Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic). Circulation. 2006 Mar 21;113(11):e463-654. http://circ.ahajournals.org/content/113/11/e463.long http://www.ncbi.nlm.nih.gov/pubmed/16549646?tool=bestpractice.com
Renal percutaneous vascular intervention appears to be no better than maximal optimal medical therapy.[45]Cooper CJ, Murphy TP, Cutlip DE, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014 Jan 2;370(1):13-22. http://www.ncbi.nlm.nih.gov/pubmed/24245566?tool=bestpractice.com However, in selected cases, guidelines suggest that renal artery stenting be considered in the following circumstances: refractory hypertension on a multi-drug regimen (≥3 medications); progressive chronic kidney disease; acute kidney injury on ACE inhibitors/angiotensin-II receptor antagonists in patients with congestive heart failure (CHF); recurrent flash pulmonary oedema; bilateral RAS; stenosis of renal artery supplying single functioning kidney; salvage therapy in recent-onset end-stage renal failure; patients with RAS, uncontrolled hypertension, and unstable angina.[3]Haller C, Keim M. Current issues in the diagnosis and management of patients with renal artery stenosis: a cardiologic perspective. Prog Cardiovasc Dis. 2003 Nov-Dec;46(3):271-86. http://www.ncbi.nlm.nih.gov/pubmed/14685944?tool=bestpractice.com [19]Hicks CW, Clark TWI, Cooper CJ, et al. Atherosclerotic renovascular disease: a KDIGO (Kidney Disease: Improving Global Outcomes) controversies conference. Am J Kidney Dis. 2022 Feb;79(2):289-301. https://www.doi.org/10.1053/j.ajkd.2021.06.025 http://www.ncbi.nlm.nih.gov/pubmed/34384806?tool=bestpractice.com [44]Bhalla V, Textor SC, Beckman JA, et al. Revascularization for renovascular disease: a scientific statement from the American Heart Association. Hypertension. 2022 Aug;79(8):e128-43. https://www.doi.org/10.1161/HYP.0000000000000217 http://www.ncbi.nlm.nih.gov/pubmed/35708012?tool=bestpractice.com
Patient factors that may suggest clinical benefit of revascularisation include a recent onset or exacerbation of hypertension (<1 year), absence of proteinuria, and identifiable activation of the renin-angiotensin system (e.g., hyperreninaemia).[44]Bhalla V, Textor SC, Beckman JA, et al. Revascularization for renovascular disease: a scientific statement from the American Heart Association. Hypertension. 2022 Aug;79(8):e128-43.
https://www.doi.org/10.1161/HYP.0000000000000217
http://www.ncbi.nlm.nih.gov/pubmed/35708012?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Digital subtraction angiography in a patient with significant atherosclerotic left renal artery stenosis. Panel A, prior to stent placement. Panel B, after successful stent deployment. Arrows indicate the site of stenosis and stent placement in their respective panelsCourtesy of Alvaro Alonso, MD and Scott J. Gilbert, MD [Citation ends].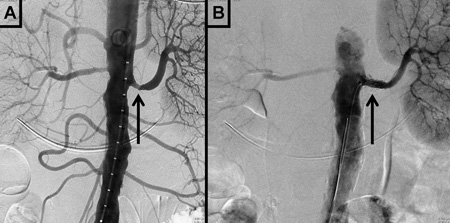
Patients should be referred to a peripheral vascular interventions specialist if revascularisation is considered. Current medical therapy should be continued and maximised. Transient addition of clopidogrel should be considered for dual antiplatelet therapy after the procedure.
post-stent clopidogrel
Treatment recommended for ALL patients in selected patient group
Patients undergoing renal artery stenting require dual antiplatelet therapy for a period of time as determined by the vascular specialist.
Patients should continue aspirin, with the addition of clopidogrel after the procedure.
Primary options
clopidogrel: 75 mg orally once daily
surgical reconstruction of the renal arteries
Surgical reconstruction of the renal arteries in the setting of RAS is restricted to those patients undergoing major aortic reconstruction for another reason, such as abdominal aortic aneurysm (AAA) repair or correction of severe aorto-iliac occlusive disease.[16]Anderson JL, Halperin JL, Albert NM, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Apr 2;127(13):1425-43. http://circ.ahajournals.org/content/127/13/1425.long http://www.ncbi.nlm.nih.gov/pubmed/23457117?tool=bestpractice.com
fibromuscular dysplasia
antihypertensive therapy + lifestyle modification
The majority of patients with fibromuscular dysplasia have refractory or difficult-to-control hypertension. Thus, first-line treatment in this condition involves BP control to a target of <140/90 mmHg. More aggressive BP control to <130/80 mmHg is indicated in the presence of concomitant cardiovascular disease.
Although no data support the use of a single agent or combination of drugs over another in fibromuscular dysplasia, the presence of compelling indication in comorbid conditions make antihypertensive selection important.
Furthermore, combination therapy with multiple agents is often necessary.
Renin-angiotensin blockade with an ACE inhibitor or angiotensin II receptor antagonist is an attractive first-line antihypertensive strategy, as their action targets the mechanism of hypertension in RAS. However, it is recommended that BP, kidney function, and electrolytes be followed closely after initiating therapy.
Patients may require referral to a hypertension consultant (e.g., cardiologist or nephrologist).
Some commonly prescribed antihypertensives are shown below. Doses should be started low and increased according to response.
Lifestyle changes include weight loss, low-salt diet, and smoking cessation.
Primary options
captopril: 12.5 to 25 mg orally three times daily
OR
enalapril: 10-20 mg orally once daily
OR
valsartan: 80-160 mg orally once daily
OR
losartan: 25-100 mg orally once daily
Secondary options
hydrochlorothiazide: 25 mg orally once daily
OR
furosemide: 40 mg orally once daily
OR
atenolol: 50-100 mg orally once daily
OR
amlodipine: 10 mg orally once daily
OR
nifedipine: 30 mg orally (extended-release) once daily
OR
prazosin: 2.5 mg orally once daily
Tertiary options
clonidine: 0.1 mg orally twice daily
OR
hydralazine: 10-50 mg orally four times daily
OR
methyldopa: 250-500 mg orally twice daily
OR
minoxidil: 5-40 mg orally once daily
percutaneous renal artery balloon angioplasty
Treatment recommended for ALL patients in selected patient group
Angioplasty, together with antihypertensive therapy, should be considered first-line therapy, as it is often curative. Angioplasty has an initial technical success rate and 10-year patency rate of approximately 90%.[49]Uder M, Humke U. Endovascular therapy of renal artery stenosis: where do we stand today? Cardiovasc Intervent Radiol. 2005 Mar-Apr;28(2):139-47. http://www.ncbi.nlm.nih.gov/pubmed/15770388?tool=bestpractice.com
renal artery stenting and dual antiplatelet therapy
Additional treatment recommended for SOME patients in selected patient group
Stenting is not indicated for initial treatment of fibromuscular dysplasia except in cases of procedural complications during percutaneous renal artery balloon angioplasty (i.e., renal artery dissection). It could be considered in the setting of re-stenosis.[16]Anderson JL, Halperin JL, Albert NM, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Apr 2;127(13):1425-43. http://circ.ahajournals.org/content/127/13/1425.long http://www.ncbi.nlm.nih.gov/pubmed/23457117?tool=bestpractice.com
Patients undergoing renal artery stenting require dual antiplatelet therapy (with aspirin and clopidogrel) following the procedure.
Primary options
aspirin: 75-300 mg orally once daily
and
clopidogrel: 75 mg orally once daily
surgical reconstruction of the renal arteries
Surgical reconstruction of the renal arteries in the setting of fibromuscular dysplasia is restricted to those patients undergoing major aortic reconstruction for another reason. Surgical intervention may be necessary in complex disease that extends into the segmental arteries, and in cases of macroaneurysms.[16]Anderson JL, Halperin JL, Albert NM, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Apr 2;127(13):1425-43. http://circ.ahajournals.org/content/127/13/1425.long http://www.ncbi.nlm.nih.gov/pubmed/23457117?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer