Any sudden loss of hearing occurring in <72 hours needs prompt investigation and, if hearing loss is >30 decibels in ≥3 frequencies, urgent otolaryngeal referral is required. Bedside tuning fork tests should be performed to establish whether the hearing loss is conductive or sensorineural. Formal audiological testing and magnetic resonance imaging are usually required to distinguish possible causes of sudden hearing loss and should be performed within 14 days of symptom onset.[2]Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Clinical Practice Guideline: Sudden Hearing Loss (Update). Otolaryngol Head Neck Surg. 2019 Aug;161(1_suppl):S1-S45.
https://www.doi.org/10.1177/0194599819859885
http://www.ncbi.nlm.nih.gov/pubmed/31369359?tool=bestpractice.com
The National Institute for Health and Care Excellence (NICE) in the UK recommends that any adult with sudden-onset or rapidly worsening hearing loss in one or both ears, not otherwise explained by external or middle ear causes, should be referred to a specialist.[55]National Institute for Health and Care Excellence. Hearing loss in adults: assessment and management. Oct 2023 [internet publication].
https://www.nice.org.uk/guidance/ng98
NICE also makes recommendations on how soon this should be done based on the presenting history.[55]National Institute for Health and Care Excellence. Hearing loss in adults: assessment and management. Oct 2023 [internet publication].
https://www.nice.org.uk/guidance/ng98
Necrotising otitis externa
This usually occurs in patients with diabetes and can be fatal if not treated aggressively. The ear canal may show oedema and granulation tissue at the bony cartilaginous junction. The hearing loss is usually conductive owing to swelling of the ear canal or middle-ear fluid but can also be sensorineural. The hallmark is pain, which may awaken the patient from sleep. Patients in advanced disease may present with lower cranial nerve paralysis. Urgent otolaryngological referral is indicated. Treatment includes biopsy to rule out a malignant neoplasm, such as squamous cell carcinoma, as well as imaging studies to assess the degree of bony and soft-tissue involvement.[56]Chawdhary G, Pankhania M, Douglas S, et al. Current management of necrotising otitis externa in the UK: survey of 221 UK otolaryngologists. Acta Otolaryngol. 2017 Aug;137(8):818-822.
https://www.doi.org/10.1080/00016489.2017.1295468
http://www.ncbi.nlm.nih.gov/pubmed/28301961?tool=bestpractice.com
Sudden sensorineural hearing loss
Sudden sensorineural hearing loss is a subjective sensation of rapid-onset hearing impairment in one or both ears.[2]Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Clinical Practice Guideline: Sudden Hearing Loss (Update). Otolaryngol Head Neck Surg. 2019 Aug;161(1_suppl):S1-S45.
https://www.doi.org/10.1177/0194599819859885
http://www.ncbi.nlm.nih.gov/pubmed/31369359?tool=bestpractice.com
Patients often have symptoms of tinnitus and/or vertigo. On Weber's testing, the patient hears the tuning fork louder in the contralateral ear. Prompt otolaryngology referral is indicated because oral corticosteroid therapy, and sometimes intra-tympanic corticosteroid therapy, may have a role in preventing permanent hearing loss in these conditions.[2]Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Clinical Practice Guideline: Sudden Hearing Loss (Update). Otolaryngol Head Neck Surg. 2019 Aug;161(1_suppl):S1-S45.
https://www.doi.org/10.1177/0194599819859885
http://www.ncbi.nlm.nih.gov/pubmed/31369359?tool=bestpractice.com
Facial nerve palsy
The facial nerve arises from the pons and passes through the acoustic auditory meatus in the petrous temporal bone, in close proximity to the inner ear. Temporal bone fractures, mastoiditis, cholesteatoma, malignant otitis externa, acoustic neuroma and stroke may all cause facial nerve palsy.[57]Yetiser S, Hidir Y, Gonul E. Facial nerve problems and hearing loss in patients with temporal bone fractures: demographic data. J Trauma. 2008 Dec;65(6):1314-20.
http://www.ncbi.nlm.nih.gov/pubmed/19077620?tool=bestpractice.com
[58]Talebnasab MH, Hougaard DD. Transient profound hearing loss and severe facial nerve palsy in schwannomas within the internal acoustic canal: a case report. Oncol Lett. 2023 Mar;25(3):126.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9950335
http://www.ncbi.nlm.nih.gov/pubmed/36844623?tool=bestpractice.com
[59]Silveira RQ, Carvalho VT, Cavalcanti HN, et al. Multiple cranial nerve palsies in malignant external otitis: a rare presentation of a rare condition. IDCases. 2020;22:e00945.
https://www.sciencedirect.com/science/article/pii/S2214250920302535?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/32983891?tool=bestpractice.com
Patients with new onset facial weakness should be referred promptly to an otolaryngologist.[60]Danner CJ. Facial nerve paralysis. Otolaryngol Clin N Am. 2008 Jun;41(3):619-32, xs.
http://www.ncbi.nlm.nih.gov/pubmed/18436002?tool=bestpractice.com
When the eyelids fail to close properly, the lubricating tear film and blink reflex become ineffective. Additionally, parasympathetic dysfunction to the lacrimal gland may result in reduced tear production. Consequently patients may develop keratoconjunctivitis sicca (dry eye) and exposure keratopathy, which can lead to ulcerative keratitis and blindness. Such complications are prevented through the use of a transparent eye shield during the day, artificial tears as needed during waking hours, and an ophthalmological lubricant ointment together with taping of the eyelids closed at bedtime. Indications for ophthalmological consultation include: only seeing eye affected, suspicion of exposure keratitis, and decreased or absent corneal sensation.
Basilar skull fracture
Basilar skull fractures often have specific clinical features. Blood pooling from these fractures can result in ecchymosis over the mastoid area (e.g., Battle's sign); periorbital ecchymosis (raccoon eyes), particularly if unilateral; and bloody otorrhoea. Cerebrospinal fluid (CSF) leakage can result in CSF rhinorrhoea or otorrhoea. Battle's sign and otorrhoea are most often associated with fractures of the petrous portion of the temporal bone.[61]Pretto Flores L, De Almeida CS, Casulari LA. Positive predictive values of selected clinical signs associated with skull base fractures. J Neurosurg Sci. 2000 Jun;44(2):77-82; discussion 82-3.
http://www.ncbi.nlm.nih.gov/pubmed/11105835?tool=bestpractice.com
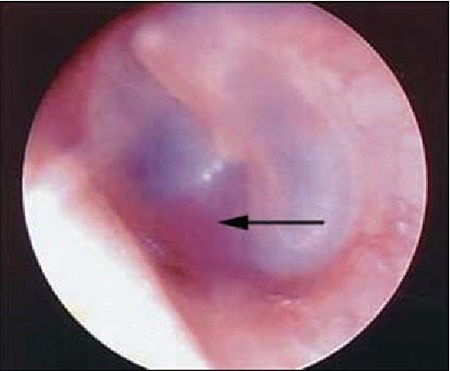
Temporal bone trauma may be accompanied by a tympanic membrane perforation, but hearing loss may also be due to discontinuity of the ossicle chain.[Figure caption and citation for the preceding image starts]: Battle’s signReproduced with permission from van Dijk GW. The bare essentials: head injury. Pract Neurol. 2011 Feb;11(1):50-5. [Citation ends]. [Figure caption and citation for the preceding image starts]: HaemotympanumReproduced with permission from van Dijk GW. The bare essentials: head injury. Pract Neurol. 2011 Feb;11(1):50-5. [Citation ends].
[Figure caption and citation for the preceding image starts]: HaemotympanumReproduced with permission from van Dijk GW. The bare essentials: head injury. Pract Neurol. 2011 Feb;11(1):50-5. [Citation ends].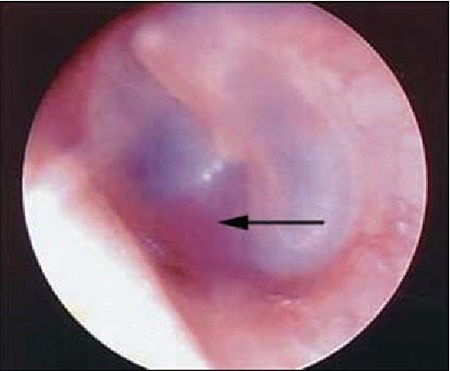
Non-contrast CT is the imaging modality of choice and is superior to MRI for detecting skull fracture in both paediatric and adult patients.[62]American College of Radiology. ACR Appropriateness Criteria: head trauma. 2020 [internet publication].
https://acsearch.acr.org/docs/69481/Narrative
Patients who have a basilar skull fracture should be referred urgently to a neurosurgeon.[63]Johnson F, Semaan MT, Megerian CA. Temporal bone fracture: evaluation and management in the modern era. Otolaryngol Clin N Am. 2008 Jun;41(3):597-618, x.
http://www.ncbi.nlm.nih.gov/pubmed/18436001?tool=bestpractice.com
Ischaemic stroke
Ischaemic stroke affecting the distribution of the internal auditory artery (also called the labyrinthine artery) can cause sudden onset sensorineural hearing loss.[64]Byun S, Lee JY, Kim BG, et al. Acute vertigo and sensorineural hearing loss from infarction of the vestibulocochlear nerve: a case report. Medicine (Baltimore). 2018 Oct;97(41):e12777.
https://journals.lww.com/md-journal/Fulltext/2018/10120/Acute_vertigo_and_sensorineural_hearing_loss_from.77.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30313095?tool=bestpractice.com
[65]Lee H, Kim JS, Chung EJ, et al. Infarction in the territory of anterior inferior cerebellar artery: spectrum of audiovestibular loss. Stroke. 2009 Dec;40(12):3745-51.
https://www.ahajournals.org/doi/10.1161/STROKEAHA.109.564682?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/19797177?tool=bestpractice.com
This may affect both ears and is usually associated with other neurologic findings. In the majority of people, the internal auditory artery is a branch of the anterior cerebellar artery, although it can also arise from the basilar artery. Associated symptoms include tinnitus, vertigo, nausea and vomiting. Other neurological signs are present, e.g. dysarthria, ataxia, facial nerve palsy, nystagmus, diplopia, hemiparesis and/or hemisensory loss.[65]Lee H, Kim JS, Chung EJ, et al. Infarction in the territory of anterior inferior cerebellar artery: spectrum of audiovestibular loss. Stroke. 2009 Dec;40(12):3745-51.
https://www.ahajournals.org/doi/10.1161/STROKEAHA.109.564682?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/19797177?tool=bestpractice.com
[66]Lee H, Whitman GT, Lim JG, et al. Bilateral sudden deafness as a prodrome of anterior inferior cerebellar artery infarction. Arch Neurol. 2001 Aug;58(8):1287-9.
https://www.doi.org/10.1001/archneur.58.8.1287
http://www.ncbi.nlm.nih.gov/pubmed/11493170?tool=bestpractice.com
[67]Huang MH, Huang CC, Ryu SJ, et al. Sudden bilateral hearing impairment in vertebrobasilar occlusive disease. Stroke. 1993 Jan;24(1):132-7.
https://www.doi.org/10.1161/01.str.24.1.132
http://www.ncbi.nlm.nih.gov/pubmed/8418537?tool=bestpractice.com
All patients with a suspected ischaemic stroke should have a non-contrast CT scan of the brain to rule out intracranial haemorrhage. Check blood glucose in all patients with suspected stroke. Prompt administration of intravenous thrombolysis with recombinant tissue plasminogen activator may be indicated to minimise the effects of thrombotic strokes.[68]Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018 Jan 24;49(3):e46-e110.
https://www.doi.org/10.1161/STR.0000000000000158
http://www.ncbi.nlm.nih.gov/pubmed/29367334?tool=bestpractice.com
Vertebral artery dissection
Sudden sensorineural hearing loss can rarely be a symptom of vertebral artery dissection. The most common manifestations of vertebral artery dissection are headache or neck pain.[69]Mattox R, Smith LW, Kettner NW. Recognition of spontaneous vertebral artery dissection preempting spinal manipulative therapy: a patient presenting with neck pain and headache for chiropractic care. J Chiropr Med. 2014 Jun;13(2):90-5.
https://www.sciencedirect.com/science/article/abs/pii/S1556370714000558
http://www.ncbi.nlm.nih.gov/pubmed/25685116?tool=bestpractice.com
[70]Lee VH, Brown RD Jr, Mandrekar JN, et al. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006 Nov 28;67(10):1809-12.
http://www.ncbi.nlm.nih.gov/pubmed/17130413?tool=bestpractice.com
[71]Arnold M, Bousser M. Clinical manifestations of vertebral artery dissection. Front Neurol Neurosci. 2005;20:77-86.
http://www.ncbi.nlm.nih.gov/pubmed/17290114?tool=bestpractice.com
Vertigo, ataxia, nausea, vomiting, nystagmus and cranial nerve palsies may also be present.[72]Gottesman RF, Sharma P, Robinson KA, et al. Clinical characteristics of symptomatic vertebral artery dissection: a systematic review. Neurologist. 2012 Sep;18(5):245-54.
http://www.ncbi.nlm.nih.gov/pubmed/22931728?tool=bestpractice.com
Computed tomography imaging with angiography (CT/CTA) and magnetic resonance imaging with angiography (MRI/MRA) can identify vertebral artery dissection. MRI/MRA better identifies small intramural hematomas, however CT is usually easier to access in the emergency setting.[73]Hanning U, Sporns PB, Schmiedel M, et al. CT versus MR Techniques in the Detection of Cervical Artery Dissection. J Neuroimaging. 2017 Nov;27(6):607-612.
https://www.doi.org/10.1111/jon.12451
http://www.ncbi.nlm.nih.gov/pubmed/28574627?tool=bestpractice.com
Anticoagulation or antiplatelet treatment should be started after confirming the diagnosis and continued for 3 to 6 months to reduce the risk of thrombosis at the dissection site.[74]CADISS trial investigators., Markus HS, Hayter E, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015 Apr;14(4):361-7.
https://www.doi.org/10.1016/S1474-4422(15)70018-9
http://www.ncbi.nlm.nih.gov/pubmed/25684164?tool=bestpractice.com
[75]Peng J, Liu Z, Luo C, et al. Treatment of Cervical Artery Dissection: Antithrombotics, Thrombolysis, and Endovascular Therapy. Biomed Res Int. 2017;2017:3072098.
https://www.doi.org/10.1155/2017/3072098
http://www.ncbi.nlm.nih.gov/pubmed/28607929?tool=bestpractice.com
Intravascular therapy is available in some centres. A combination of techniques including thrombolysis, thrombectomy, stenting and angioplasty is used.[76]Jensen J, Salottolo K, Frei D, et al. Comprehensive analysis of intra-arterial treatment for acute ischemic stroke due to cervical artery dissection. J Neurointerv Surg. 2017 Jul;9(7):654-658.
https://www.doi.org/10.1136/neurintsurg-2016-012421
http://www.ncbi.nlm.nih.gov/pubmed/27286992?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: HaemotympanumReproduced with permission from van Dijk GW. The bare essentials: head injury. Pract Neurol. 2011 Feb;11(1):50-5. [Citation ends].
[Figure caption and citation for the preceding image starts]: HaemotympanumReproduced with permission from van Dijk GW. The bare essentials: head injury. Pract Neurol. 2011 Feb;11(1):50-5. [Citation ends].