Aetiology
WPW pattern on ECG arises from a developmental cardiac defect in the atrioventricular (AV) electrical insulation at the AV groove due to the presence of an accessory pathway (AP). These APs are usually single epicardial strands of tissue that travel across the AV groove to connect the atrium and the adjacent ventricular myocardium. Less commonly, they are multiple hair-like strands or a broad band of tissues. Rarely, these muscle bands extend over coronary sinus diverticula or may connect right atrial appendage to the anterior right ventricle. The anatomical distribution of APs is: 40% to 60% left lateral; 20% right or left posteroseptal area; 13% to 21% right free wall; and 2% to 10% anteroseptal area. Unlike the AV node, where conduction slows at faster rates of stimulation (decremental conduction) approximately 90% of APs are rapidly conducting, resulting in circus movement tachycardia involving the atrium and ipsilateral ventricle with the AP as one limb and AV node as another limb of the circuit (AV re-entrant tachycardias). Approximately 10% of the APs in WPW syndrome are slowly conducting (decremental).
The presence of APs can be associated with various disorders. Ebstein's anomaly is a malformation of the tricuspid valve and right ventricle characterised by adherence of the septal and posterior tricuspid leaflets to the underlying myocardium, apical displacement of the tricuspid annulus, and dilation of the atrialised portion of the right ventricle. Other rare associations include hypertrophic cardiomyopathy, mitral valve prolapse, atrial septal defect, ventricular septal defect, transposition of the great vessels, coarctation of the aorta, dextrocardia, coronary sinus diverticula, right and left atrial aneurysms, cardiac rhabdomyomas (as seen in patients with tuberous sclerosis), Marfan's syndrome, Friedreich's ataxia, Pompe's disease, Danon's disease, and hypokalaemic periodic paralysis. Most cases of WPW are not due to a genetic cause and genetic testing is only relevant if there is pre-excitation in combination with hypertrophic cardiomyopathy and/or progressive cardiac conduction disease. In these patients, the underlying gene PRKAG2 has been identified as a potential cause, resulting in cardiac glycogen storage abnormalities.[10]
The incidence of multiple APs (2 to 5) in patients with WPW syndrome is 5% to 13%.[11] Multiple APs are more commonly observed in patients with a family history of WPW syndrome, Ebstein's anomaly, or other congenital heart diseases (10% to 20%).[10][12] Multiple APs are associated with a higher incidence of antidromic reciprocating tachycardia and a higher incidence of sudden cardiac death.[Figure caption and citation for the preceding image starts]: Anatomical location of accessory pathways across the valve annuliFrom the collection of Dr Mithilesh K. Das [Citation ends].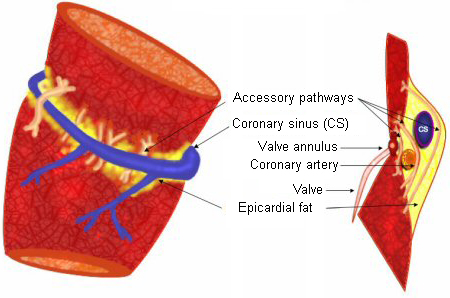 [Figure caption and citation for the preceding image starts]: Common locations of accessory pathways across the mitral and tricuspid annuliFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Common locations of accessory pathways across the mitral and tricuspid annuliFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: Right lateral accessory pathway in a patient with Ebstein's anomalyFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Right lateral accessory pathway in a patient with Ebstein's anomalyFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: WPW syndrome in a patient with hypertrophic obstructive cardiomyopathyFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: WPW syndrome in a patient with hypertrophic obstructive cardiomyopathyFrom the collection of Dr Mithilesh K. Das [Citation ends].
Pathophysiology
Normal conduction from the atria to the ventricles occurs via the atrioventricular (AV) node (where minor physiological delay occurs) and His-Purkinje system, resulting in a normal PR interval and a narrow QRS complex. In WPW syndrome, because of the physiological delay of conduction in the AV node, conduction from the atrium reaches the adjacent ventricle initially via the accessory pathway (AP), which normally has no conduction delay, and a part of the ventricle is pre-excited, resulting in a slurred upstroke at the initiation of the QRS complex, known as the delta wave. The terminal portion of the QRS complex is narrow, as conduction via the AV node to the His-Purkinje system reaches the remainder of the ventricles.
The degree of pre-excitation depends upon the relative contributions of ventricular activation via the AP versus the His-Purkinje system. It is typically greater for patients with a right-sided AP as compared with a left free-wall AP due to the relative time differences for engaging the AP when the electrical impulse leaves the sinus node. Conduction over the AP results in shortening of the PR interval (<120 ms) and widening of the QRS complex (>110 ms) with secondary ST-T wave changes. During atrial fibrillation (AF), which occurs in up to one third of patients with WPW syndrome, rapid anterograde conduction via the AP to the ventricle may rarely cause ventricular fibrillation (VF) that may result in sudden cardiac death.
When an AP is capable of retrograde conduction only (from the ventricle to the atria), the sinus rhythm ECG is normal and no delta wave is seen (concealed AP). These APs can serve as the retrograde limb of orthodromic reciprocating tachycardia (ORT).[Figure caption and citation for the preceding image starts]: Manifest versus concealed accessory pathway. AP, accessory pathway; AV, atrioventricular; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; SA, sino-atrialFrom the collection of Dr Mithilesh K. Das [Citation ends].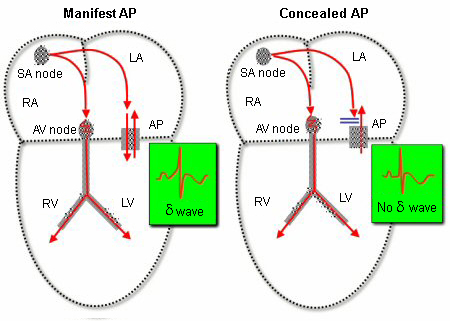 [Figure caption and citation for the preceding image starts]: Collision (fusion) of wave fronts down the atrioventricular node and accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Collision (fusion) of wave fronts down the atrioventricular node and accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
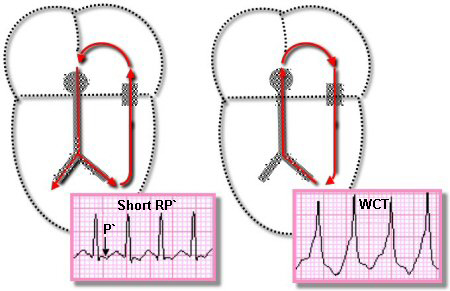
AV re-entrant tachycardia (AVRT): AVRT is the most common arrhythmia and occurs in approximately 70% to 80% of patients with WPW syndrome.[3][4] The common form of AVRT involves impulse conduction via the AV node, down the His-Purkinje system to the ventricles anterogradely, and the AP retrogradely, resulting in rapid atrial activation after ventricular depolarisation. This is known as ORT. Less commonly (5% to 10%), AVRT results from impulse conduction in a direction opposite to ORT: that is, conduction from atrium to ventricle via the AP and then from the ventricle to the atrium via the His-Purkinje system and the AV node. Therefore, it is a regular wide complex tachycardia (WCT), because ventricular activation is transmyocardial rather than via the specialised conduction tissue. This type of AVRT is known as antidromic reciprocating tachycardia (ART). ART is relatively more frequent in patients with multiple APs as compared with those with a single AP and is also relatively less common in patients with septal APs.[Figure caption and citation for the preceding image starts]: Orthodromic and antidromic atrioventricular reciprocating tachycardia circuits. WCT, wide complex tachycardiaFrom the collection of Dr Mithilesh K. Das [Citation ends].
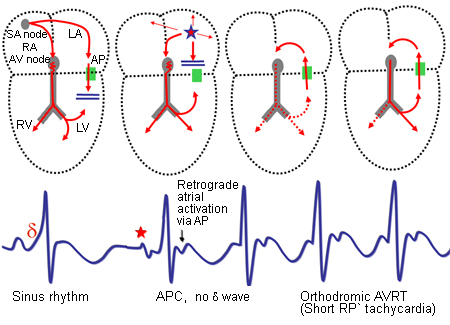
ORT: AVRT occurs in 70% to 80% of patients with WPW syndrome.[4] During ORT, the impulses reach the ventricles via the normal conduction system (AV node and His-Purkinje system) and then return to the atrium via the AP as soon as ventricular depolarisation reaches the valve annuli. Tachycardia more commonly starts after a premature atrial complex that blocks at the refractory AP but is able to conduct down the AV node to the ventricles. By this time, the AP recovers and the impulse reaches the atrium via the AP and then travels to the ventricles via the AV node, to continue as ORT. During ORT the ventricle is depolarised via the normal conduction system; ORT is a narrow complex tachycardia with a short RP interval (short RP tachycardia). [Figure caption and citation for the preceding image starts]: Orthodromic atrioventricular reciprocating tachycardia in a patient with left-sided accessory pathway. AP, accessory pathway; APC, atrial premature complex; AV, atrioventricular; AVRT, atrioventricular re-entrant tachycardia; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; SA, sino-atrialFrom the collection of Dr Mithilesh K. Das [Citation ends].
 [Figure caption and citation for the preceding image starts]: Orthodromic reciprocating tachycardia induced in a patient with left lateral accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Orthodromic reciprocating tachycardia induced in a patient with left lateral accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
ART: ART is a less common arrhythmia in patients with WPW syndrome. ART can be initiated by a premature atrial complex. The impulse is blocked at the AV node if it is refractory but conducts down the AP to the ventricles and then back to the atrium via the AV node, and then the circus movement tachycardia is initiated. Alternatively, ART can be initiated by a premature ventricular complex that blocks in the AP and conducts retrograde via the AV node. The baseline ECG (upper panel) of a patient with minimum pre-excitation and the WCT (lower panel) is an ART with negative delta wave in inferior leads and lead V1 suggestive of a right inferoseptal AP as shown here. The ART is a wide QRS tachycardia and therefore can be confused with a ventricular tachycardia (VT) or a supraventricular tachycardia with aberrancy. The baseline ECG is the key in most cases. If there is positive QRS concordance (QRS polarity positive in all precordial leads due to annular location of the APs) during ART, then this may mimic a VT. However, if there is negative concordance (QRS polarity negative in all precordial leads), then an ART is ruled out - except for a rare AVRT involving an atriofascicular pathway, which has AV node-like property that connects the tricuspid annulus to the distal right bundle and results in a left bundle branch block configuration WCT.[Figure caption and citation for the preceding image starts]: Antidromic atrioventricular reciprocating tachycardia in a patient with left-sided accessory pathway. AP, accessory pathway; APC, atrial premature complex; AV, atrioventricular; AVRT, atrioventricular re-entrant tachycardia; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; SA, sino-atrial; SVT, supraventricular tachycardiaFrom the collection of Dr Mithilesh K. Das [Citation ends].
 [Figure caption and citation for the preceding image starts]: Antidromic reciprocating tachycardia in a patient with right posteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Antidromic reciprocating tachycardia in a patient with right posteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
AF: AF is encountered in 10% to 35% of patients with WPW syndrome. AF with rapid conduction via the AP is recognised by an irregular WCT with a varying degree of ventricular pre-excitation. Patients with a rapidly conducting AP or multiple APs are at a risk for VF due to rapid ventricular stimulation. [Figure caption and citation for the preceding image starts]: Atrial fibrillation in a patient with WPW syndrome with rapid ventricular rate; resulted in aborted sudden cardiac deathFrom the collection of Dr Mithilesh K. Das [Citation ends].

Atrial flutter and atrial tachycardia: Atrial flutter and atrial tachycardia can result in a regular pre-excited WCT. Atrial flutter is encountered in 5% to 10% of patients with WPW syndrome. If the conduction is rapid, then rapid stimulation of ventricle can also result in VF. AV nodal Wenckebach pattern over the AV node or the AP in atrial flutter and AF can result in an irregular WCT. [Figure caption and citation for the preceding image starts]: Atrial flutter with pre-excitationFrom the collection of Dr Mithilesh K. Das [Citation ends].
Classification
Manifest AP versus concealed AP
Accessory pathways (APs) in WPW syndrome are usually capable of conducting bidirectionally (atrium to ventricle and ventricle to atrium). When an AP is capable of conducting retrogradely only (from the ventricle to the atria), the sinus rhythm ECG is normal and no delta wave is seen (concealed AP).[Figure caption and citation for the preceding image starts]: Manifest versus concealed accessory pathway. AP, accessory pathway; AV, atrioventricular; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; SA, sino-atrialFrom the collection of Dr Mithilesh K. Das [Citation ends].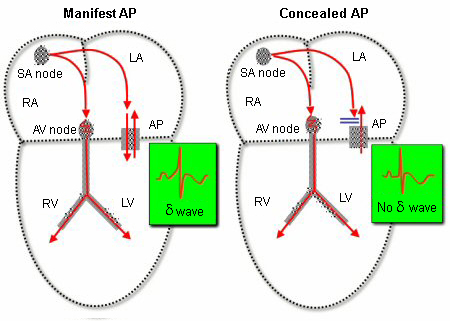 These APs serve as a substrate for re-entry and can cause a supraventricular tachycardia (SVT) involving the AV node as the other connection between the atrium and the ventricle. This type of SVT is termed atrioventricular re-entrant tachycardia (AVRT). An increased risk of sudden cardiac death is observed in patients with antegradely conducting APs but not in those with concealed APs.[3]
These APs serve as a substrate for re-entry and can cause a supraventricular tachycardia (SVT) involving the AV node as the other connection between the atrium and the ventricle. This type of SVT is termed atrioventricular re-entrant tachycardia (AVRT). An increased risk of sudden cardiac death is observed in patients with antegradely conducting APs but not in those with concealed APs.[3]
Asymptomatic/symptomatic patients
Symptomatic patients are those with episodes of tachycardia. The severity of symptoms can vary widely based on the frequency of episodes, whether they self-terminate, and the rate of the tachycardia. In general, faster tachycardias result in more severe symptoms than slower tachycardias. Tolerance is related to the rate of SVT as well as the patient's subjective experience. The decision about whether to advise electrophysiology (EP) testing and catheter ablation should be based largely on the presence of any symptoms. Because by definition all patients with WPW syndrome are symptomatic (as opposed to asymptomatic with pre-excitation on ECG) they should all be referred for baseline diagnostic EP testing, and catheter ablation should be offered if appropriate based on the results.
The management of patients with asymptomatic pre-excitation is comparatively more complex. It is well established that sudden cardiac death an be the first manifestation of an accessory pathway. Approximately one fifth of patients with asymptomatic pre-excitation will develop a symptomatic arrhythmia over time. And very rarely this can be sudden cardiac death. It is for this reason that the 2019 European Society of Cardiology guidelines have a large set of recommendations for managing patients with asymptomatic pre-excitation. It is recommended that an electrophysiology study (EPS) with isoproterenol should be considered to risk stratify individuals with asymptomatic pre-excitation and is recommended in individuals who are athletes or have a high risk occupation. If high risk electrophysiologic properties are identified, catheter ablation is recommended. In addition, an EPS and ablation can be considered in patients with asymptomatic pre-excitation who have an AP demonstrating low risk features on invasive or non-invasive screening.[3]
Atrioventricular re-entrant tachycardia (AVRT)
AVRT is the most common arrhythmia and occurs in approximately 70% to 80% of symptomatic patients with WPW syndrome.[4]
Orthodromic reciprocating tachycardia (ORT): during ORT, the ventricle is depolarised via the normal conduction system; ORT is a narrow complex tachycardia most commonly with a short RP interval (short RP tachycardia). [Figure caption and citation for the preceding image starts]: Orthodromic atrioventricular reciprocating tachycardia in a patient with left-sided accessory pathway. AP, accessory pathway; APC, atrial premature complex; AV, atrioventricular; AVRT, atrioventricular re-entrant tachycardia; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; SA, sino-atrialFrom the collection of Dr Mithilesh K. Das [Citation ends].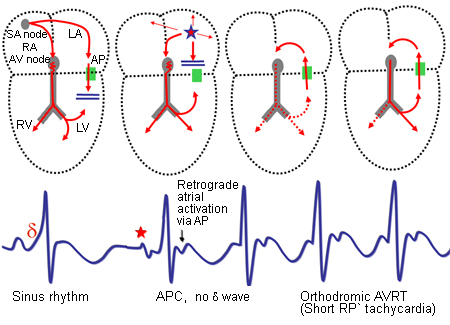 [Figure caption and citation for the preceding image starts]: Orthodromic reciprocating tachycardia induced in a patient with left lateral accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Orthodromic reciprocating tachycardia induced in a patient with left lateral accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
Antidromic reciprocating tachycardia (ART): ART is a wide QRS tachycardia, as the ventricle is depolarised via the AP. [Figure caption and citation for the preceding image starts]: Antidromic atrioventricular reciprocating tachycardia in a patient with left-sided accessory pathway. AP, accessory pathway; APC, atrial premature complex; AV, atrioventricular; AVRT, atrioventricular re-entrant tachycardia; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; SA, sino-atrial; SVT, supraventricular tachycardiaFrom the collection of Dr Mithilesh K. Das [Citation ends]. [Figure caption and citation for the preceding image starts]: Antidromic reciprocating tachycardia in a patient with right posteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
[Figure caption and citation for the preceding image starts]: Antidromic reciprocating tachycardia in a patient with right posteroseptal accessory pathwayFrom the collection of Dr Mithilesh K. Das [Citation ends].
Use of this content is subject to our disclaimer