Approach
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Cliquez ici pour les guides de pratique clinique sur l'otite moyenne aiguë et leur mise en œuvre dans le contexte belgePublished by: ebpracticenet adminLast published: 2024Acute otitis media (NL versie)Published by: ebpracticenet adminLast published: 2024Acute otitis media (AOM) can be present with a spectrum of signs and symptoms as the disease develops. However, the key factors in the history that support the diagnosis of AOM vary depending on the age of the patient. In an older, verbal child they include a preceding viral respiratory illness followed by the acute onset of otalgia. In a pre-verbal child, the key factors should include fever or systemic symptoms indicative of otalgia such as irritability, crying, sleep disturbance, vomiting, or poor appetite. Pre-verbal children may tug, rub or hold the affected ear, though these symptoms are not specific to the diagnosis of AOM.[19]
AOM occurs much less frequently in adults than in children. Adults typically seek care more quickly than children with complaints of ear pain, decreased hearing, sore throat, and otorrhoea. Adults have higher rates of persistent middle ear effusions or infections 2 months after initial diagnosis compared with children.[20] Bacteriology and treatment are similar to those for children.
Examination
Factors in the physical examination that support the diagnosis of AOM specifically include a bulging, opaque tympanic membrane.[21][22] The tympanic membrane may appear white, yellow, pink or red.[Figure caption and citation for the preceding image starts]: Otoscopy appearance of a bulging, erythematous tympanic membrane and absent landmarksFrom the personal collection of Dr Armengol [Citation ends].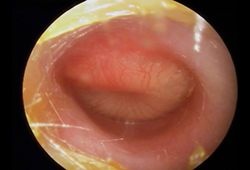
In a neutral position, a normal tympanic membrane appears draped over the umbo centrally and the lateral process of the malleus is visible in the anterosuperior quadrant. [Figure caption and citation for the preceding image starts]: Normal tympanic membrane, appearing draped over the umbo centrally, and the lateral process of the malleus in the anterosuperior quadrant. LM = lateral process of the malleus; I = incus; U = umbo; LR = light reflex; A = annulus of tympanic membrane; PI = posterior inferior quadrantFrom the personal collection of Dr Armengol [Citation ends].
In addition, a light reflex should be visible in the anteroinferior quadrant. When AOM develops, the tympanic membrane will bulge (bagel sign), obscuring these landmarks and splaying or attenuating the light reflex.[23][Figure caption and citation for the preceding image starts]: Purulent middle ear effusion and tympanic membrane with a loss of landmarks and characteristic bagel or doughnut appearanceFrom the personal collection of Dr Armengol [Citation ends].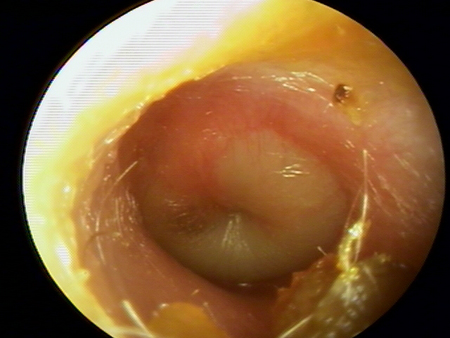
As such, examination of the external auditory canal and visualisation of the tympanic membrane are the accepted standard for the diagnosis of AOM.
On occasion, cerumen in the external auditory canal may interfere with visualisation of the tympanic membrane. Every effort should be made to clear the cerumen from the external auditory canal. If the tympanic membrane cannot be visualised, then a judgment must be made regarding the appropriate management of the patient.
Tests
Usually no tests are necessary: AOM is a clinical diagnosis. Bacterial culture is not required in most cases of AOM and no imaging is recommended for uncomplicated AOM.[24][25]
Additional tests might include pneumatic otoscopy or tympanometry to confirm the presence of an effusion.[22]
Tympanocentesis and bacterial culture of aspirated middle ear fluid are the means of making an aetiological diagnosis. However, tympanocentesis is technically difficult to perform and may require a referral to an otolaryngologist; additionally, the patient's condition is likely to have improved before culture results are available. Therefore, it is usually only performed in patients with persistent AOM unresponsive to antibiotics, or to provide immediate relief of severe pain. A mini-tipped swab of fluid draining from the middle ear cavity via established myringotomy or otorrhoea may also be considered, after cleaning the ear canal.[24]
Use of this content is subject to our disclaimer