Differentials
Common
Idiopathic dilated cardiomyopathy
History
symptoms of cardiac failure (shortness of breath on exertion, orthopnoea, fatigue, chest pain or pressure, paroxysmal nocturnal dyspnoea, abdominal discomfort, leg swelling), family history of cardiomyopathy
Exam
signs of cardiac failure (S3 gallop during rapid ventricular phase of diastole may indicate ventricular dilatation; jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly)
1st investigation
- ECG:
often non-specific findings; low limb lead voltage along with precordial criteria for left ventricular hypertrophy, and a wide QRS complex/left bundle branch block seen in idiopathic dilated cardiomyopathy; P wave abnormalities indicating atrial enlargement
More - CXR:
enlarged cardiac silhouette
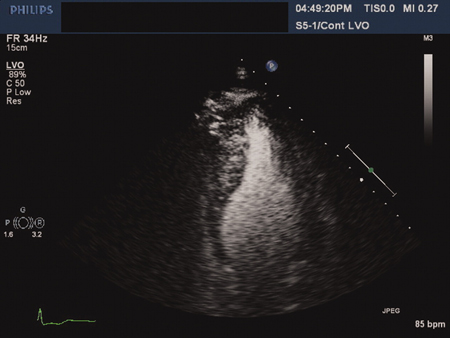
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; poor systolic function with diminished stroke volume and low ejection fraction; 4-chamber cardiac enlargement
- FBC:
low Hb or haematocrit levels in anaemia
More - B-type natriuretic peptide:
elevated in heart failure
More
Other investigations
Myocarditis
History
history of recent or known infection, which may be viral (e.g., coxsackievirus, cytomegalovirus [CMV], herpes, adenovirus, parvovirus, HIV, severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]), bacterial (meningococcus, psittacosis, streptococcal), rickettsial (typhus, Rocky Mountain spotted fever), fungal (e.g., aspergillosis, candidiasis), or parasitic; history of recent drug use (e.g., cocaine, sulfonamides, anticonvulsants) or vaccination with SARS-CoV-2 mRNA vaccine; chest pain, exertional dyspnoea, fatigue, syncope, or palpitations
Exam
signs related to underlying cause, plus signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly) and/or tachyarrhythmias, and/or cardiogenic shock
1st investigation
- ECG:
ST-T changes, ventricular tachyarrhythmias
- echocardiogram:
left ventricular dilatation and/or segmental wall motion abnormalities
Other investigations
- serology:
may be positive for infective organism (e.g., parvovirus, HIV, Lyme)
- cardiac MRI:
may show areas of abnormal signal intensity in regions of active myocarditis
- endomyocardial biopsy:
may be positive for CMV, adenovirus, coxsackievirus, parvovirus, or human herpes virus
More
Alcohol: dilated cardiomyopathy
History
history of excessive alcohol consumption; may be diagnosed as idiopathic if alcohol history is not apparent
Exam
signs of liver disease (spider naevi, clubbing, jaundice, hepatomegaly); signs of cardiac failure due to systolic dysfunction (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly)
1st investigation
- ECG:
non-specific ST-T wave changes, atrial fibrillation
More - CXR:
enlarged cardiac silhouette
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
Other investigations
- liver function tests:
may be elevated, particularly gamma-glutamyl transferase
- serum albumin:
low albumin if hepatic synthetic function impaired
- coagulation profile:
may be abnormal if hepatic synthetic function impaired
Uncommon
Hypertrophic cardiomyopathy (HCM)
History
often presents during adolescence; sudden cardiac death can be presenting sign; dyspnoea most common symptom; lightheadedness, pre-syncope or syncope, angina, palpitations; family history of sudden cardiac death or diagnosed HCM
Exam
late systolic murmur at the left sternal border, with a crescendo-decrescendo pattern at the apex and left sternal border; holosystolic murmur of mitral regurgitation may be heard at apex; jugular venous pulse with prominent 'a' wave; S4 gallop
1st investigation
- ECG:
left ventricular hypertrophy often present; pathological Q waves and ST-T wave changes common; P wave abnormalities indicating atrial enlargement
- CXR:
enlarged cardiac silhouette
- echocardiogram:
hallmark sign is left ventricular hypertrophy; there may be evidence of delayed ventricular relaxation pattern/diastolic dysfunction; systolic dysfunction representing end-stage disease may develop; left atrial enlargement; aortic valve notching
More
Other investigations
- cardiac MRI:
apical or other localised areas of hypertrophy may be more readily seen on cardiac MRI than on conventional echocardiography; functional cardiac MRI may be used to assess left ventricular outflow tract obstruction (LVOT), thickness of septum and presence of anterior motion of mitral valve during systole, as well as extent of fibrosis on late gadolinium enhancement
- cardiac catheterisation:
LVOT; pull-back catheterisation may be used to assess pressure gradient between apex and aorta; falsely elevated left ventricular pressures may be seen due to entrapment of the catheter during systole; Brockenbrough-Braunwald-Morrow sign
More - endomyocardial biopsy (more commonly done at autopsy in the case of a sudden death):
myocardial hypertrophy and disorganisation of muscle bundles in a whorled pattern; diffuse fibrosis of the walls of the heart, with somewhat increased fibrosis observed in intraventricular septum; intramural coronary artery arterial wall thickening and decreased lumen size may be seen
More
Idiopathic restrictive cardiomyopathy
History
may be asymptomatic or present with symptoms of cardiac failure (shortness of breath on exertion, orthopnoea, fatigue, chest pain or pressure, paroxysmal nocturnal dyspnoea, abdominal discomfort, leg swelling); family history of cardiomyopathy
Exam
may have signs of heart failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly)
1st investigation
- ECG:
findings may suggest a secondary cause for the cardiomyopathy
More - CXR:
findings may suggest a secondary cause for the cardiomyopathy
More - echocardiogram:
normal or small reduction in left ventricular diastolic diameter; bi-atrial enlargement; restrictive diastolic dysfunction; normal appearance of pericardium
More - B-type natriuretic peptide:
elevated
More
Other investigations
- cardiac MRI:
useful in distinguishing between constrictive pericarditis and restrictive cardiomyopathy; in constrictive pericarditis the pericardium may appear to be calcified or thickened, which is not typically present in restrictive cardiomyopathy
More - cardiac catheterisation:
similar haemodynamic findings to constrictive pericarditis, but higher left ventricular than right ventricular filling pressures are more suggestive of restrictive cardiomyopathy when the diagnosis is in question.
Arrhythmogenic right ventricular cardiomyopathy (ARVC)
History
male predominance; first presentation often in adolescence; family history of sudden cardiac death or ARVC; chest pain, palpitations, dizziness, fatigue, dyspnoea, syncope, or sudden cardiac death after physical exertion
Exam
may be normal; S3, S4, or split S2 may be present
1st investigation
- ECG:
may have abnormal repolarisation with T wave inversion present in leads V1-V3; an epsilon wave (small amplitude potentials at end of QRS); ventricular ectopy or recurrent monomorphic ventricular tachycardia with left bundle branch block pattern
- echocardiogram:
right ventricular dilatation; aneurysmal projections from right ventricular wall
- B-type natriuretic peptide:
elevated
More
Other investigations
- cardiac MRI:
increased signal intensity of right ventricular free wall on T1-weighted images representing fatty infiltration; thinning and akinesis/aneurysms of right ventricular free wall/triangle of dysplasia; left ventricular involvement is increasingly recognised
- cardiac catheterisation:
right ventricular enlargement; right ventricular wall motion abnormalities; normal coronary artery anatomy
More - endomyocardial biopsy:
fibro-fatty replacement of myocardium
More - exercise stress test:
exercise-related ventricular tachyarrhythmias
- ambulatory monitoring:
spontaneous ventricular tachyarrhythmias
- signal-averaged ECG:
a late potential may be present
Brugada syndrome and other ion channelopathies
History
syncope, palpitations, and cardiac arrest are common presentations; Brugada syndrome: may have family history of Brugada syndrome or unexplained cardiac death, can be asymptomatic, may have a history of febrile illness, illicit drug or alcohol use, or use of sodium channel blockers or psychotropic drugs
Exam
often non-specific to causes of syndrome and unremarkable arrhythmia; may be an incidental finding on ECG
1st investigation
Other investigations
- drug provocation test with sodium channel blocker:
may unmask ECG findings in Brugada syndrome
- electrophysiological study:
inducible arrhythmia
- genetic testing for Brugada syndrome:
positive for known pathogenic mutation associated with Brugada syndrome (e.g., SCN5A)
- advanced cardiac imaging (MRI or CT):
in Brugada syndrome, may demonstrate cardiac structural changes, particularly in the right ventricular outflow tract
Conduction system disease
History
patients may present with syncope or sudden death; there may be other features of cardiomyopathy or structural heart disease resulting in heart failure; in some cases, there may be features of an associated neuromuscular disease
Exam
exclude associated neuromuscular diseases
1st investigation
- ECG:
prolonged PR, QRS, or QT intervals with evidence of bundle branch block or high-grade atrioventricular block
- ambulatory monitoring:
evidence of high-grade atrioventricular block
Mitochondrial disorders
History
present with a wide range of symptoms relating to the organ systems affected; the more common conditions, which may have cardiac manifestations, include the Kearns-Sayre syndrome and myopathy, lactic acidosis, and stroke-like-episodes (MELAS) syndrome
Exam
findings depend on the specific organ systems involved
1st investigation
- clinical evaluation:
diagnosis depends on a high index of clinical suspicion in patients with multisystem involvement, exercise tolerance that is out of keeping with cardiac imaging (e.g., poor cardiopulmonary stress testing with early achievement of anaerobic threshold), or an unusual pattern of inheritance (i.e., maternal if there is a mitochondrial mutation); tests are guided by clinical presentation
- cardiopulmonary exercise testing:
elevated ventilatory equivalent for oxygen (VE/VO2) at peak exercise
More
Takotsubo syndrome
History
usually affects older women; history of recent physical/psychological stress, chest pain, dyspnoea; similar presentation to anterior myocardial infarction
Exam
may be signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly)
1st investigation
- echocardiogram:
apical ballooning of left ventricle
Other investigations
- cardiac catheterisation:
normal coronary vessels
More - cardiac MRI:
may show apical ballooning without scarring in the apical segments, distinguishing this from left anterior descending artery territory infarction
Peripartum: dilated cardiomyopathy
History
most common in obese, multiparous women >30 years of age, with preeclampsia, towards the end of pregnancy or in the months following delivery; presents with fatigue, shortness of breath
Exam
may be signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly)
1st investigation
- ECG:
non-specific ST-T wave changes or bundle branch block; P wave abnormalities indicating atrial enlargement
More - CXR:
enlarged cardiac silhouette
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
Other investigations
Tachycardia-induced: dilated cardiomyopathy
History
history of structural heart disease with decreased left ventricular function, particularly idiopathic dilated cardiomyopathy and a tachyarrhythmia; can affect any age group including children; evidence of underlying cause for tachyarrhythmia such as thyrotoxicosis
Exam
rapid, irregular pulse rate; features of cardiac failure due to systolic dysfunction (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly)
1st investigation
- ECG:
evidence of underlying atrial or ventricular tachyarrhythmias, which lead to the condition
More - CXR:
enlarged cardiac silhouette
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
More
Other investigations
Amyloidosis: hypertrophic or restrictive cardiomyopathy
History
history of and symptoms of amyloidosis and cardiac failure (e.g., fatigue, weight loss, shortness of breath on exertion, orthopnoea, fatigue, chest pain or pressure), palpitations, syncope
Exam
signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly), arrhythmias; specific features suggestive of amyloid include periorbital purpura and macroglossia
1st investigation
- ECG:
may show conduction abnormalities, low QRS voltage compared with muscle mass
- echocardiogram:
speckled appearance of myocardium (although can occur in end stage kidney disease), normal or small reduction in left ventricular ejection fraction; bi-atrial enlargement (with right atrial pressure > 10 mmHg); restrictive diastolic dysfunction; normal appearance of pericardium, but presence of effusion together with other signs supports diagnosis; longitudinal strain quantification
More - B-type natriuretic peptide:
elevated
More
Other investigations
- serum and urine protein electrophoresis with immunofixation:
monoclonal immunoglobulin light chain spike
More - rectal biopsy:
amyloid on Congo red stain; for immunohistology and genotyping
More - endomyocardial biopsy:
amyloid on Congo red stain; gold standard test
- cardiac MRI:
diffuse decrease in T1 and T2 signal intensity of the myocardium, due to infiltration with amyloid protein; global sub-endocardial late gadolinium enhancement
More - bone scan:
unique myocardial uptake pattern in ATTR cardiac amyloidosis by scintigraphy with 99mTechnetium (Tc)-bisphosphonate derivatives
More - cardiac catheterisation:
absolute myocardial blood flow and coronary flow reserve are substantially reduced
More - genetic testing:
may demonstrate transthyretin mutations
Haemochromatosis: restrictive or dilated cardiomyopathy
History
history of haemochromatosis and related symptoms (e.g., fatigue, arthralgias, sexual dysfunction), symptoms of cardiac failure (shortness of breath on exertion, orthopnoea, fatigue, chest pain or pressure, paroxysmal nocturnal dyspnoea, abdominal discomfort, leg swelling), palpitations, syncope
Exam
signs of haemochromatosis (e.g., skin bronzing), signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly) and/or arrhythmias
1st investigation
- ECG:
decreased QRS amplitude and flattened/inverted T waves; arrhythmias
- echocardiogram:
either signs of mixed dilated-restrictive or dilated cardiomyopathy
Other investigations
- cardiac MRI:
iron depositions in sub-epicardial regions
More - serum iron studies:
elevated ferritin >449 picomoles/L (>200 micrograms/L); elevated transferrin saturation; ferritin also acts as an acute phase reactant and levels may be elevated due to other acute illnesses
More - liver biopsy:
elevated hepatic iron concentration
More - endomyocardial biopsy:
increased iron concentration
Fabry disease: hypertrophic or restrictive cardiomyopathy
History
rare; symptoms begin in adolescence, burning pain in arms and legs, ocular involvement with vortex keratopathy, renal insufficiency and failure, fatigue; cardiac-predominant variant may present in middle life
Exam
rash in swimming-trunk distribution; cornea verticillata (whorl-like epithelial deposits); anhidrosis
1st investigation
Other lysosomal storage disease
History
symptoms vary depending on the underlying disorder (e.g., Gaucher's, Niemann-Pick's, Hunter-Hurler, Pompe's syndromes)
Exam
signs variable depending on the underlying disorder (e.g., Gaucher's, Niemann-Pick's, Hunter-Hurler, Pompe's syndromes)
1st investigation
Other investigations
- enzyme and/or substrate assays:
altered activity or levels, depending on specific enzyme deficiency
- genetic testing:
may show mutation
Doxorubicin: dilated cardiomyopathy
History
recent administration of doxorubicin, usually occurs 1-8 weeks after the final dose; age >70 years and pre-existing cardiac disease may increase risk
Exam
features of cardiac failure due to systolic dysfunction (crackles at the lung bases, peripheral oedema, jugular venous distension, hepatomegaly)
1st investigation
- ECG:
non-specific ST-T wave changes
More - CXR:
enlarged cardiac silhouette
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
More
Other investigations
- endomyocardial biopsy:
vacuolar degeneration and interstitial oedema; no inflammatory changes; histopathological grade corresponds to cumulative dose of doxorubicin
Heavy metals/chemicals: dilated cardiomyopathy
History
exposure to cobalt, occupational exposure to heavy metals, use of herbal medicines, nausea and vomiting with heavy metal ingestion
Exam
horizontal lines across the fingernails, neurological impairment, features of cardiac failure due to systolic dysfunction (crackles at the lung bases, peripheral oedema, jugular venous distension and hepatomegaly)
1st investigation
- ECG:
non-specific ST-T wave changes
More - CXR:
enlarged cardiac silhouette
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
Other investigations
- FBC/blood film:
basophilic stippling with arsenic or lead ingestion; may show anaemia
- serum chemistries:
renal failure may be seen with heavy metal poisoning
Diabetes mellitus
History
history of diabetes mellitus; polyuria, polydipsia if undiagnosed; symptoms of cardiac failure (shortness of breath on exertion, orthopnoea, fatigue, chest pain or pressure, paroxysmal nocturnal dyspnoea, abdominal discomfort, leg swelling) important to exclude associated coronary heart disease in patients with diabetes mellitus who present with a suspected cardiomyopathy
Exam
signs of complications from diabetes: peripheral vascular disease, ulceration, diabetic retinopathy; signs of cardiac failure: jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly
1st investigation
Other investigations
- fasting plasma glucose:
>6.9 mmol/L (125 mg/dL)
- HbA1c:
≥48 mmol/mol (6.5%)
Thyroid dysfunction: dilated cardiomyopathy
History
tachycardia, palpitations, shortness of breath, paroxysmal nocturnal dyspnoea, heat/cold intolerance, weight loss/gain, lethargy, hyperdefecation/constipation, depression
Exam
signs of hyperthyroidism: tachycardia, weight loss, tremor; signs of hypothyroidism: thinning of hair, numbness in fingers and dry skin; signs of cardiac failure: jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly
1st investigation
Other investigations
- thyroid function tests:
elevated free T3 and/or free T4 with suppressed thyroid-stimulating hormone (TSH) in hyperthyroidism; elevated TSH in primary hypothyroidism
- thyroid uptake and scan:
increased uptake in region of excess T4 production in instances of Graves' disease or toxic nodular goitre
More
Acromegaly: hypertrophic or dilated cardiomyopathy
History
shortness of breath, chest pain, orthopnoea, paroxysmal nocturnal dyspnoea; deep voice and slowing of speech; acromegaly can be asymptomatic
Exam
enlargement of hands, feet, nose, and ears with a prominent brow and jaw; signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly)
1st investigation
Noonan syndrome: hypertrophic cardiomyopathy
History
may be found in conjunction with other cardiac anomalies such as pulmonary valve stenosis and septal defects, problems with language and speech, normal intelligence in the majority of patients, puberty may be delayed by up to 2 years, hearing loss in some
Exam
eye signs (downward sloping, ptosis, wide set), undescended testes, short stature, pectus excavatum
1st investigation
- ECG:
left ventricular hypertrophy and left-axis deviation often present; ST-T wave changes common; P wave abnormalities indicating atrial enlargement
- CXR:
enlarged cardiac silhouette
- echocardiogram:
left ventricular hypertrophy and pulmonary stenosis
Other investigations
- karyotype analysis/genetic tests:
normal karyotype/mutations have been reported in PTPN11, KRAS, and other genes
More
Lentiginosis: hypertrophic cardiomyopathy
History
abnormalities of genitalia; hearing loss (sensorineural)
Exam
numerous pigmented skin lesions (lentigines), pectus excavatum, hypertelorism
1st investigation
- ECG:
left ventricular hypertrophy and left-axis deviation often present; ST-T wave changes common; conduction defects are also common
- CXR:
enlarged cardiac silhouette
- echocardiogram:
concentric left ventricular hypertrophy
Other investigations
Thiamine deficiency (wet beriberi): dilated cardiomyopathy
History
chest pain, palpitations, ankle swelling, anxiety, mental impairment, poor appetite, abdominal pain, alcohol dependency, poor diet or oral intake
Exam
jugular venous distension, peripheral oedema, tachycardia (signs of high-output cardiac failure), peripheral neuropathy, high blood pressure, cyanosis
1st investigation
- ECG:
sinus tachycardia and non-specific ST-T wave changes
More - CXR:
enlarged cardiac silhouette
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
Friedreich's ataxia/muscular dystrophy: hypertrophic and dilated cardiomyopathy
History
stumbling and falls, muscle weakness, drooping eyelids, visual and hearing loss, speech difficulties
Exam
loss of proprioception distally, nystagmus, scoliosis
1st investigation
- ECG:
left ventricular hypertrophy and T wave changes, atrial fibrillation
- CXR:
enlarged cardiac silhouette
- echocardiogram:
concentric left ventricular hypertrophy is common
Other investigations
- electromyography:
reduced sensory and motor potentials in Friedreich's ataxia
Deficiency of iron, niacin, selenium, or vitamin D: dilated cardiomyopathy
History
poor nutrition; risk factors for iron deficiency anaemia (heavy menstrual cycles, gastrointestinal losses); history of bowel pathology (malabsorption); fatigue, shortness of breath, unusual food cravings (pica due to iron deficiency)
Exam
signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly) pale mucous membranes (suggesting anaemia)
1st investigation
- ECG:
non-specific ST-T wave changes
More - CXR:
enlarged cardiac silhouette
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
Other investigations
- serum selenium levels:
may be low
- serum iron studies:
low iron and ferritin levels in iron deficiency
- FBC:
Hb low in iron deficiency
- serum vitamin D levels:
may be low
Systemic lupus erythematosus: dilated cardiomyopathy
History
fatigue, rash, myalgia, arthritis, painless haematuria
Exam
butterfly rash, discoid rash, heart murmur (Libman-Sacks endocarditis), features of biventricular failure; jugular venous distension, peripheral oedema, hepatomegaly, crackles at lung bases
1st investigation
- ECG:
variable non-specific findings
More - CXR:
enlarged cardiac silhouette, pleural effusions, infiltrates
More - echocardiogram:
normal or decreased wall thickness; poor wall thickening in systole; left ventricular dilatation in a spherical pattern; diminished stroke volume on Doppler echocardiography, with low ejection fraction; 4-chamber cardiac enlargement
Other investigations
- serum antinuclear antibody test:
usually positive
- serum anti-Smith and anti-double stranded-DNA antibodies:
usually positive
More - activated PTT levels:
may be prolonged if antiphospholipid antibodies are present
- urinalysis:
haematuria, casts, or proteinuria may be present, indicating renal involvement
Endomyocardial fibrosis/Loeffler endocarditis (hypereosinophilic syndrome)
History
majority of cases occur following travel to tropical regions within 15° of the equator; Loeffler endocarditis may occur without precedent travel; women and children more commonly affected; symptoms depend on which chambers of the heart are affected; may include shortness of breath (left ventricle) or peripheral oedema (right ventricle)
Exam
dependent on the heart chamber affected: jugular venous distension, oedema and ascites possible with right ventricular fibrosis; signs of pulmonary congestion (e.g., crackles, rales) with left ventricular fibrosis
1st investigation
- FBC:
>600 cells/mL peripheral blood eosinophils in hypereosinophilic syndrome
- CXR:
may demonstrate atrial enlargement; ventricles usually normal size
- ECG:
may show a variety of abnormalities including ST segment changes, abnormal P waves and atrial fibrillation
More - echocardiogram:
may demonstrate a pericardial effusion or fibrosis
Other investigations
- cardiac MRI:
may demonstrate endomyocardial fibrosis
- endomyocardial biopsy:
reactive fibrosis and thrombosis
More
Sarcoidosis
History
history of sarcoidosis, and/or features of the condition (e.g. dry cough, eye symptoms of dryness, blurred vision, and red eye); progressive symptoms of cardiac failure (shortness of breath on exertion, orthopnoea, fatigue, chest pain or pressure, paroxysmal nocturnal dyspnoea, abdominal discomfort, leg swelling), palpitations, syncope
Exam
signs of cardiac failure (jugular venous distension, peripheral oedema, basal crackles on lung auscultation, hepatomegaly), pansystolic murmur, arrhythmias, lymph node enlargement, erythema nodosum
1st investigation
- CXR:
may show lymph node enlargement (typically bilateral hilar or mediastinal nodal enlargement); less common features include a ground-glass appearance of the lungs and small pleural effusions
- serum angiotensin converting enzyme (ACE) level:
may be elevated
More - ECG:
may show prolonged PR interval; higher degrees of heart block may be present
More
Other investigations
- pulmonary function tests:
restrictive pattern, or obstructive or mixed pattern
- lymph node biopsy:
non-caseating granulomas
- transbronchial lung biopsy:
non-caseating granulomas
More - cardiac MRI:
may show inflammatory changes
More - echocardiogram:
may be normal or show left ventricular dysfunction
More - endomyocardial biopsy:
granulomatous involvement, often patchy
More
Electrolyte disorders
History
symptoms will depend on the nature/cause of the electrolyte abnormality
Exam
signs will depend on the nature/cause of the electrolyte abnormality
1st investigation
- serum metabolic panel:
may show low potassium, calcium, phosphate, or magnesium levels
More - ECG:
hypokalaemia: may show ST segment depression, decreased amplitude of T waves, U waves; hypocalcaemia/hypomagnesaemia: may show prolonged QT interval
Other investigations
- echocardiogram:
performed for signs of cardiomyopathy; rarely may show evidence of left ventricular dysfunction
Use of this content is subject to our disclaimer