History and exam
Key diagnostic factors
common
presence of risk factors
Anyone can develop an adverse cutaneous reaction to a drug. Key risk factors to certain drugs or reactions include history of hereditary angio-oedema (allergic type I reactions), cytomegalovirus and Epstein-Barr virus infections or lymphoid malignancy (ampicillin and amoxicillin rash), HIV infection (hypersensitivity to sulfonamides and related compounds), HLA-B*5701 polymorphism (abacavir-induced skin hypersensitivity reactions), HLA-B*1502 polymorphism (carbamazepine-induced skin hypersensitivity reactions), and HLA-B*5801 polymorphism (allopurinol-induced skin reactions).
history of drug exposure
Exposure to a drug within the previous few minutes or hours (acute allergic reactions) or up to 2 weeks before suggests the possibility of a drug-induced lesion.
Any drug can cause an allergic reaction; commonly implicated are beta-lactam antibiotics, non-selective non-steroidal anti-inflammatory drugs, muscle relaxants used in anaesthesia, sulfonamides and structurally related drugs, contrast media, and gelatins.
skin lesions
Adverse drug reactions can cause any type of skin lesion. Common adverse skin reactions to systemic drugs include maculopapular skin reactions; urticaria and angio-oedema; the spectrum of skin lesions encompassing erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis; and fixed drug eruptions. Together these account for the majority of all drug-induced eruptions. More severe reactions, such as toxic epidermal necrolysis and drug hypersensitivity syndrome, can initially present as morbilliform eruptions.
Macroscopic appearances of drug-induced skin lesions are indistinguishable from those of non-drug-induced lesions.[Figure caption and citation for the preceding image starts]: Drug exanthem due to phenytoinPhotography courtesy of Brian L. Swick [Citation ends]. [Figure caption and citation for the preceding image starts]: Typical lesions seen in acute or chronic urticariaFrom the personal collection of Stephen Dreskin, MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Typical lesions seen in acute or chronic urticariaFrom the personal collection of Stephen Dreskin, MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Angio-oedema of the lips in a patient who also has urticariaFrom the personal collection of Stephen Dreskin, MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Angio-oedema of the lips in a patient who also has urticariaFrom the personal collection of Stephen Dreskin, MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Palmar target lesions in erythema multiformeFrom the personal collection of Nanette Silverberg, MD, FAAD, FAAP [Citation ends].
[Figure caption and citation for the preceding image starts]: Palmar target lesions in erythema multiformeFrom the personal collection of Nanette Silverberg, MD, FAAD, FAAP [Citation ends]. [Figure caption and citation for the preceding image starts]: Blistering targetoid lesions on the trunk, carbamazepine induced Stevens-Johnson syndromeKhoo AB, Ali FR, Yiu ZZ, et al. Carbamazepine induced Stevens-Johnson syndrome. BMJ Case Rep. 2016;2016. pii: bcr2016214926. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Blistering targetoid lesions on the trunk, carbamazepine induced Stevens-Johnson syndromeKhoo AB, Ali FR, Yiu ZZ, et al. Carbamazepine induced Stevens-Johnson syndrome. BMJ Case Rep. 2016;2016. pii: bcr2016214926. Used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Stevens-Johnson syndrome: epidermal loss on soles of feetFrom the personal collection of Areta Kowal-Vern, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Stevens-Johnson syndrome: epidermal loss on soles of feetFrom the personal collection of Areta Kowal-Vern, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Initial phase of toxic epidermal necrolysis with diffuse erythema and vesicles that will evolve to full epidermal necrosisFerrandiz-Pulido C, Garcia-Patos V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch Dis Child. 2013;98:998-1003. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Initial phase of toxic epidermal necrolysis with diffuse erythema and vesicles that will evolve to full epidermal necrosisFerrandiz-Pulido C, Garcia-Patos V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch Dis Child. 2013;98:998-1003. Used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: A 5-year-old female patient with toxic epidermal necrolysis with three suspected drugs (penicillin, ibuprofen, and paracetamol)Ferrandiz-Pulido C, Garcia-Patos V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch Dis Child. 2013;98:998-1003. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: A 5-year-old female patient with toxic epidermal necrolysis with three suspected drugs (penicillin, ibuprofen, and paracetamol)Ferrandiz-Pulido C, Garcia-Patos V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch Dis Child. 2013;98:998-1003. Used with permission [Citation ends].
variable skin reactions within 5 to 15 minutes of drug exposure
variable skin reactions within a few hours of drug exposure
uncommon
Other diagnostic factors
common
pruritus
Can be a symptom of an adverse drug reaction, indistinguishable from its occurrence in non-drug-induced lesions.
associated non-cutaneous features
Cutaneous drug reactions may be associated with a wide spectrum of symptoms depending on the type of reaction. These reactions include: anaphylactic reactions, erythema multiforme (including SJS [Stevens-Johnson syndrome] and TEN [toxic epidermal necrolysis]), DRESS (drug reaction with eosinophilia and systemic symptoms; also called drug hypersensitivity syndrome), acute generalised exanthematous pustulosis, and fixed drug eruptions. Atopic symptoms such as rhinitis, conjunctivitis, and respiratory wheeze may be seen. Non-specific symptoms such as nausea, vomiting, abdominal pain, and dizziness may also be seen. DRESS is associated with fever and lymphadenopathy in at least 2 sites. Blisters and mucosal involvement may be seen in fixed drug reactions and SJS/TEN.[Figure caption and citation for the preceding image starts]: Oral and mucosal ulcerations, carbamazepine induced Stevens-Johnson syndromeKhoo AB, Ali FR, Yiu ZZ, et al. Carbamazepine induced Stevens-Johnson syndrome. BMJ Case Rep. 2016;2016. pii: bcr2016214926. Used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: A 17-year-old male patient diagnosed with Stevens-Johnson syndrome due to azitromicine. Erosions and crusts on the lips with diffuse ulcers on the tongueFerrandiz-Pulido C, Garcia-Patos V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch Dis Child. 2013;98:998-1003. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: A 17-year-old male patient diagnosed with Stevens-Johnson syndrome due to azitromicine. Erosions and crusts on the lips with diffuse ulcers on the tongueFerrandiz-Pulido C, Garcia-Patos V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch Dis Child. 2013;98:998-1003. Used with permission [Citation ends].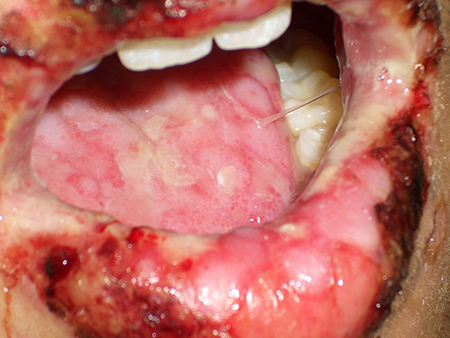
uncommon
pain
Can be a symptom of an adverse drug reaction, indistinguishable from its occurrence in non-drug-induced lesions.
Risk factors
strong
virus infections
Increased risk of the ampicillin and amoxicillin rash in patients with certain virus infections (cytomegalovirus and Epstein-Barr virus).
HIV infection
Increased risk of hypersensitivity reactions (drug reaction with eosinophilia and systemic symptoms [DRESS]; also called drug hypersensitivity syndrome), for example to sulfonamides and related compounds.
HLA-B*5701 polymorphism
Confers an increased risk of abacavir-induced skin hypersensitivity reactions. This polymorphism has a near 100% negative predictive value, and screening reduces the risk from about 10% to nearly 0%.[32]
HLA-B*1502 polymorphism
Han Chinese people with this polymorphism are at increased risk of carbamazepine-induced skin hypersensitivity reactions.[33]
HLA-B*5801 polymorphism
Han Chinese people with this polymorphism are at increased risk of allopurinol-induced skin reactions.[33]
weak
female sex
Women are slightly more likely than men to report adverse drug reactions.[34]
Use of this content is subject to our disclaimer