Endometriosis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
immediate fertility not desired: pain without endometrioma or suspected severe/deep disease
analgesia
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
combined oral contraceptive pill (OCP)
OCPs suppress the hypothalamic-pituitary-ovarian axis and subsequent oestrogen/progesterone secretion, thereby inducing atrophy of ectopic implants.
If pain is strictly related to the menstrual cycle, then continuous use of the OCP can be recommended as women may become amenorrhoeic and will experience less cyclic pain.[66]Miller L, Hughes JP. Continuous combination oral contraceptive pills to eliminate withdrawal bleeding: a randomized trial. Obstet Gynecol. 2003 Apr;101(4):653-61. http://www.ncbi.nlm.nih.gov/pubmed/12681866?tool=bestpractice.com Women should be made aware that irregular spotting is common with continuous use.
Side effects are generally mild and time-limited. Life-threatening cardiovascular adverse events are more likely to occur in women aged over 35 years, who are heavy smokers, have acquired/inherited thrombophilia, or have experienced a prior cardiovascular event. Therefore, OCPs are not recommended for these women.
There is an increasing debate on the use of OCPs as first-line therapy because of concern over oestrogenic side effects and progression of more advanced stage disease.
Consult product literature for guidance on dosage for individual preparations.
analgesia
Additional treatment recommended for SOME patients in selected patient group
May be used in combination with an oral contraceptive pill.
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
progestogen
Progesterone induces decidualisation and eventual atrophy of implants. Certain formulations also suppress the hypothalamic-pituitary-ovarian axis, resulting in decreased steroid hormone stimulation of implants. Many such women will become amenorrhoeic.[61]Brown J, Kives S, Akhtar M. Progestagens and anti-progestagens for pain associated with endometriosis. Cochrane Database Syst Rev. 2012 Mar 14;(3):CD002122. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002122.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/22419284?tool=bestpractice.com Continuous administration significantly reduces pain, whereas prescribing a luteal phase-only regimen is ineffective.
The levonorgestrel IUD is approved for long-term use, with individual devices approved for up to 5 to 6 years of use prior to exchange. The levonorgestrel IUD significantly reduces pelvic pain (up to 6 months of therapy) and the recurrence of painful periods after surgery. This effect is more dramatic in women with advanced-stage disease.[62]Gibbons T, Georgiou EX, Cheong YC, et al. Levonorgestrel-releasing intrauterine device (LNG-IUD) for symptomatic endometriosis following surgery. Cochrane Database Syst Rev. 2021 Dec 20;12:CD005072. https://www.doi.org/10.1002/14651858.CD005072.pub4 http://www.ncbi.nlm.nih.gov/pubmed/34928503?tool=bestpractice.com Serum progestin levels remain low, allowing the device to provide effective therapy without promoting a hypo-oestrogenic state. The etonogestrel-releasing subdermal implant can also be considered for long-term therapy because it lasts for 3 years.[76]Ambacher K, Secter M, Sanders AP. The use of progestin subdermal implants in the management of endometriosis-related pain symptoms and quality of life: a systematic review. Curr Med Res Opin. 2022 Mar;38(3):479-86. http://www.ncbi.nlm.nih.gov/pubmed/35048754?tool=bestpractice.com
Dienogest, an oral progestin, reduces endometriotic implants while providing similar symptomatic relief to gonadotrophin-releasing hormone (GnRH) agonists, with better quality-of-life scores.[77]Strowitzki T, Marr J, Gerlinger C, et al. Detailed analysis of a randomized, multicenter, comparative trial of dienogest versus leuprolide acetate in endometriosis. Int J Gynaecol Obstet. 2012 Jun;117(3):228-33. http://www.ncbi.nlm.nih.gov/pubmed/22459918?tool=bestpractice.com Three to 4 months of treatment may be required to see the full effect. It is not currently available in the US and some other countries, except in combination with estradiol valerate. However, this combination is sometimes used off-label for endometriosis.
Serious adverse events that occur with progestogens include decreased bone mineral density, especially with prolonged use. This effect may be more marked in adolescents, when the rate of bone mineralisation peaks. The subcutaneous form of medroxyprogesterone acetate and IUD levonorgestrel may reduce this risk.[55]Miller JD, Shaw RW, Casper RF, et al. Historical prospective cohort study of the recurrence of pain after discontinuation of treatment with danazol or a gonadotropin-releasing hormone agonist. Fertil Steril. 1998 Aug;70(2):293-6. http://www.ncbi.nlm.nih.gov/pubmed/9696224?tool=bestpractice.com [75]Petta CA, Ferriani RA, Abrao MS, et al. Randomized clinical trial of a levonorgestrel-releasing intrauterine system and a depot GnRH analogue for the treatment of chronic pelvic pain in women with endometriosis. Human Reprod. 2005 Jul;20(7):1993-8. http://humrep.oxfordjournals.org/cgi/content/full/20/7/1993 http://www.ncbi.nlm.nih.gov/pubmed/15790607?tool=bestpractice.com IUD levonorgestrel should be placed during the early proliferative phase of the menstrual cycle. Other bothersome side effects include weight gain, irregular uterine bleeding, and mood changes.
Use caution with medroxyprogesterone. Doses of subcutaneous and intramuscular formulations are different.
Primary options
medroxyprogesterone: 150 mg intramuscularly every 3 months; 104 mg subcutaneously every 3 months
OR
levonorgestrel intrauterine device: 52 mg/unit every 5 years
OR
etonogestrel subdermal implant: 68 mg/unit every 3 years
OR
estradiol valerate/dienogest: 1 tablet once daily according to product literature
OR
dienogest: 2 mg orally once daily
analgesia
Additional treatment recommended for SOME patients in selected patient group
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
gonadotrophin-releasing hormone (GnRH) antagonist
Elagolix is an oral GnRH antagonist that suppresses ovarian oestrogen production in a dose-dependent manner.[78]Carr B, Dmowski WP, O'Brien C, et al. Elagolix, an oral GnRH antagonist, versus subcutaneous depot medroxyprogesterone acetate for the treatment of endometriosis: effects on bone mineral density. Reprod Sci. 2014 Nov;21(11):1341-51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4212335 http://www.ncbi.nlm.nih.gov/pubmed/25249568?tool=bestpractice.com In the US, it is licensed for the treatment of moderate to severe endometriosis-related pain.
Two 6-month placebo-controlled phase 3 trials reported significant reductions in dysmenorrhoea and non-menstrual pelvic pain among women with endometriosis-associated pain who were randomised to elagolix.[79]Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017 May 19;377(1):28-40. https://www.doi.org/10.1056/NEJMoa1700089 http://www.ncbi.nlm.nih.gov/pubmed/28525302?tool=bestpractice.com
Hypo-oestrogenic adverse effects were similar to those of injectable GnRH agonists, and included hot flushes, increased serum lipids, and decreased bone mineral density.[79]Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017 May 19;377(1):28-40. https://www.doi.org/10.1056/NEJMoa1700089 http://www.ncbi.nlm.nih.gov/pubmed/28525302?tool=bestpractice.com
The maximum recommended duration of elagolix use is 6 to 24 months (depending on dose) to reduce the extent of bone loss.
A lower initial dose and longer treatment course (up to 24 months) is recommended in women without coexisting dyspareunia. A higher initial dose can be considered in women with coexisting dyspareunia; however, women on the higher dose should receive a shorter treatment course (up to 6 months). The dose should be adjusted to the lowest effective dose guided by the severity of symptoms.
Elagolix is contraindicated in women with severe hepatic impairment. Women with moderate hepatic impairment should only be prescribed the lower dose for up to 6 months. Women with mild impairment do not require any modifications to the recommended dose regimen.
Relugolix, another GnRH antagonist, is available in combination with estradiol and norethisterone, which are thought to reduce hypo-oestrogenic adverse effects.[80]Giudice LC, As-Sanie S, Arjona Ferreira JC, et al. Once daily oral relugolix combination therapy versus placebo in patients with endometriosis-associated pain: two replicate phase 3, randomised, double-blind, studies (SPIRIT 1 and 2). Lancet. 2022 Jun 18;399(10343):2267-79. https://www.sciencedirect.com/science/article/pii/S0140673622006225 http://www.ncbi.nlm.nih.gov/pubmed/35717987?tool=bestpractice.com In the US, it is approved for the management of moderate to severe endometriosis-related pain.
In two 6-month phase 3 trials, significantly more women who received relugolix combination therapy experienced improvements in dysmenorrhoea and non-menstrual pelvic pain compared with those who received placebo.[80]Giudice LC, As-Sanie S, Arjona Ferreira JC, et al. Once daily oral relugolix combination therapy versus placebo in patients with endometriosis-associated pain: two replicate phase 3, randomised, double-blind, studies (SPIRIT 1 and 2). Lancet. 2022 Jun 18;399(10343):2267-79. https://www.sciencedirect.com/science/article/pii/S0140673622006225 http://www.ncbi.nlm.nih.gov/pubmed/35717987?tool=bestpractice.com The least squares mean percentage loss in lumbar spine and total hip bone mineral density was less than 1% after 24 weeks. Headache, nasopharyngitis, and hot flushes were the most common adverse effects.[80]Giudice LC, As-Sanie S, Arjona Ferreira JC, et al. Once daily oral relugolix combination therapy versus placebo in patients with endometriosis-associated pain: two replicate phase 3, randomised, double-blind, studies (SPIRIT 1 and 2). Lancet. 2022 Jun 18;399(10343):2267-79. https://www.sciencedirect.com/science/article/pii/S0140673622006225 http://www.ncbi.nlm.nih.gov/pubmed/35717987?tool=bestpractice.com
The maximum recommended treatment duration for relugolix combination therapy is 24 months due to the risk for continued bone loss.
Relugolix/estradiol/norethisterone is contraindicated in patients with hepatic impairment of any severity.
Primary options
elagolix: 150 mg orally once daily for up to 24 months; women with dyspareunia: consider initiating treatment at the higher dose of 200 mg twice daily for up to 6 months; moderate hepatic impairment: 150 mg once daily for up to 6 months
OR
relugolix/estradiol/norethisterone acetate: 40 mg (relugolix)/1 mg (estradiol)/0.5 mg (norethisterone) orally once daily for up to 24 months
analgesia
Additional treatment recommended for SOME patients in selected patient group
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
laparoscopy
Additional treatment recommended for SOME patients in selected patient group
When to offer surgery is debatable and varies among specialists. It is usually determined by the individual clinician and woman. The patient’s symptoms, preferences and priorities regarding pain and fertility are elements that should be considered.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73 The side effects of hormonal therapy may influence the decision to proceed to surgery. For example, gonadotrophin-releasing hormone agonists and progestogens are not ideal options in adolescents due to the potential impact on bone mineral density at such a critical point in development. Therefore, laparoscopy may be preferred. Furthermore, both progestogens and androgens have bothersome side effects that may result in a preference for surgery.
Conservative surgical management with laparoscopic excision or ablation of visible implants provides effective treatment of pain-related complaints.[Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].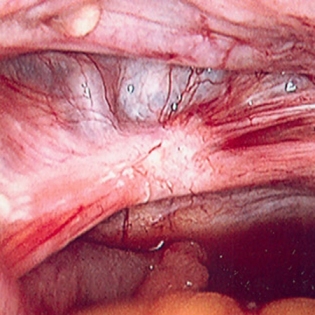 Diagnostic laparoscopy alone may impart a therapeutic response in up to 30% of women.[98]Abbott JA, Hawe J, Clayton RD, et al. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2-5 year follow-up. Hum Reprod. 2003 Sep;18(9):1922-7.
http://humrep.oxfordjournals.org/cgi/content/full/18/9/1922
http://www.ncbi.nlm.nih.gov/pubmed/12923150?tool=bestpractice.com
Several studies have established a clear relationship between surgical intervention and reduction of pain in women with endometriosis.
Diagnostic laparoscopy alone may impart a therapeutic response in up to 30% of women.[98]Abbott JA, Hawe J, Clayton RD, et al. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2-5 year follow-up. Hum Reprod. 2003 Sep;18(9):1922-7.
http://humrep.oxfordjournals.org/cgi/content/full/18/9/1922
http://www.ncbi.nlm.nih.gov/pubmed/12923150?tool=bestpractice.com
Several studies have established a clear relationship between surgical intervention and reduction of pain in women with endometriosis.
Rectal, bladder, and ureteral injury may occur because of the alterations in normal anatomy. These risks should be discussed prior to surgery. Bowel preparation facilitates these difficult procedures and should be administered to any woman undergoing operative laparoscopy.
Appendectomy should be considered in women undergoing laparoscopic surgery for suspected endometriosis if there is a complaint of right-sided pain and the appendix appears abnormal. Up to 50% of appendiceal specimens will yield abnormal pathology, but the effect on pain and future adverse outcomes is difficult to assess.[101]Berker B, Lashay N, Davarpanah R, et al. Laparoscopic appendectomy in patients with endometriosis. J Minim Invasive Gynecol. 2005 May-Jun;12(3):206-9. http://www.ncbi.nlm.nih.gov/pubmed/15922976?tool=bestpractice.com
gonadotrophin-releasing hormone (GnRH) agonist
Rapidly induce a hypo-oestrogenic state by down-regulating the hypothalamic-pituitary-ovarian axis. An initial rise in gonadotrophins and oestrogen (flare) occurs after administration, but chronic exposure provides the desired response.
Approximately 85% of women with confirmed endometriosis will experience significant reduction in pain complaints.[82]Dlugi AM, Miller JD, Knittle H. Lupron depot (leuprolide acetate for depot suspension) in the treatment of endometriosis: a randomized, placebo-controlled, double-blind study. Lupron Study Group. Fertil Steril. 1990 Sep;54(3):419-27. http://www.ncbi.nlm.nih.gov/pubmed/2118858?tool=bestpractice.com Empirical use in women with chronic pelvic pain may also be considered, regardless of the diagnosis.[83]Ling FW. Randomized controlled trial of depot leuprolide in patients with chronic pelvic pain and clinically suspected endometriosis. Pelvic Pain Study Group. Obstet Gynecol. 1999 Jan;93(1):51-8. http://www.ncbi.nlm.nih.gov/pubmed/9916956?tool=bestpractice.com One systematic review found no difference in the positive therapeutic effect of GnRH agonists when compared with other hormonal regimens.[64]Brown J, Pan A, Hart RJ. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst Rev. 2010 Dec 8;(12):CD008475. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD008475.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/21154398?tool=bestpractice.com However results of one trial suggest that GnRH agonists have similar efficacy to that of continuous oral contraceptive pills in treating endometriosis-associated pain.[86]Guzick DS, Huang LS, Broadman BA, et al. Randomized trial of leuprolide versus continuous oral contraceptives in the treatment of endometriosis-associated pelvic pain. Fertil Steril. 2011 Apr;95(5):1568-73. http://www.ncbi.nlm.nih.gov/pubmed/21300339?tool=bestpractice.com
Prolonged exposure (>6 months) can lead to an irreversible decrease in bone mineral density (BMD).[115]Shaw RW. A risk benefit assessment of drugs used in the treatment of endometriosis. Drug Saf. 1994 Aug;11(2):104-13. http://www.ncbi.nlm.nih.gov/pubmed/7945998?tool=bestpractice.com GnRH agonists may not be an ideal choice in adolescents because of the potential impact on BMD at such a critical point in development. To reduce menopausal symptoms and the effect on BMD without reducing the efficacy of pain relief, GnRH agonists should be administered with hormonal add-back therapy (e.g., norethisterone or conjugated oestrogens plus medroxyprogesterone), which should be offered from the beginning of treatment. Non-hormonal forms of add-back therapy to alleviate vasomotor symptoms include selective serotonin reuptake inhibitors, serotonin-noradrenaline (norepinephrine) reuptake inhibitors, and various herbal remedies.
GnRH agonists lack the bothersome side effects of progestogens (weight gain, irregular uterine bleeding, mood changes) and androgens (darkening facial hair, acne, oily skin, deepening of the voice, and male-pattern hair loss) and are therefore usually recommended prior to initiating these other hormonal therapies. However, they are typically less well tolerated than progestogens.
Primary options
leuprorelin: 3.75 mg intramuscularly once monthly; or 11.25 mg intramuscularly every 3 months
or
nafarelin: 200 micrograms (1 spray) in one nostril in the morning and 200 micrograms (1 spray) in the other nostril in the evening; start between days 2-4 of menstrual cycle
or
goserelin: 3.6 mg subcutaneously every 28 days
-- AND --
norethisterone: 5 mg orally once daily
or
oestrogens, conjugated/medroxyprogesterone: 0.3 mg/1.5 mg orally once daily initially, increase according to response
analgesia
Additional treatment recommended for SOME patients in selected patient group
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
laparoscopy
Additional treatment recommended for SOME patients in selected patient group
When to offer surgery is debatable and varies among specialists. It is usually determined by the individual clinician and woman. The patient’s symptoms, preferences and priorities regarding pain and fertility are elements that should be considered.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73 The side effects of hormonal therapy may influence the decision to proceed to surgery. For example, gonadotrophin-releasing hormone agonists and progestogens are not ideal options in adolescents due to the potential impact on bone mineral density at such a critical point in development. Therefore, laparoscopy may be preferred. Furthermore, both progestogens and androgens have bothersome side effects which may result in a preference for surgery.
Conservative surgical management with laparoscopic excision or ablation of visible implants provides effective treatment of pain-related complaints.[Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].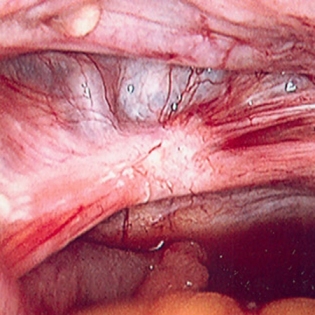 Diagnostic laparoscopy alone may impart a therapeutic response in up to 30% of women.[98]Abbott JA, Hawe J, Clayton RD, et al. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2-5 year follow-up. Hum Reprod. 2003 Sep;18(9):1922-7.
http://humrep.oxfordjournals.org/cgi/content/full/18/9/1922
http://www.ncbi.nlm.nih.gov/pubmed/12923150?tool=bestpractice.com
Several studies have established a clear relationship between surgical intervention and reduction of pain in women with endometriosis.
Diagnostic laparoscopy alone may impart a therapeutic response in up to 30% of women.[98]Abbott JA, Hawe J, Clayton RD, et al. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2-5 year follow-up. Hum Reprod. 2003 Sep;18(9):1922-7.
http://humrep.oxfordjournals.org/cgi/content/full/18/9/1922
http://www.ncbi.nlm.nih.gov/pubmed/12923150?tool=bestpractice.com
Several studies have established a clear relationship between surgical intervention and reduction of pain in women with endometriosis.
Rectal, bladder, and ureteral injury may occur because of the alterations in normal anatomy. These risks should be discussed prior to surgery. Bowel preparation facilitates these difficult procedures and should be administered to any woman undergoing operative laparoscopy.
Appendectomy should be considered in women undergoing laparoscopic surgery for suspected endometriosis if there is a complaint of right-sided pain and the appendix appears abnormal. Up to 50% of appendiceal specimens will yield abnormal pathology, but the effect on pain and future adverse outcomes is difficult to assess.[101]Berker B, Lashay N, Davarpanah R, et al. Laparoscopic appendectomy in patients with endometriosis. J Minim Invasive Gynecol. 2005 May-Jun;12(3):206-9. http://www.ncbi.nlm.nih.gov/pubmed/15922976?tool=bestpractice.com
androgen
Produce a hypo-oestrogenic state by directly suppressing the hypothalamic-pituitary-ovarian axis. Onset of amenorrhoea seems to correlate with therapeutic effect.
Clinical trials have shown that androgens (e.g., danazol) effectively reduce pain related to endometriosis when compared with placebo.[63]Farquhar C, Prentice A, Singla AA, et al. Danazol for pelvic pain associated with endometriosis. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD000068. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000068.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/17943735?tool=bestpractice.com They may also be effective post-surgical adjuncts. Improved revised American Society for Reproductive Medicine scores were noted at laparoscopy.[63]Farquhar C, Prentice A, Singla AA, et al. Danazol for pelvic pain associated with endometriosis. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD000068. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000068.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/17943735?tool=bestpractice.com However, their use is limited by adverse effects that include darkening facial hair, acne, oily skin, deepening of the voice, and male-pattern hair loss.[63]Farquhar C, Prentice A, Singla AA, et al. Danazol for pelvic pain associated with endometriosis. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD000068. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000068.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/17943735?tool=bestpractice.com [87]Hughes E, Brown J, Collins JJ, et al. Ovulation suppression for endometriosis for women with subfertility. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD000155. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000155.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/17636607?tool=bestpractice.com Furthermore, reports have linked danazol to ovarian cancer.[88]Cottreau CM, Ness RB, Modugno F, et al. Endometriosis and its treatment with danazol or lupron in relation to ovarian cancer. Clin Cancer Res. 2003 Nov 1;9(14):5142-4. http://clincancerres.aacrjournals.org/content/9/14/5142.long http://www.ncbi.nlm.nih.gov/pubmed/14613992?tool=bestpractice.com
Initial dosing schedule depends on severity of disease. Maintenance dose is achieved when women experience amenorrhoea or a reduction in pain.
Primary options
danazol: 200-800 mg/day orally given in 2 divided doses
analgesia
Additional treatment recommended for SOME patients in selected patient group
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
laparoscopy
Additional treatment recommended for SOME patients in selected patient group
When to offer surgery is debatable and varies among specialists. It is usually determined by the individual clinician and woman. The patient’s symptoms, preferences and priorities regarding pain and fertility are elements that should be considered.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73 The side effects of hormonal therapy may influence the decision to proceed to surgery. For example, gonadotrophin-releasing hormone agonists and progestogens are not ideal options in adolescents due to the potential impact on bone mineral density at such a critical point in development. Therefore, laparoscopy may be preferred. Furthermore, both progestogens and androgens have bothersome side effects which may result in a preference for surgery.
Conservative surgical management with laparoscopic excision or ablation of visible implants provides effective treatment of pain-related complaints.[Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].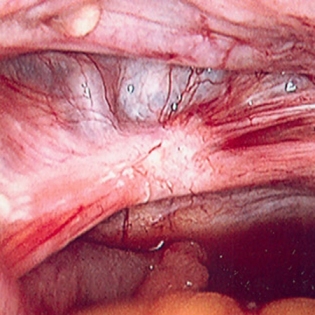 Diagnostic laparoscopy alone may impart a therapeutic response in up to 30% of women.[98]Abbott JA, Hawe J, Clayton RD, et al. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2-5 year follow-up. Hum Reprod. 2003 Sep;18(9):1922-7.
http://humrep.oxfordjournals.org/cgi/content/full/18/9/1922
http://www.ncbi.nlm.nih.gov/pubmed/12923150?tool=bestpractice.com
Several studies have established a clear relationship between surgical intervention and reduction of pain in women with endometriosis.
Diagnostic laparoscopy alone may impart a therapeutic response in up to 30% of women.[98]Abbott JA, Hawe J, Clayton RD, et al. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2-5 year follow-up. Hum Reprod. 2003 Sep;18(9):1922-7.
http://humrep.oxfordjournals.org/cgi/content/full/18/9/1922
http://www.ncbi.nlm.nih.gov/pubmed/12923150?tool=bestpractice.com
Several studies have established a clear relationship between surgical intervention and reduction of pain in women with endometriosis.
Rectal, bladder, and ureteral injury may occur because of the alterations in normal anatomy. These risks should be discussed prior to surgery. Bowel preparation facilitates these difficult procedures and should be administered to any woman undergoing operative laparoscopy.
Appendectomy should be considered in women undergoing laparoscopic surgery for suspected endometriosis if there is a complaint of right-sided pain and the appendix appears abnormal. Up to 50% of appendiceal specimens will yield abnormal pathology, but the effect on pain and future adverse outcomes is difficult to assess.[101]Berker B, Lashay N, Davarpanah R, et al. Laparoscopic appendectomy in patients with endometriosis. J Minim Invasive Gynecol. 2005 May-Jun;12(3):206-9. http://www.ncbi.nlm.nih.gov/pubmed/15922976?tool=bestpractice.com
hysterectomy
Considered the definitive treatment for symptomatic women who have persistent pain despite conservative measures, and no longer desire childbearing potential.
bilateral salpingo-oophorectomy and excision of visible peritoneal disease
Additional treatment recommended for SOME patients in selected patient group
For the best chance of cure, hysterectomy with bilateral salpingo-oophorectomy and excision of visible peritoneal disease should be offered, focusing on excising deep infiltrating lesions.[106]Namnoum AB, Hickman TN, Goodman SB, et al. Incidence of symptom recurrence after hysterectomy for endometriosis. Fertil Steril. 1995 Nov;64(5):898-902. http://www.ncbi.nlm.nih.gov/pubmed/7589631?tool=bestpractice.com The principle is based on removal of common areas of implantation along with the primary source of endogenous oestrogen production, and with a focus on excising deep infiltrating lesions. However, there is little distinction in the literature as to whether this is an effective treatment modality specifically for cyclical pain.[107]Martin DC. Hysterectomy for treatment of pain associated with endometriosis. J Minim Invasive Gynecol. 2006 Nov-Dec;13(6):566-72. http://www.ncbi.nlm.nih.gov/pubmed/17097580?tool=bestpractice.com
hormone replacement therapy (HRT)
Additional treatment recommended for SOME patients in selected patient group
Oestrogen replacement is generally warranted after hysterectomy with bilateral salpingo-oophorectomy to reduce vasomotor symptoms and risk of bone loss, especially in pre-menopausal and symptomatic post-menopausal women. HRT reduces the incidence of fracture and the risk of coronary artery disease in pre-menopausal women who undergo surgical menopause. However, there are increases in risk of breast cancer, venous thrombosis, and stroke in post-menopausal women. Therefore, risks versus benefits of HRT should be discussed with the woman before initiating treatment.
immediate fertility not desired: pain with endometrioma or suspected severe/deep disease
surgery
Ovarian endometriomas do not resolve in response to hormonal suppression and, if symptomatic, should be addressed surgically.[Figure caption and citation for the preceding image starts]: Laparoscopic image of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].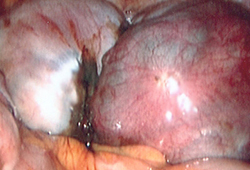
Radical excision of affected areas with restoration of normal anatomy is the preferred method of treating symptomatic women with deep peritoneal disease.[96]Koninckx PR, Meuleman C, Demeyere S, et al. Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil Steril. 1991 Apr;55(4):759-65. http://www.ncbi.nlm.nih.gov/pubmed/2010001?tool=bestpractice.com [97]Chopin N, Vieira M, Borghese B, et al. Operative management of deeply infiltrating endometriosis: results on pelvic pain symptoms according to a surgical classification. J Minim Invasive Gynecol. 2005 Mar-Apr;12(2):106-12. http://www.ncbi.nlm.nih.gov/pubmed/15904612?tool=bestpractice.com
NICE advises that 3 months of pre-operative gonadotrophin-releasing hormone (GnRH) agonist treatment should be considered as an adjunct to surgery for deep endometriosis involving the bowel, bladder or ureter.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Improvement in pain may last up to 5 years after surgery, but the risk of re-intervention approaches 50% in women with moderate to severe disease.[98]Abbott JA, Hawe J, Clayton RD, et al. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2-5 year follow-up. Hum Reprod. 2003 Sep;18(9):1922-7. http://humrep.oxfordjournals.org/cgi/content/full/18/9/1922 http://www.ncbi.nlm.nih.gov/pubmed/12923150?tool=bestpractice.com Less aggressive surgical measures and younger age are predictive of recurrence.[95]Busacca M, Chiaffarino F, Candiani M, et al. Determinants of long-term clinically detected recurrence rates of deep, ovarian, and pelvic endometriosis. Am J Obstet Gynecol. 2006 Aug;195(2):426-32. http://www.ncbi.nlm.nih.gov/pubmed/16890551?tool=bestpractice.com [99]Fedele L, Bianchi S, Zanconato G, et al. Tailoring radicality in demolitive surgery for deeply infiltrating endometriosis. Am J Obstet Gynecol. 2005 Jul;193(1):114-7. http://www.ncbi.nlm.nih.gov/pubmed/16021068?tool=bestpractice.com
For this reason, prolonged hormonal suppression is recommended after surgery for endometriosis.[6]Falcone T, Flyckt R. Clinical management of endometriosis. Obstet Gynecol. 2018 Mar;131(3):557-71. http://www.ncbi.nlm.nih.gov/pubmed/29420391?tool=bestpractice.com
post-surgery hormonal therapy
Additional treatment recommended for SOME patients in selected patient group
If surgery does not result in complete removal of implants, postoperative medical therapy using a gonadotrophin-releasing hormone agonist, progestogen, or androgen may be indicated to increase the duration of pain relief and delay recurrence of symptoms. Some reports indicate a reduction in anatomical relapse, and in the frequency and intensity of dysmenorrhoea recurrence with postoperative use of oral contraceptive pills.[67]Seracchioli R, Mabrouk M, Manuzzi L, et al. Post-operative use of oral contraceptive pills for prevention of anatomical relapse or symptom-recurrence after conservative surgery for endometriosis. Hum Reprod. 2009 Nov;24(11):2729-35. http://humrep.oxfordjournals.org/content/24/11/2729.long http://www.ncbi.nlm.nih.gov/pubmed/19625310?tool=bestpractice.com [68]Seracchioli R, Mabrouk M, Frasca C, et al. Long-term cyclic and continuous oral contraceptive therapy and endometrioma recurrence: a randomized controlled trial. Fertil Steril. 2010 Jan;93(1):52-6. http://www.ncbi.nlm.nih.gov/pubmed/18973896?tool=bestpractice.com [69]Seracchioli R, Mabrouk M, Frasca C, et al. Long-term oral contraceptive pills and postoperative pain management after laparoscopic excision of ovarian endometrioma: a randomized controlled trial. Fertil Steril. 2010 Jul;94(2):464-71. http://www.ncbi.nlm.nih.gov/pubmed/19442968?tool=bestpractice.com There is insufficient evidence to determine whether hormonal suppression, either before or after surgery, is associated with any significant benefit compared with surgery alone.[91]Chen I, Veth VB, Choudhry AJ, et al. Pre- and postsurgical medical therapy for endometriosis surgery Cochrane Database Syst Rev. 2020 Nov 18;11(11):CD003678. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003678.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/33206374?tool=bestpractice.com [92]Wattanayingcharoenchai R, Rattanasiri S, Charakorn C, et al. Postoperative hormonal treatment for prevention of endometrioma recurrence after ovarian cystectomy: a systematic review and network meta-analysis. BJOG. 2021 Jan;128(1):25-35. https://www.doi.org/10.1111/1471-0528.16366 http://www.ncbi.nlm.nih.gov/pubmed/32558987?tool=bestpractice.com [93]Sesti F, Capozzolo T, Pietropolli A, et al. Recurrence rate of endometrioma after laparoscopic cystectomy: a comparative randomized trial between post-operative hormonal suppression treatment or dietary therapy vs. placebo. Eur J Obstet Gynecol Reprod Biol. 2009 Nov;147(1):72-7. http://www.ncbi.nlm.nih.gov/pubmed/19665279?tool=bestpractice.com
immediate fertility desired
controlled ovarian hyper-stimulation
May be achieved with ovulation induction medications including a selective oestrogen receptor modulator (i.e., clomifene), an aromatase inhibitor (e.g., letrozole), highly purified gonadotrophins (also known as menotrophin), or recombinant follicle-stimulating hormone (FSH).
Clomifene (a competitive antagonist of estradiol) disrupts negative feedback and augments gonadotrophin-releasing hormone production.
Letrozole (a competitive reversible inhibitor of testosterone aromatisation) decreases circulating oestrogen, affects the hypothalamic feedback, and induces greater levels of FSH.
A typical starting dose of any gonadotrophin is dependent on the woman's age, diagnosis, and prior stimulation history. The length of the stimulation is dependent on the response to medications.
These medications should only be utilised by experienced infertility practitioners because of the high risk of ovarian hyper-stimulation syndrome and higher-order multiple gestations.
Primary options
clomifene: 50-200 mg orally once daily for 5 days
OR
letrozole: 5 to 7.5mg orally once daily for 5 days, starting on day 3 of cycle
Secondary options
menotrophin: consult product literature for guidance on dose
OR
follitropin alfa: 75-225 international units subcutaneously once daily
analgesia
Additional treatment recommended for SOME patients in selected patient group
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
therapeutic laparoscopy
Additional treatment recommended for SOME patients in selected patient group
The role of surgery is controversial since advanced reproductive technologies successfully treat infertility despite most disease state considerations. However, if symptomatic women without endometrioma or severe deep disease desire fertility, surgery should be offered regardless of age. Women with endometrioma or severe deep disease usually require surgery if pain or large endometrioma (>3 cm) present. Women who fail fertility treatment can be offered surgery, and there is some evidence in support of fertility treatments soon after corrective surgery. One meta-analysis of data from cohort studies found that women who had surgery for deep infiltrating endometriosis before IVF were 2.2 times more likely to have a live birth, compared with unoperated women with deep infiltrating endometriosis who underwent IVF.[109]Casals G, Carrera M, Domínguez JA, et al. Impact of surgery for deep infiltrative endometriosis before in vitro fertilization: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2021 Jul;28(7):1303-12.e5.
https://www.doi.org/10.1016/j.jmig.2021.02.007
http://www.ncbi.nlm.nih.gov/pubmed/33582380?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Laparoscopic image of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].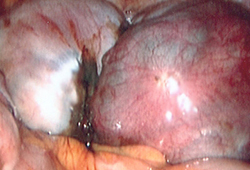 [Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].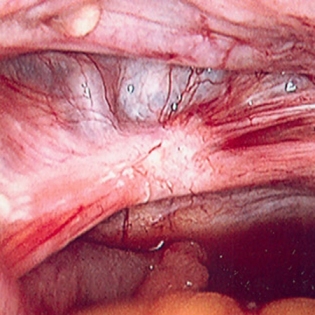
Risk of ovarian failure (reduced number of primordial follicles) after excising endometriomas is approximately 2.4%.[95]Busacca M, Chiaffarino F, Candiani M, et al. Determinants of long-term clinically detected recurrence rates of deep, ovarian, and pelvic endometriosis. Am J Obstet Gynecol. 2006 Aug;195(2):426-32. http://www.ncbi.nlm.nih.gov/pubmed/16890551?tool=bestpractice.com
IVF
Although there is no consensus among experts, there has been a recent shift in the paradigm for those with sub-fertility and endometriosis. Many agree that IVF may be a more viable option for older women and those with multiple contributing factors (such as endometriosis) when compared with surgery. Although IVF is costly it may be the most viable option for women with advanced endometriosis and sub-fertility; however, there are no validating, large randomised trials. Sub-fertility in the setting of advanced endometriosis is controversial, but it remains a viable option for women with advanced disease who are symptomatic or have failed previous IVF cycles.[110]Surrey ES. Endometriosis and assisted reproductive technologies: maximizing outcomes. Semin Reprod Med. 2013 Mar;31(2):154-63. http://www.ncbi.nlm.nih.gov/pubmed/23446863?tool=bestpractice.com
Sub-fertile women with endometrioma may show a diminished response to gonadotrophin stimulation, but the IVF success rates match those who defer surgery.[114]Matalliotakis IM, Cakmak H, Mahutte N, et al. Women with advanced-stage endometriosis and previous surgery respond less well to gonadotropin stimulation, but have similar IVF implantation and delivery rates compared with women with tubal factor infertility. Fertil Steril. 2007 Dec;88(6):1568-72. http://www.ncbi.nlm.nih.gov/pubmed/17349642?tool=bestpractice.com
analgesia
Additional treatment recommended for SOME patients in selected patient group
In clinical trials, non-steroidal anti-inflammatory drug (NSAIDs) effectively treat primary dysmenorrhoea and provide adequate analgesia, but their use remains inconclusive for endometriosis-associated pain.[58]Marjoribanks J, Ayeleke RO, Farquhar C, et al. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015 Jul 30;(7):CD001751. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001751.pub3/full http://www.ncbi.nlm.nih.gov/pubmed/26224322?tool=bestpractice.com [59]Brown J, Crawford TJ, Allen C, et al. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017 Jan 23;(1):CD004753. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD004753.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/28114727?tool=bestpractice.com
There appears to be positive feedback between prostaglandin (PG) synthesis, aromatase activity, and oestrogen production, mediated by abnormally high COX-2 activity in the setting of endometriosis.[57]Bulun SE, Gurates B, Fang Z, et al. Mechanisms of excessive estrogen formation in endometriosis. J Reprod Immunol. 2002 May-Jun;55(1-2):21-33. http://www.ncbi.nlm.nih.gov/pubmed/12062819?tool=bestpractice.com Superficial, often atypical implants (seen more commonly in adolescents) are active PG producers.
Since endometriosis is a chronic inflammatory condition, NSAIDs may improve symptoms of PG-associated inflammation and pain by interrupting receptor-mediated signalling pathways.
Variable responses may be seen with different medicines in each woman.
Ketorolac is only indicated for acute, moderate to severe pain or during the postoperative period; do not use for chronic conditions.
If dysmenorrhoea is the primary complaint, pre-emptively administer oral NSAIDs prior to onset of menses.
In the UK, the National Institute for Health and Care Excellence recommends paracetamol (alone or in combination with an NSAID) as an alternative first-line analgesic for women with endometriosis-related pain.[36]National Institute for Health and Care Excellence (UK). Endometriosis: diagnosis and management. Nov 2024 [internet publication]. https://www.nice.org.uk/guidance/ng73
Primary options
ibuprofen: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
naproxen: 250-500 mg orally twice daily when required, maximum 1250 mg/day
OR
celecoxib: 200 mg orally once or twice daily
OR
paracetamol: 500-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
Secondary options
ketorolac: consult specialist for guidance on dose
therapeutic laparoscopy
Additional treatment recommended for SOME patients in selected patient group
The role of surgery is controversial since advanced reproductive technologies successfully treat infertility despite most disease state considerations. However, if symptomatic women without endometrioma or severe deep disease desire fertility, surgery should be offered regardless of age. Women with endometrioma or severe deep disease usually require surgery if pain or large endometrioma (>3 cm) present. Women who fail fertility treatment can be offered surgery, and there is some evidence in support of fertility treatments soon after corrective surgery. One meta-analysis of data from cohort studies found that women who had surgery for deep infiltrating endometriosis before IVF were 2.2 times more likely to have a live birth, compared with unoperated women with deep infiltrating endometriosis who underwent IVF.[109]Casals G, Carrera M, Domínguez JA, et al. Impact of surgery for deep infiltrative endometriosis before in vitro fertilization: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2021 Jul;28(7):1303-12.e5.
https://www.doi.org/10.1016/j.jmig.2021.02.007
http://www.ncbi.nlm.nih.gov/pubmed/33582380?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Laparoscopic image of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].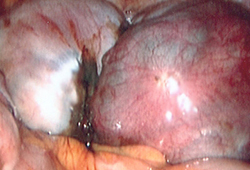 [Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].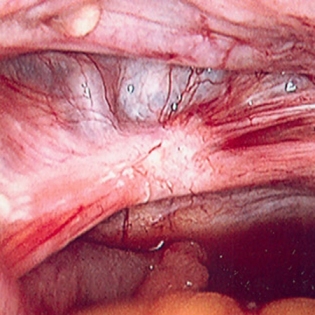
Risk of ovarian failure (reduced number of primordial follicles) after excising endometriomas is approximately 2.4%.[95]Busacca M, Chiaffarino F, Candiani M, et al. Determinants of long-term clinically detected recurrence rates of deep, ovarian, and pelvic endometriosis. Am J Obstet Gynecol. 2006 Aug;195(2):426-32. http://www.ncbi.nlm.nih.gov/pubmed/16890551?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer