Diagnosis and severity are established by symptoms and quantitative findings on echocardiography.[10]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-227.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
http://www.ncbi.nlm.nih.gov/pubmed/33332150?tool=bestpractice.com
[11]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.
https://academic.oup.com/eurheartj/article/43/7/561/6358470
http://www.ncbi.nlm.nih.gov/pubmed/34453165?tool=bestpractice.com
[12]Robinson S, Ring L, Augustine DX, et al. The assessment of mitral valve disease: a guideline from the British Society of Echocardiography. Echo Res Pract. 2021 Sep 27;8(1):G87-136.
https://echo.biomedcentral.com/articles/10.1530/ERP-20-0034
http://www.ncbi.nlm.nih.gov/pubmed/34061768?tool=bestpractice.com
Presentation
There are no pathognomonic features to diagnose MR by history; however, dyspnoea on exertion, orthopnoea, paroxysmal nocturnal dyspnoea, lower extremity oedema, palpitations, fatigue, and diaphoresis are common presenting symptoms.
Patients with acute MR may present with a sudden and marked increase in symptoms of congestive heart failure, with weakness, fatigue, dyspnoea, and sometimes respiratory failure and shock.
Physical examination
MR usually presents as a holosystolic, blowing murmur at the apex that radiates to the axilla. Chronic MR is also associated with laterally displaced apical impulse (with left ventricular dilation) and diminished S1.
Transthoracic echocardiogram
This is the definitive test for determining the presence, severity, and mechanism of flail, as well as evaluating left ventricular size and function, left atrial size, other valvular abnormalities, and right ventricular systolic pressure.[10]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-227.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
http://www.ncbi.nlm.nih.gov/pubmed/33332150?tool=bestpractice.com
[11]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.
https://academic.oup.com/eurheartj/article/43/7/561/6358470
http://www.ncbi.nlm.nih.gov/pubmed/34453165?tool=bestpractice.com
[13]Lancellotti P, Moura L, Pierard LA, et al; European Association of Echocardiography. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010 May;11(4):307-32.
http://www.ncbi.nlm.nih.gov/pubmed/20435783?tool=bestpractice.com
It is also useful for assessing serial changes in left ventricular size and function, and evaluating the patient after a change in symptoms. Measurement of left ventricular global longitudinal strain may provide earlier detection of systolic dysfunction than ejection fraction and evidence shows that it may have incremental prognostic value in patients with primary MR treated with surgical repair.[10]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-227.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
http://www.ncbi.nlm.nih.gov/pubmed/33332150?tool=bestpractice.com
[11]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.
https://academic.oup.com/eurheartj/article/43/7/561/6358470
http://www.ncbi.nlm.nih.gov/pubmed/34453165?tool=bestpractice.com
[14]Hiemstra YL, Tomsic A, van Wijngaarden SE, et al. Prognostic value of global longitudinal strain and etiology after surgery for primary mitral regurgitation. JACC Cardiovasc Imaging. 2020 Feb;13(2 pt 2):577-85.
https://www.sciencedirect.com/science/article/pii/S1936878X19304267
http://www.ncbi.nlm.nih.gov/pubmed/31202761?tool=bestpractice.com
[15]Kim HM, Cho GY, Hwang IC, et al. Myocardial strain in prediction of outcomes after surgery for severe mitral regurgitation. JACC Cardiovasc Imaging. 2018 Sep;11(9):1235-44.
https://www.doi.org/10.1016/j.jcmg.2018.03.016
http://www.ncbi.nlm.nih.gov/pubmed/29778855?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Apical 3-chamber view of hypertrophic cardiomyopathy with systolic anterior motionFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends]. [Figure caption and citation for the preceding image starts]: Apical 4-chamber view of flail posterior mitral leafletFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber view of flail posterior mitral leafletFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].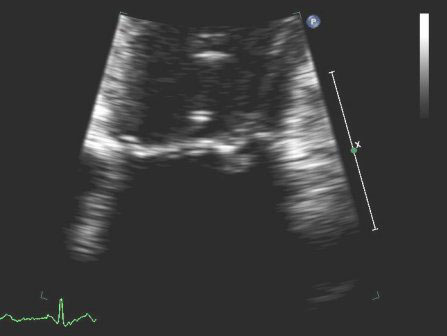 [Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing posterior mitral leaflet prolapseFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing posterior mitral leaflet prolapseFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends]. [Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 2D viewFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 2D viewFrom the collection of Prakash P. Punjabi [Citation ends].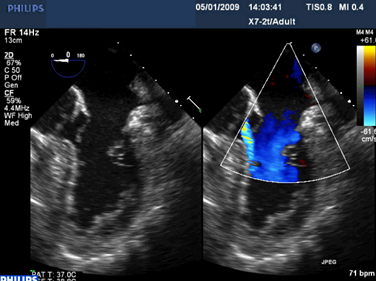 [Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends]. [Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends]. [Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends].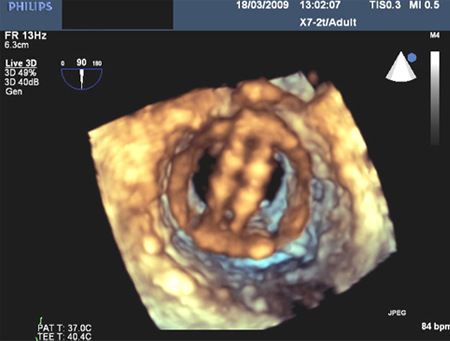
Measures of flow
Spatial mapping, flow convergence, pulmonary vein velocity patterns, vena contracta width, continuous-wave Doppler density and shape, and quantification of antegrade valvular flow volumes can be used to further assess severity. A weighted average of multiple methods is often used.
Flow convergence method, also called the proximal isovelocity surface area method, involves looking at the colour images on the left ventricular side of the mitral regurgitant images.[16]Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med. 2005 Mar 3;352(9):875-83.
https://www.nejm.org/doi/10.1056/NEJMoa041451
http://www.ncbi.nlm.nih.gov/pubmed/15745978?tool=bestpractice.com
[17]Cosgrove DM, Stewart WJ. Mitral valvuloplasty. Curr Probl Cardiol. 1989 Jul;14(7):359-415.
http://www.ncbi.nlm.nih.gov/pubmed/2667897?tool=bestpractice.com
[18]Stewart WJ, Currie PJ, Salcedo EE, et al. Evaluation of mitral leaflet motion by echocardiography and jet direction by Doppler color flow mapping to determine the mechanisms of mitral regurgitation. J Am Coll Cardiol. 1992 Nov 15;20(6):1353-61.
https://www.sciencedirect.com/science/article/pii/073510979290248L
http://www.ncbi.nlm.nih.gov/pubmed/1430686?tool=bestpractice.com
[19]Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003 Jul;16(7):777-802.
http://www.ncbi.nlm.nih.gov/pubmed/12835667?tool=bestpractice.com
This flow convergence zone is the location where the blood is accelerating to go across the regurgitant orifice, as it undergoes a pressure drop from left ventricular pressure to left atrial pressure. Analysis of this convergence zone when its shape is hemispheric allows estimation of the surface area of the hemisphere; it calculates the actual size of the regurgitant lesion, a fundamental parameter of valve integrity, which may be less load-dependent than other methods. A regurgitant orifice area over 0.4 cm² is indicative of severe regurgitation, whereas <0.2 cm² is considered mild.
Pulmonary vein flow profiles are also useful for determining severity.[20]Pu M, Griffin BP, Vandervoort PM, et al. The value of assessing pulmonary venous flow velocity for predicting severity of mitral regurgitation: a quantitative assessment integrating left ventricular function. J Am Soc Echocardiogr. 1999 Sep;12(9):736-43.
http://www.ncbi.nlm.nih.gov/pubmed/10477418?tool=bestpractice.com
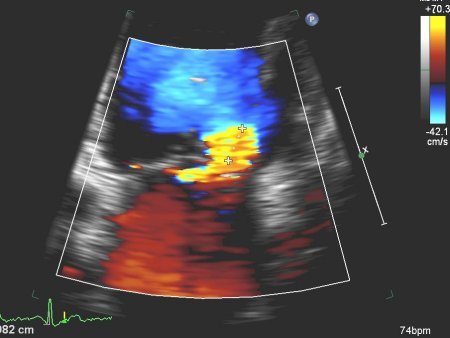
The normal pulmonary vein pattern is to have flow velocity during ventricular systole higher than antegrade flow velocity during diastole, a pattern that persists in mild and sometimes moderate MR. As the regurgitation progresses, pulmonary vein systolic velocity becomes blunted, with systolic velocity less than diastolic velocity, and sometimes with cessation of systolic flow. In patients with severe MR, systolic flow is often reversed, with flow away from the left atrium during ventricular systole. This occurs due to the large V wave on left atrial pressure and a transient reversal of flow back into the pulmonary parenchyma during ventricular systole.[Figure caption and citation for the preceding image starts]: Apical 4-chamber view of 1-2+ posteriorly directed mitral regurgitationFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends]. [Figure caption and citation for the preceding image starts]: Apical 4-chamber view of 4+ (severe) mitral regurgitation and a large proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber view of 4+ (severe) mitral regurgitation and a large proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].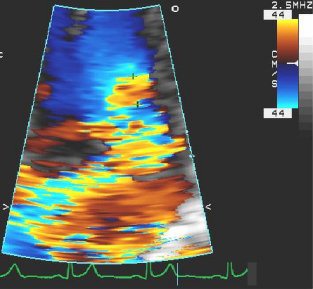 [Figure caption and citation for the preceding image starts]: Apical 4-chamber view of severe MR with proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber view of severe MR with proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].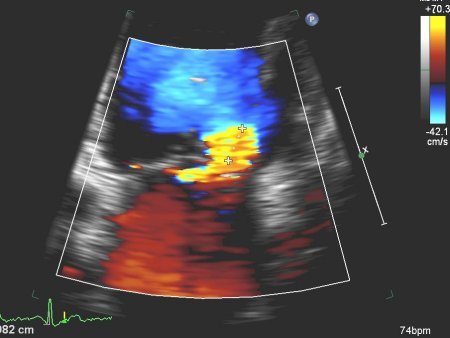
Transoesophageal echocardiogram
May be needed to better assess the severity and aetiology in rare occasions where the degree of symptoms does not match transthoracic echocardiogram findings.[10]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-227.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
http://www.ncbi.nlm.nih.gov/pubmed/33332150?tool=bestpractice.com
[11]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.
https://academic.oup.com/eurheartj/article/43/7/561/6358470
http://www.ncbi.nlm.nih.gov/pubmed/34453165?tool=bestpractice.com
[21]Pu M, Vandervoort PM, Griffin BP, et al. Quantification of mitral regurgitation by the proximal convergence method using transesophageal echocardiography: clinical validation of a geometric correction for proximal flow constraint. Circulation. 1995 Oct 15;92(8):2169-77.
https://www.ahajournals.org/doi/10.1161/01.cir.92.8.2169
http://www.ncbi.nlm.nih.gov/pubmed/7554198?tool=bestpractice.com
Additionally, three-dimensional transoesophageal echocardiogram provides a surgical view of the mitral valve, which can help the heart team discussion on intervention strategy.[10]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-227.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
http://www.ncbi.nlm.nih.gov/pubmed/33332150?tool=bestpractice.com
[11]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.
https://academic.oup.com/eurheartj/article/43/7/561/6358470
http://www.ncbi.nlm.nih.gov/pubmed/34453165?tool=bestpractice.com
A stress echocardiogram is often useful for determining the severity and impact of the disease on the patient's exercise haemodynamics.
ECG
All patients must undergo ECG examination as a routine screening as well as for any rhythm disturbance (e.g., atrial fibrillation).[13]Lancellotti P, Moura L, Pierard LA, et al; European Association of Echocardiography. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010 May;11(4):307-32.
http://www.ncbi.nlm.nih.gov/pubmed/20435783?tool=bestpractice.com
Cardiac catheterisation and cardiac magnetic resonance imaging (CMR)
Cardiac catheterisation is used when non-invasive evaluation is inconclusive or discordant with clinical findings.[10]Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-227.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000923
http://www.ncbi.nlm.nih.gov/pubmed/33332150?tool=bestpractice.com
[11]Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.
https://academic.oup.com/eurheartj/article/43/7/561/6358470
http://www.ncbi.nlm.nih.gov/pubmed/34453165?tool=bestpractice.com
It is also used to check for disease in coronary arteries. Patients suspected of having pulmonary hypertension and/or poor left or right ventricular function should have cardiac catheterisation to calculate pulmonary artery pressures and determine level of pulmonary hypertension.
Patients with poor left or right ventricular function and/or mitral annular/leaflet calcification may undergo cardiac CMR. Early data using CMR have shown that myocardial fibrosis has been associated with sudden cardiac death and ventricular arrhythmias in primary MR.[22]Kitkungvan D, Nabi F, Kim RJ, et al. Myocardial fibrosis in patients with primary mitral regurgitation with and without prolapse. J Am Coll Cardiol. 2018 Aug 21;72(8):823-34.
https://www.sciencedirect.com/science/article/pii/S0735109718354019
http://www.ncbi.nlm.nih.gov/pubmed/30115220?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Apical 4-chamber view of flail posterior mitral leafletFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber view of flail posterior mitral leafletFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].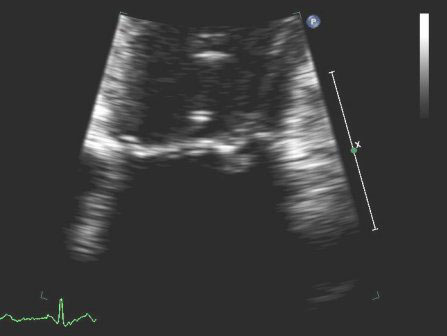 [Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing posterior mitral leaflet prolapseFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing posterior mitral leaflet prolapseFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends]. [Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 2D viewFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 2D viewFrom the collection of Prakash P. Punjabi [Citation ends].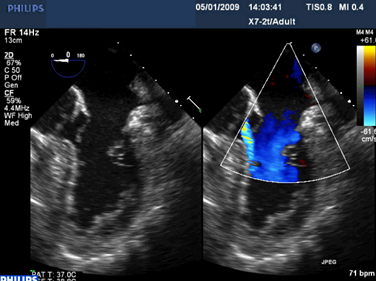 [Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends]. [Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends]. [Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Prosthetic mitral valve with intermittent mitral regurgitationFrom the collection of Prakash P. Punjabi [Citation ends].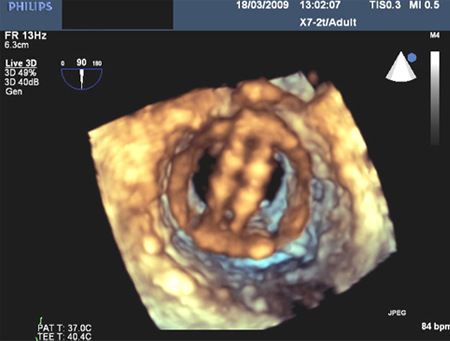
 [Figure caption and citation for the preceding image starts]: Apical 4-chamber view of 4+ (severe) mitral regurgitation and a large proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber view of 4+ (severe) mitral regurgitation and a large proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].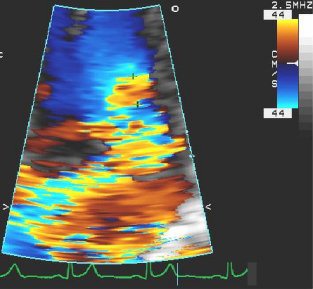 [Figure caption and citation for the preceding image starts]: Apical 4-chamber view of severe MR with proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber view of severe MR with proximal isovelocity surface areaFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].