Aetiology
The mitral valve apparatus consists of anterior and posterior leaflets, chordae tendineae, anterolateral, and posteromedial papillary muscles, and mitral annulus. To be inclusive, it also includes the atrial and ventricular myocardium. Mitral valve dysfunction may result from aberrations of any portion of the mitral valve apparatus, due to mechanical, traumatic, infectious, degenerative, congenital, or metabolic causes.
MR can be primary or secondary and either acute or chronic. Primary MR is a consequence of degenerative disease of one or more components of the mitral valve; secondary MR is a consequence of annular dilatation and distortion of the subvalvular apparatus secondary to left ventricular remodelling and dysfunction, usually associated with cardiomyopathy or coronary artery disease.[1]
Typical causes of acute MR include infective endocarditis, ischaemic papillary muscle dysfunction or rupture, acute rheumatic fever, and acute dilation of the left ventricle due to myocarditis or ischaemia.[4]
Common causes of chronic MR include those already listed as well as myxomatous degeneration of the mitral leaflets or chordae tendineae, mitral valve prolapse, and mitral annular enlargement.[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 2D viewFrom the collection of Prakash P. Punjabi [Citation ends].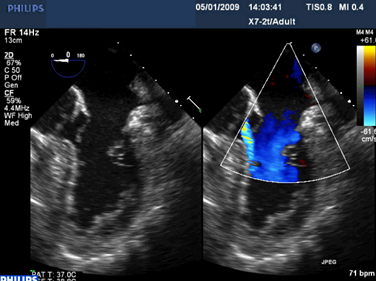 [Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends].
Pathophysiology
Chronic MR can be mild or moderate and can be asymptomatic for many years; however, with progression of the disease to severe, eccentric cardiac hypertrophy occurs, which leads to elongation of the myocardial fibres and increased left ventricular end-diastolic volume. This is a compensatory mechanism that allows an increase in total stroke volume to maintain adequate cardiac output. Additionally, both left ventricular and left atrial enlargement will accommodate the regurgitant volume at a lower filling pressure, which prevents pulmonary congestion. In this stage of the disease, which may last for 7 to 10 years, patients are typically asymptomatic. Eventually, prolonged volume overload leads to left ventricular dysfunction and increased left ventricular end-systolic diameter. However, even in this phase of the disease, left ventricular ejection fraction usually remains above 50% to 60%.[5]
Classification
Primary MR
A consequence of degenerative disease of one or more components of the mitral valve.[1]
Secondary MR
A consequence of annular dilatation and distortion of the subvalvular apparatus secondary to left ventricular remodelling and dysfunction, usually associated with cardiomyopathy or coronary artery disease.[1]
Acute MR
Results from acute disruption of mitral valve leaflets, chordae tendineae, or papillary muscles following myocardial infarction, trauma, infective endocarditis, rheumatic fever, or other causes that suddenly disrupt the mitral valve apparatus causing sudden changes in haemodynamics and symptoms.
There is no actual classification cut-off point between acute and chronic, because acute MR occurs suddenly within seconds after chordal or papillary muscle rupture and results in immediate symptoms.
Chronic MR
Occurs over many years and results in volume overload and left ventricular dysfunction.
Use of this content is subject to our disclaimer