Investigations
1st investigations to order
FBC
Test
Order in all patients with suspected microscopic colitis. Some patients present with mild anaemia.
A non-sensitive and non-specific test. Does not exclude diagnosis if normal.
Result
may be normal; may show decreased haemoglobin
basic metabolic panel
Test
Order if patient has evidence of severe presentation including stool output of 15 or more bowel movements per day and signs of dehydration.[12]
Result
raised creatinine, hypokalaemia
CRP
Test
Order in all patients to exclude inflammatory bowel disease.
Result
normal
erythrocyte sedimentation rate
Test
Order in all patients (if part of the protocol in your centre) to exclude inflammatory bowel disease.
Result
normal
immunoglobulin A-tissue transglutaminase
stool studies for infective pathogens
Test
Order to exclude gastrointestinal infections, particularly in those who have recently travelled to an endemic area. Although infective pathogens typically cause acute or subacute diarrhoea, some patients may present with chronic diarrhoea.
Stool studies should include comprehensive culture of Salmonella, Shigella, Campylobacter, Yersinia, and also Clostridium difficile toxin A and B immunoassay. Faecal leukocytes may be present but they are neither sensitive nor specific.[7][52]
Result
negative culture and negative Clostridium difficile toxins A and B
stool O+P
Test
Order a stool microscopy for ova and parasites to rule out parasitic infections, particularly if the patient has recently traveled to an endemic area.[7]
Result
absence of specific ova and/or parasite
lateral flow immunoassay (Giardia)
Test
Order a Giardia antigen test to rule out giardiasis, particularly if the patient has recently travelled to an endemic area.[7]
Result
negative
ileocolonoscopy
Test
European guidelines recommend an ileocolonoscopy with biopsies from at least the right and left colon.[6]
Result
colonic mucosa usually normal or near-normal gross appearance; erythema or oedema may be seen
colonic biopsies
Test
If initial laboratory investigations are negative, obtain biopsies from at least the right and left colon at time of ileocolonoscopy.[6] Diagnosis of microscopic colitis is confirmed by the presence of characteristic histological findings, which identify two major subtypes of microscopic colitis.[6]
[Figure caption and citation for the preceding image starts]: Biopsy demonstrating collagenous colitis with a thickened subepithelial collagen bandTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].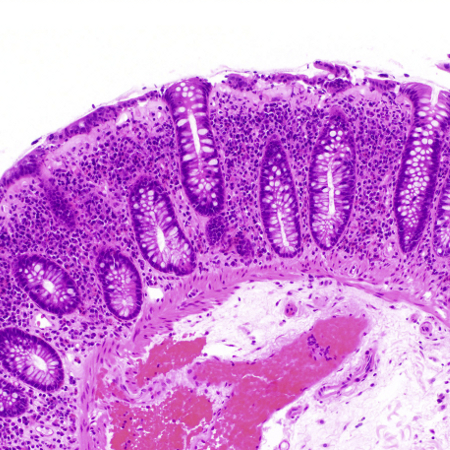 [Figure caption and citation for the preceding image starts]: Biopsy demonstrating lymphocytic colitis with intraepithelial lymphocytosisTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy demonstrating lymphocytic colitis with intraepithelial lymphocytosisTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].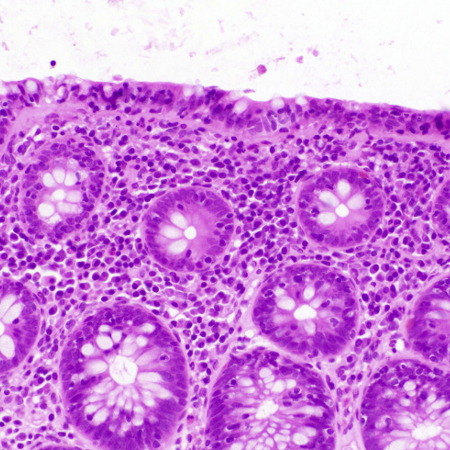
There is a subset of patients who do not meet the above histological criteria. These patients may be diagnosed as microscopic colitis incomplete or microscopic colitis not otherwise specified. Microscopic colitis incomplete comprises incomplete collagenous colitis (defined by a thickened subepithelial collagenous band >5 micrometres but <10 micrometres) and incomplete lymphocytic colitis (defined by >10 but <20 intraepithelial lymphocytes and a normal collagenous band). Both types show a mild inflammatory infiltrate in the lamina propria.
Result
collagenous colitis: thickened subepithelial collagen band ≥10 micrometres (normal <5 micrometres) combined with an increased inflammatory infiltrate in lamina propria; lymphocytic colitis: increased number of intraepithelial lymphocytes ≥20 per 100 surface epithelial cells (normal <5 micrometres) combined with an increased inflammatory infiltrate in lamina propria and a not significantly thickened collagenous band (<10 micrometres)
Investigations to consider
flexible sigmoidoscopy with biopsies
Test
In patients who have recently undergone a colonoscopy for cancer screening, order a flexible sigmoidoscopy for evaluation of microscopic colitis. This is a reasonable next test to evaluate for microscopic colitis provided biopsies are obtained above the rectosigmoid colon.[1]
Diagnosis of microscopic colitis is confirmed by the presence of characteristic histological findings, which identify two major subtypes of microscopic colitis.[6]
[Figure caption and citation for the preceding image starts]: Biopsy demonstrating collagenous colitis with a thickened subepithelial collagen bandTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].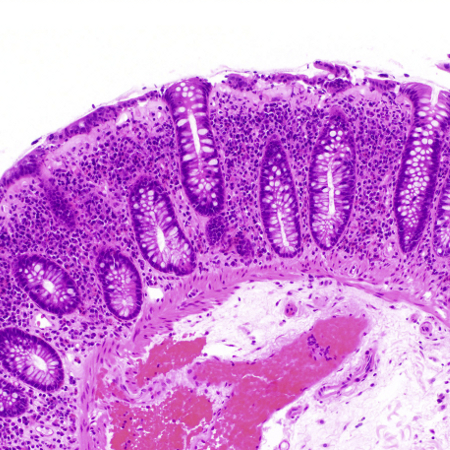 [Figure caption and citation for the preceding image starts]: Biopsy demonstrating lymphocytic colitis with intraepithelial lymphocytosisTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy demonstrating lymphocytic colitis with intraepithelial lymphocytosisTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].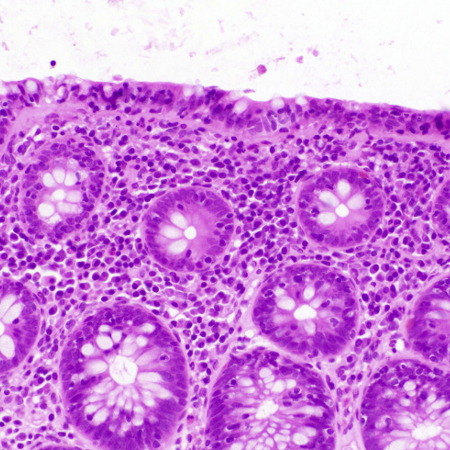
There is a subset of patients who do not meet the above histological criteria. These patients may be diagnosed as microscopic colitis incomplete or microscopic colitis not otherwise specified. Microscopic colitis incomplete comprises incomplete collagenous colitis (defined by a thickened subepithelial collagenous band >5 micrometres but <10 micrometres) and incomplete lymphocytic colitis (defined by >10 but <20 intraepithelial lymphocytes and a normal collagenous band). Both types show a mild inflammatory infiltrate in the lamina propria.
Result
usually normal gross appearance although erythema or oedema may be seen; biopsy specimens show either (a) collagenous colitis: thickened subepithelial collagen band ≥10 micrometres (normal <5 micrometres) combined with an increased inflammatory infiltrate in lamina propria, or (b) lymphocytic colitis: increased number of intraepithelial lymphocytes ≥20 per 100 surface epithelial cells (normal <5 micrometres) combined with an increased inflammatory infiltrate in lamina propria and a not significantly thickened collagenous band (<10 micrometres)
Use of this content is subject to our disclaimer