Although microscopic colitis is not associated with increased mortality, symptoms can lead to a significantly impaired quality of life.[2]Münch A, Sanders DS, Molloy-Bland M, et al. Undiagnosed microscopic colitis: a hidden cause of chronic diarrhoea and a frequently missed treatment opportunity. Frontline Gastroenterol. 2019 Jul 5;11(3):228-34.
https://fg.bmj.com/content/11/3/228
http://www.ncbi.nlm.nih.gov/pubmed/32419914?tool=bestpractice.com
[3]Nguyen GC, Smalley WE, Vege SS, et al. American Gastroenterological Association Institute guideline on the medical management of microscopic colitis. Gastroenterology. 2016 Jan;150(1):242-6.
https://www.gastrojournal.org/article/S0016-5085(15)01625-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/26584605?tool=bestpractice.com
Most investigations are done to first rule out other causes of chronic diarrhoea such as inflammatory bowel disease, coeliac disease, or irritable bowel syndrome. See Differentials. Unlike Crohn's disease and ulcerative colitis, the colonic mucosa in patients with microscopic colitis has a normal or near-normal appearance on colonoscopy.[9]Burke KE, D'Amato M, Ng SC, et al. Microscopic colitis. Nat Rev Dis Primers. 2021 Jun 10;7(1):39.
http://www.ncbi.nlm.nih.gov/pubmed/34112810?tool=bestpractice.com
However, biopsy of colonic mucosa demonstrates characteristic histopathological features of collagenous colitis or lymphocytic colitis, which confirms the diagnosis.[8]Münch A, Aust D, Bohr J, et al. Microscopic colitis: current status, present and future challenges: statements of the European Microscopic Colitis Group. J Crohns Colitis. 2012 Oct;6(9):932-45.
https://academic.oup.com/ecco-jcc/article/6/9/932/2392159
http://www.ncbi.nlm.nih.gov/pubmed/22704658?tool=bestpractice.com
Clinical presentation
Suspect microscopic colitis in a patient presenting with chronic, non-bloody, watery diarrhoea, particularly if they are aged >50 years and female.[2]Münch A, Sanders DS, Molloy-Bland M, et al. Undiagnosed microscopic colitis: a hidden cause of chronic diarrhoea and a frequently missed treatment opportunity. Frontline Gastroenterol. 2019 Jul 5;11(3):228-34.
https://fg.bmj.com/content/11/3/228
http://www.ncbi.nlm.nih.gov/pubmed/32419914?tool=bestpractice.com
[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
These symptoms were reported by 85% to 100% of patients with microscopic colitis in 22 studies.[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
Patients usually report between 5 and 10 watery stools per day, but some may have 15 or more bowel movements per day.[12]Münch A, Langner C. Microscopic colitis: clinical and pathologic perspectives. Clin Gastroenterol Hepatol. 2015 Feb;13(2):228-36.
https://www.cghjournal.org/article/S1542-3565(14)00002-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/24407107?tool=bestpractice.com
Other symptoms may include any of faecal urgency, faecal incontinence, nocturnal stools, abdominal pain, weight loss, bloating, and fatigue.[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
The clinical course is variable, with chronic or recurrent mild to severe symptoms persisting for months to years.[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
History
Take a thorough history. Ask about:
Number of stools per day and whether the patient is experiencing night episodes.
Duration of symptoms.
Recent travel to endemic areas, to exclude gastrointestinal infection. Although infective pathogens typically cause acute or subacute diarrhoea, some patients may present with chronic diarrhoea.
Recent antibiotic exposure, as diarrhoea can be an adverse effect of antibiotics.
Family history of autoimmune diseases, such as coeliac disease, hypothyroidism, rheumatoid arthritis, hyperthyroidism, or Crohn's disease. People with these disorders are at higher risk of developing microscopic colitis.[9]Burke KE, D'Amato M, Ng SC, et al. Microscopic colitis. Nat Rev Dis Primers. 2021 Jun 10;7(1):39.
http://www.ncbi.nlm.nih.gov/pubmed/34112810?tool=bestpractice.com
[21]Park T, Cave D, Marshall C. Microscopic colitis: a review of etiology, treatment and refractory disease. World J Gastroenterol. 2015 Aug 7;21(29):8804-10.
https://www.wjgnet.com/1007-9327/full/v21/i29/8804.htm
http://www.ncbi.nlm.nih.gov/pubmed/26269669?tool=bestpractice.com
Presence of bloody diarrhoea, which may indicate a differential diagnosis such as food poisoning.
Relationship of abdominal pain and bowel movements. Some patients with microscopic colitis present with mild pain that is relieved after a bowel movement.
Ask about risk factors for microscopic colitis including cigarette smoking, presence of concomitant autoimmune diseases such as coeliac disease, rheumatoid arthritis, and thyroid disorders, and use of certain medications (i.e., non-steroidal anti-inflammatory drugs [NSAIDs], proton-pump inhibitors [PPIs], selective serotonin-reuptake inhibitors [SSRIs], statins, and H2 antagonists).[9]Burke KE, D'Amato M, Ng SC, et al. Microscopic colitis. Nat Rev Dis Primers. 2021 Jun 10;7(1):39.
http://www.ncbi.nlm.nih.gov/pubmed/34112810?tool=bestpractice.com
[21]Park T, Cave D, Marshall C. Microscopic colitis: a review of etiology, treatment and refractory disease. World J Gastroenterol. 2015 Aug 7;21(29):8804-10.
https://www.wjgnet.com/1007-9327/full/v21/i29/8804.htm
http://www.ncbi.nlm.nih.gov/pubmed/26269669?tool=bestpractice.com
[24]Masclee GM, Coloma PM, Kuipers EJ, et al. Increased risk of microscopic colitis with use of proton pump inhibitors and non-steroidal anti-inflammatory drugs. Am J Gastroenterol. 2015 May;110(5):749-59.
http://www.ncbi.nlm.nih.gov/pubmed/25916221?tool=bestpractice.com
[25]Bonderup OK, Nielsen GL, Dall M, et al. Significant association between the use of different proton pump inhibitors and microscopic colitis: a nationwide Danish case-control study. Aliment Pharmacol Ther. 2018 Sep;48(6):618-25.
http://www.ncbi.nlm.nih.gov/pubmed/30039564?tool=bestpractice.com
[26]Mori S, Kadochi Y, Luo Y, et al. Proton pump inhibitor induced collagen expression in colonocytes is associated with collagenous colitis. World J Gastroenterol. 2017 Mar 7;23(9):1586-93.
https://www.wjgnet.com/1007-9327/full/v23/i9/1586.htm
http://www.ncbi.nlm.nih.gov/pubmed/28321159?tool=bestpractice.com
[27]Verhaegh BP, de Vries F, Masclee AA, et al. High risk of drug-induced microscopic colitis with concomitant use of NSAIDs and proton pump inhibitors. Aliment Pharmacol Ther. 2016 May;43(9):1004-13.
https://onlinelibrary.wiley.com/doi/10.1111/apt.13583
http://www.ncbi.nlm.nih.gov/pubmed/26956016?tool=bestpractice.com
[44]Yen EF, Pokhrel B, Du H, et al. Current and past cigarette smoking significantly increase risk for microscopic colitis. Inflamm Bowel Dis. 2012 Oct;18(10):1835-41.
http://www.ncbi.nlm.nih.gov/pubmed/22147506?tool=bestpractice.com
[45]Vigren L, Sjöberg K, Benoni C, et al. Is smoking a risk factor for collagenous colitis?. Scand J Gastroenterol. 2011 Nov;46(11):1334-9.
http://www.ncbi.nlm.nih.gov/pubmed/21854096?tool=bestpractice.com
Note that the risk of developing microscopic colitis is higher in women than men.[10]Tong J, Zheng Q, Zhang C, et al. Incidence, prevalence, and temporal trends of microscopic colitis: a systematic review and meta-analysis. Am J Gastroenterol. 2015 Feb;110(2):265-76.
http://www.ncbi.nlm.nih.gov/pubmed/25623658?tool=bestpractice.com
Physical examination
Physical examination is usually non-specific and unlikely to further aid in refining the differential diagnosis in most patients.
Initial investigations
Order the following investigations in all patients to rule out other causes of chronic diarrhoea:[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
[7]Tome J, Kamboj AK, Pardi DS. Microscopic colitis: a concise review for clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8.
https://www.mayoclinicproceedings.org/article/S0025-6196(21)00246-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33958059?tool=bestpractice.com
Serological tests for coeliac disease (i.e., immunoglobulin A-tissue transglutaminase [IgA-tTG] titre), a basic metabolic panel to assess dehydration in patients with severe disease, and full blood count with inflammatory markers (erythrocyte sedimentation rate, C-reactive protein) to rule out coeliac disease and inflammatory bowel disease, respectively. Some patients with microscopic colitis may present with mild anaemia.
Stool studies for Clostridium difficile toxin, routine stool cultures for Salmonella, Shigella, Campylobacter, and Yersinia; and specific testing for Escherichia coli O157:H7 to rule out gastrointestinal infection.
Stool microscopy for ova and parasites, and giardia stool antigen to rule out parasitic infections, particularly if the patient has recently travelled to an endemic area.
Ileocolonoscopy
Order an ileocolonoscopy with biopsies from at least the right and left colon if the initial investigations are negative.[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
[48]Bohr J, Wickbom A, Hegedus A, et al. Diagnosis and management of microscopic colitis: current perspectives. Clin Exp Gastroenterol. 2014 Aug 21;7:273-84.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4144984
http://www.ncbi.nlm.nih.gov/pubmed/25170275?tool=bestpractice.com
Diagnosis is confirmed by the presence of characteristic pathohistological findings.[5]Arasaradnam RP, Brown S, Forbes A, et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, 3rd edition. Gut. 2018 Aug;67(8):1380-99.
https://gut.bmj.com/content/67/8/1380.long
http://www.ncbi.nlm.nih.gov/pubmed/29653941?tool=bestpractice.com
[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
On endoscopic examination, findings are non-specific. The colon typically appears completely normal, although mild erythema and oedema may be seen.[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
On histological examination, distinct abnormalities are found that identify two major histological subtypes:[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
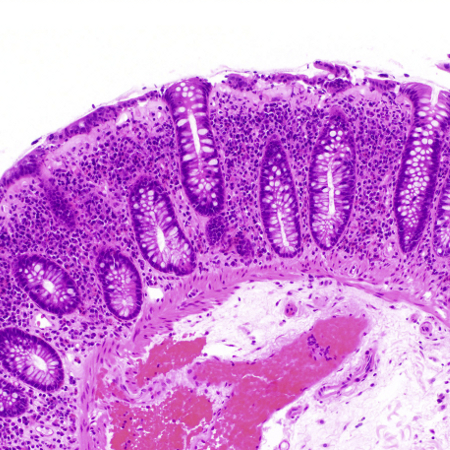
Collagenous colitis: characterised by a thickened subepithelial collagenous band ≥10 micrometres (normal <5 micrometres) combined with an increased inflammatory infiltrate in the lamina propria.
[Figure caption and citation for the preceding image starts]: Biopsy demonstrating collagenous colitis with a thickened subepithelial collagen bandTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].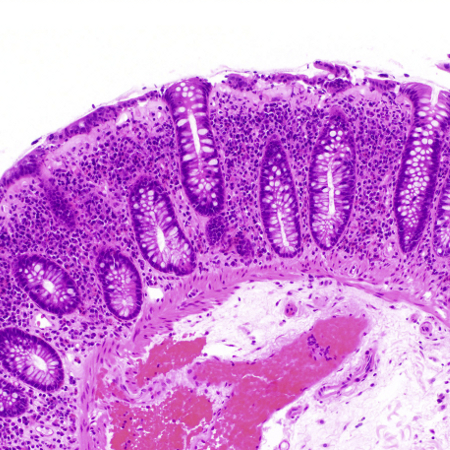
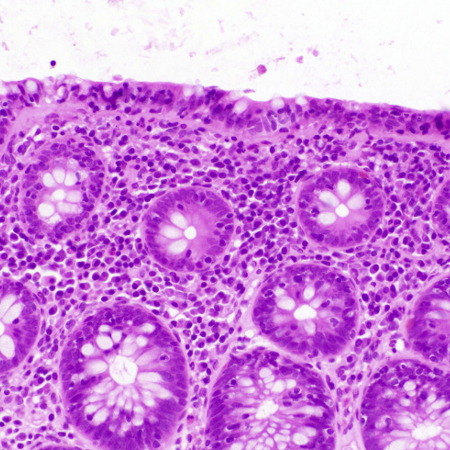
Lymphocytic colitis: characterised by an increased number of intraepithelial lymphocytes ≥20 per 100 surface epithelial cells (normal <5 micrometres) combined with an increased inflammatory infiltrate in the lamina propria and a not significantly thickened collagenous band (<10 micrometres).
[Figure caption and citation for the preceding image starts]: Biopsy demonstrating lymphocytic colitis with intraepithelial lymphocytosisTome J et al. Microscopic Colitis: A Concise Review for Clinicians. Mayo Clin Proc. 2021 May;96(5):1302-8; used with permission [Citation ends].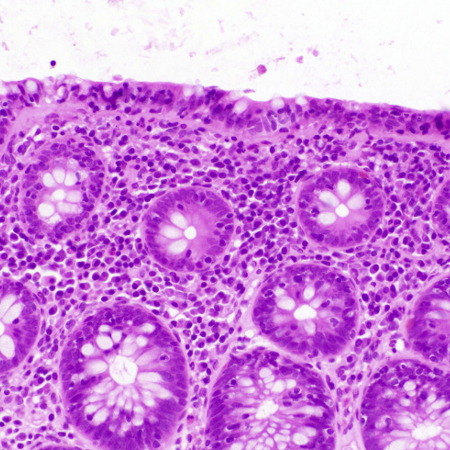
There is a further subset of patients who do not meet the above histological criteria. These patients may be diagnosed as microscopic colitis incomplete or microscopic colitis not otherwise specified. Microscopic colitis incomplete comprises incomplete collagenous colitis (defined by a thickened subepithelial collagenous band >5 micrometres but <10 micrometres) and incomplete lymphocytic colitis (defined by >10 but <20 intraepithelial lymphocytes per 100 epithelial cells and a normal collagenous band). Both types show a mild inflammatory infiltrate in the lamina propria.[6]Miehlke S, Guagnozzi D, Zabana Y, et al. European guidelines on microscopic colitis: United European Gastroenterology and European Microscopic Colitis Group statements and recommendations. United European Gastroenterol J. 2021 Feb 22;9(1):13-37.
https://onlinelibrary.wiley.com/doi/10.1177/2050640620951905
http://www.ncbi.nlm.nih.gov/pubmed/33619914?tool=bestpractice.com
Other investigations
Flexible sigmoidoscopy
In patients who have recently undergone a colonoscopy for cancer screening, order flexible sigmoidoscopy for evaluation of microscopic colitis. This is a reasonable next test provided biopsies are obtained above the rectosigmoid colon.[1]Miehlke S, Verhaegh B, Tontini GE, et al. Microscopic colitis: pathophysiology and clinical management. Lancet Gastroenterol Hepatol. 2019 Apr;4(4):305-14.
http://www.ncbi.nlm.nih.gov/pubmed/30860066?tool=bestpractice.com
Since most patients will have changes detectable in the distal colon, the diagnosis can be made from biopsies taken at flexible sigmoidoscopy.[5]Arasaradnam RP, Brown S, Forbes A, et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, 3rd edition. Gut. 2018 Aug;67(8):1380-99.
https://gut.bmj.com/content/67/8/1380.long
http://www.ncbi.nlm.nih.gov/pubmed/29653941?tool=bestpractice.com
Faecal calprotectin
Faecal calprotectin testing is not recommended by guidelines to exclude or monitor microscopic colitis.[1]Miehlke S, Verhaegh B, Tontini GE, et al. Microscopic colitis: pathophysiology and clinical management. Lancet Gastroenterol Hepatol. 2019 Apr;4(4):305-14.
http://www.ncbi.nlm.nih.gov/pubmed/30860066?tool=bestpractice.com
Despite a few studies suggesting slightly elevated levels of faecal calprotectin in patients with microscopic colitis compared with patients without an organic cause of diarrhoea and irritable bowel syndrome, its role in clinical practice is uncertain.[49]Batista L, Ruiz L, Ferrer C, et al. Usefulness of fecal calprotectin as a biomarker of microscopic colitis in a cohort of patients with chronic watery diarrhoea of functional characteristics. Dig Liver Dis. 2019 Dec;51(12):1646-51.
http://www.ncbi.nlm.nih.gov/pubmed/31383457?tool=bestpractice.com
[50]von Arnim U, Wex T, Ganzert C, et al. Fecal calprotectin: a marker for clinical differentiation of microscopic colitis and irritable bowel syndrome. Clin Exp Gastroenterol. 2016 Apr 21;9:97-103.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4849404
http://www.ncbi.nlm.nih.gov/pubmed/27147826?tool=bestpractice.com
Some centres may, however, include this test in the diagnostic work-up as an elevated result indicates inflammation.