Investigations
1st investigations to order
chest x-ray
Test
Take a focused history to make the diagnosis of acute aspiration. However, this should be corroborated using imaging; order a chest x-ray as first-line
Be aware that chest x-ray changes may only be seen if acute aspiration has led to aspiration pneumonitis or pneumonia. Bear in mind that aspiration pneumonitis and pneumonia can also co-exist.
Also note that the pattern of chest x-ray changes varies depending on the positioning of the patient when they aspirate, and the mechanism of aspiration.
Look for patchy, bilateral airspace consolidations with a perihilar and basilar distribution following aspiration.[27]
In general, the right lung is involved more frequently than the left lung. Any material that is aspirated is more likely to end up in the right lung because:
The angle between the trachea and the right main bronchus is obtuse
The right main bronchus is wider and more vertical than the left main bronchus.
The most commonly involved segments are the superior and posterobasal segments of the right lower lobe and the posterior segment of the right upper lobe, because of their dependent location if the patient aspirates while lying in a supine position.
However, other segments can be involved if the patient is not lying in a supine position. For example, if the patient is lying on the left side, the left lung may show consolidation.
In acute on chronic aspiration, the consolidation may predominantly be in the basal segments.
Barium aspiration may show dense opacities in the mid- and lower lungs, with a miliary pattern.[38][39]
[Figure caption and citation for the preceding image starts]: A. Portable upright chest x-ray before aspiration; B. Chest x-ray 1 hour after aspiration, showing bilateral diffuse alveolar infiltrates, worse at the bases on the right sideFrom the collection of Dr Henri Colt [Citation ends].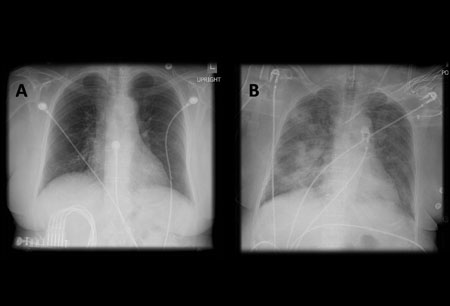
Chest x-ray findings of aspiration pneumonitis usually develop within 2 hours of aspiration and sometimes resolve quickly. However, opacities due to aspiration pneumonia can develop days later and can take weeks to resolve.
Result
patchy, bilateral airspace consolidations
blood tests
Test
Order blood tests to differentiate between chemical pneumonitis and pneumonia; high white cell count, procalcitonin, or C-reactive protein indicates infection.
Result
high white cell count, procalcitonin, or C-reactive protein indicates infection
Investigations to consider
chest CT
Test
Order chest CT if the patient does not improve with initial treatment, to rule out complications of aspiration such as empyema or lung abscess. Chest CT is better than chest-ray for visualising these complications.
Chest CT may show:
Extensive consolidation with cavitation if a lung abscess is present
Pleural effusion, often with loculations, if an empyema is present
Opacities in the posterior segments of the upper lobes and the superior segments of the lower lobes if a chemical pneumonitis or pneumonia is present. CT can precisely delineate the location of the lobar and segmental opacities. If the patient has significant aspiration, CT findings may be indistinguishable from those of acute respiratory distress syndrome. Note that the pattern of changes on CT varies depending on the positioning of the patient when they aspirate and the mechanism of aspiration - see Chest x-ray above
Thickened interlobular septae, subpleural lines, and subpleural cysts following aspiration of barium. These findings may be present for a long time (even 1 year) after aspiration
Aspiration of fat or contrast material, which can sometimes be determined by measuring the tissue attenuation.
Result
extensive consolidation with cavitation if a lung abscess is present
pleural effusion, often with loculations, if an empyema is present
opacities in dependent segments if a chemical pneumonitis or pneumonia is present
thickened interlobular septae, subpleural lines, and subpleural cysts following aspiration of barium
aspiration of fat or contrast material
bronchoscopy
Test
If you suspect a substantial amount of gastric content (>20-25 mL) is likely to have been aspirated, organise urgent (within a few hours) bronchoscopy and suctioning to remove any aspirated gastric fluid and solid material from the central airways.
Organise early bronchoscopy if you suspect the patient has aspirated barium during gastrointestinal studies, to remove the barium from their airway.
Get help from the critical care team if the patient has significant hypoxia or respiratory distress because bronchoscopy may cause further deterioration.
Other indications for bronchoscopy are to:
Clear the airway if the aspirated material is particulate or if there is radiographic evidence of lobar or segmental collapse
Collect quantitative cultures on bronchoalveolar lavage or protected specimen brush, which can be used to guide antibiotic therapy, particularly in patients who do not respond to empirical antibiotic treatment
Investigate alternative diagnoses that can cause a similar radiographic pattern to acute aspiration. These include acute respiratory distress syndrome imitators such as COVID-19 pneumonitis/pneumonia, acute interstitial pneumonitis (Hamman-Rich syndrome), acute eosinophilic pneumonia, cryptogenic organising pneumonia, diffuse alveolar haemorrhage, and acute hypersensitivity pneumonitis.[41]
[Figure caption and citation for the preceding image starts]: Bronchoscopy showing barium aspiration in a lung transplant patient in the right mainstem bronchus after a barium swallow studyFrom the collection of Dr Kamran Mahmood [Citation ends].
Result
airway erythema
arterial blood gas
Test
Aspiration may cause hypoxaemia.
Result
reduced oxygen tension
Use of this content is subject to our disclaimer