Syncope at presentation is usually associated with worse outcomes. A deadly triad of hypotension/shock (not syncope), lack of chest or back pain (presumably related to delay in diagnosis), and branch vessel involvement is also described.[73]Suzuki T, Mehta RH, Ince H, et al. Clinical profiles and outcomes of acute type B aortic dissection in the current era: lessons from the International Registry of Aortic Dissection (IRAD). Circulation. 2003 Sep 9;108 Suppl 1:II312-7.
http://circ.ahajournals.org/content/108/10_suppl_1/II-312.long
http://www.ncbi.nlm.nih.gov/pubmed/12970252?tool=bestpractice.com
Left untreated, the natural history of proximal acute aortic dissection is of false channel rupture with fatal exsanguination in 50% to 60% of patients within 24 hours.[74]Svensson LG, Kouchoukos NT, Miller DC, et al. Expert consensus document on the treatment of descending thoracic aortic disease using endovascular stent-grafts. Ann Thorac Surg. 2008 Jan;85(1 suppl):S1-41.
http://www.ncbi.nlm.nih.gov/pubmed/18083364?tool=bestpractice.com
Patients with non-operated type A dissection rarely live past the acute event.[5]Fleischmann D, Afifi RO, Casanegra AI, et al. Imaging and surveillance of chronic aortic dissection: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging. 2022 Mar;15(3):e000075.
https://www.ahajournals.org/doi/full/10.1161/HCI.0000000000000075?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/35172599?tool=bestpractice.com
In tertiary high-volume referral centers for aortic diseases, the surgical mortality for ascending and hemiarch replacement with or without root replacement is as low as 10% to 20%.[5]Fleischmann D, Afifi RO, Casanegra AI, et al. Imaging and surveillance of chronic aortic dissection: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging. 2022 Mar;15(3):e000075.
https://www.ahajournals.org/doi/full/10.1161/HCI.0000000000000075?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/35172599?tool=bestpractice.com
The midterm survival of surgically corrected ascending dissections at 1, 3, and 5 years is 95%, 93%, and 89%, respectively.[5]Fleischmann D, Afifi RO, Casanegra AI, et al. Imaging and surveillance of chronic aortic dissection: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging. 2022 Mar;15(3):e000075.
https://www.ahajournals.org/doi/full/10.1161/HCI.0000000000000075?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/35172599?tool=bestpractice.com
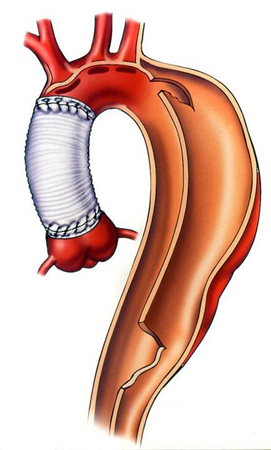
The 10-year survival after surgery of ascending aortic dissection is 52%. Freedom from re-operation at both 5 and 10 years ranges from 59% to 95%.[75]Subramanian S, Roselli EE. Thoracic aortic dissection: long-term results of endovascular and open repair. Semin Vasc Surg. 2009 Jun;22(2):61-8.
http://www.ncbi.nlm.nih.gov/pubmed/19573743?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Dissection status post-proximal repair with late distal aneurysm [Citation ends].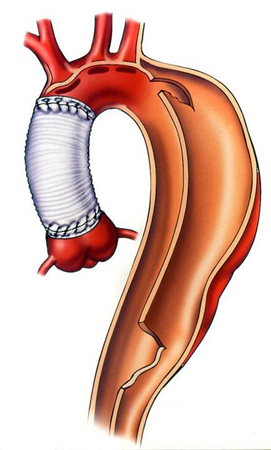
Patients with uncomplicated type B dissection (i.e., those without signs of rupture, rapid expansion, or branch vessel malperfusion; approximately 60% to 70% of type B dissections) can be safely managed medically. Almost all patients with initially uncomplicated type B dissection therefore progress to the chronic phase with a 20% to 50% risk of late adverse events.[5]Fleischmann D, Afifi RO, Casanegra AI, et al. Imaging and surveillance of chronic aortic dissection: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging. 2022 Mar;15(3):e000075.
https://www.ahajournals.org/doi/full/10.1161/HCI.0000000000000075?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/35172599?tool=bestpractice.com
Complicated type B dissections (ie, those requiring urgent endovascular or surgical repair for aortic rupture, rapid expansion, or branch vessel malperfusion, as well as those patients too sick to undergo an acute intervention) represent approximately 0% to 40% of type B dissections. The in-hospital mortality of these patients is approximately 20%.[5]Fleischmann D, Afifi RO, Casanegra AI, et al. Imaging and surveillance of chronic aortic dissection: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging. 2022 Mar;15(3):e000075.
https://www.ahajournals.org/doi/full/10.1161/HCI.0000000000000075?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/35172599?tool=bestpractice.com
Late degeneration of the dissected aorta into a false lumen aneurysm occurs in 30% to 50% of patients.[62]Eggebrecht H, Nienaber CA, Neuhauser M, et al. Endovascular stent-graft placement in aortic dissection: a meta-analysis. Eur Heart J. 2006 Feb;27(4):489-98.
http://www.ncbi.nlm.nih.gov/pubmed/16227309?tool=bestpractice.com
Following treatment, patients remain at risk for further aneurysmal degeneration of remaining diseased aorta.
The 5-year survival after thoracic endovascular aortic repair (TEVAR) for acute type B aortic dissection is 81%.[76]Yoshitake A, Okamoto K, Yamazaki M, et al. Comparison of aortic arch repair using the endovascular technique, total arch replacement and staged surgery. Eur J Cardiothorac Surg. 2017 Jun 1;51(6):1142-8.
https://academic.oup.com/ejcts/article/51/6/1142/3061960
http://www.ncbi.nlm.nih.gov/pubmed/28329146?tool=bestpractice.com
Longer term outcomes after TEVAR for the treatment of either acute or chronic type B aortic dissection are currently unknown.