Aetiology
Aortic dissection results from an intimal tear that extends into the media of the aortic wall. Cystic medial degeneration predisposes to intimal disruption and is characterised by elastin, collagen, and smooth muscle breakdown in the lamina media. Bleeding from the vasa vasorum can also lead to this condition.
Inherited conditions that lead to medial degeneration provide a morphological substrate for developing aortic dissection. Marfan syndrome and Ehlers-Danlos syndrome lead to weakening of the media, thus predisposing to aortic dilation and dissection. Bicuspid aortic valve may be associated with a non-specific connective-tissue disease, predisposing to aortic aneurysm and/or dissection. Aortic atherosclerosis with dilation, and inflammatory or traumatic conditions or infections, may also predispose to aneurysmal degeneration and dissection. Although rare, iatrogenic causes of aortic dissection include aortic manipulation associated with cardiac surgery or interventional procedures.[10] It is unclear if these iatrogenic complications occur in patients already predisposed by the aetiologies described above.
[Figure caption and citation for the preceding image starts]: Trans-oesophageal echocardiography (transverse aortic section) showing a circumferential dissection of the ascending aorta in a 30-year-old patient with features of Marfan's syndromeBouzas-Mosquera A, Solla-Buceta M, Fojón-Polanco S. Circumferential aortic dissection. BMJ Case Reports 2009; doi:10.1136/bcr.2007.049908 [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan showing dissecting aneurysm in a 45-year-old patient with Marfan syndrome experiencing chest pain [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan showing dissecting aneurysm in a 45-year-old patient with Marfan syndrome experiencing chest pain [Citation ends].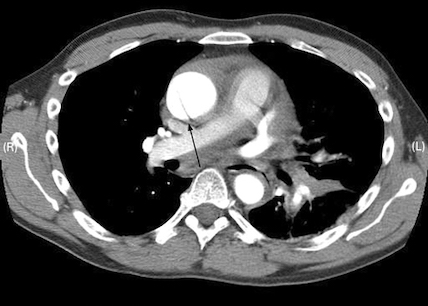
Pathophysiology
An intimal tear is the initial event, with subsequent degeneration of the medial layer of the aortic wall. Blood then passes through the media, propagating distally or proximally and creating a false lumen. As the dissection propagates, flow through the false lumen can occlude flow through branches of the aorta, including the coronary, brachiocephalic, intercostal, visceral and renal, or iliac vessels.
The intimal tears of dissection most commonly occur just above the sinotubular junction or just distal to the left subclavian artery.[11] Regardless of where tears occur in the aorta, there may be both a retrograde and antegrade extension of the dissection.[8] Retrograde dissections starting in the ascending aorta can lead to aortic incompetence by separating the aortic valve from the aortic root.
Static narrowing of side-branches occurs when the line of dissection intersects the vessel origin and the aortic haematoma has propagated into the vessel wall, leading to stenosis or occlusion of the side-branch. Dynamic compression occurs when the dissection flap is on the opposite side of the side-branch origin. Obstruction of the side-branch occurs during diastole, when the true lumen collapses and the intimal flap closes over the ostium of the branch vessel. Flow is restored during systole. Both static and dynamic compression of a side-branch or a combination of both can lead to total flow occlusion and end-organ ischaemia.[8] Subsequent clinical manifestations occur depending on the extent of propagation of the dissection with subsequent organ malperfusion.[8][12]
Laplace's law describes wall stress as directly proportional to pressure and radius, and inversely proportional to wall thickness. Thus, factors that weaken the aortic wall, particularly the lamina media, lead to increased risk of aneurysm formation and dissection, and a cycle of increasing wall stress.[8]
Classification
Stanford[1]
Type A: Dissection involves the ascending aorta with or without involvement of the arch and descending aorta.
Type B: Dissection does not involve the ascending aorta. Predominantly involves only the descending thoracic (distal to the left subclavian artery) and/or abdominal aorta.
DeBakey[4]
Type 1: Tear originates in the ascending aorta and involves the ascending aorta and aortic arch, and variable amounts of the descending thoracic aorta.
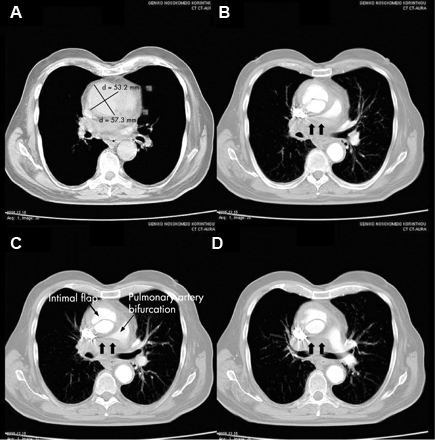
Type 2: Dissection is confined to the ascending aorta. [Figure caption and citation for the preceding image starts]: CT of a 71-year-old man showing type II dissecting aneurysm of the ascending aorta. Haematoma around the proximal segment of the ascending aorta (panels A-D) compressed the right pulmonary artery, almost occluding its patency and limiting the perfusion of the reciprocal lung [Citation ends].
Type 3: Tear originates distal to the left subclavian artery and extends through the thoracic aorta (3A) or extends beyond the visceral segment (3B).
Society for Vascular Surgery/Society of Thoracic Surgeons (SVS/STS) chronicity classification[3]
Type A and B aortic dissection can be further classified into phases according to the time elapsed since first onset of symptoms.[2][3][5]
The European Society for Cardiology defines these time frames as:
<14 days (acute)
15-90 days (subacute)
>90 days (chronic), which includes type B dissection, and type A dissection with persisting dissection of the descending aorta following surgery.
In addition to these time frames, the Society for Vascular Surgery and Society for Vascular Surgeons (SVS/STS) classifies type A and B aortic dissection <24 hours since first onset of symptoms as 'hyperacute'.[3]
Use of this content is subject to our disclaimer