Investigations
1st investigations to order
ECG
Test
Perform a 12-lead resting ECG.[5]
This will show continuous regular electrical activity (if a regular atrioventricular [AV] block is present), most commonly a saw-tooth pattern.[5]
Typically there is 2:1 AV block and the characteristic ventricular rate is 150 beats per minute. However, variable block may occur leading to an irregular rate.
Further classic ECG findings depend on the type of flutter (typical, reverse typical, or atypical – see More info: Types of atrial flutter [with ECG examples] below), but this does not change initial management.
The ECG pattern may fluctuate between atrial flutter and atrial fibrillation. See our topic New-onset atrial fibrillation.
[Figure caption and citation for the preceding image starts]: Typical atrial flutter with variable (3 to 4:1) blockFrom the collection of Dr K.C. Wu [Citation ends].
 [Figure caption and citation for the preceding image starts]: Atrial fibrillationFrom the collection of Dr K.C. Wu [Citation ends].
[Figure caption and citation for the preceding image starts]: Atrial fibrillationFrom the collection of Dr K.C. Wu [Citation ends].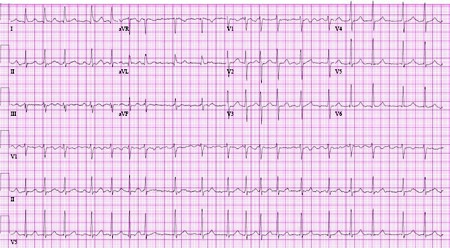
Practical tip
Always suspect atrial flutter if there is a narrow complex tachycardia at 150 bpm (or in the range 130-170 bpm).
Examine all the ECG leads carefully for atrial flutter.
Ventricular rate is a fraction of the atrial rate, for example:
2:1 block = 150 bpm
3:1 block = 100 bpm
4:1 block = 75 bpm.
More info: Types of atrial flutter (with ECG examples)
Further classic ECG findings depend on the type of flutter.
Typical form (anticlockwise isthmus-dependent): negatively directed saw-tooth atrial deflections (f waves) in leads II, III, and aVF, and positive deflections in V1 with atrial rates of 250 to 330 bpm.[5][Figure caption and citation for the preceding image starts]: Typical atrial flutter with variable (3 to 4:1) blockFrom the collection of Dr K.C. Wu [Citation ends].
 [Figure caption and citation for the preceding image starts]: Close-up images of leads V1, II, III, aVF demonstrating the features of typical atrial flutter: positive saw-tooth deflections in lead V1 and negative deflections in leads II, III, aVF (arrows)From the collection of Dr K.C. Wu [Citation ends].
[Figure caption and citation for the preceding image starts]: Close-up images of leads V1, II, III, aVF demonstrating the features of typical atrial flutter: positive saw-tooth deflections in lead V1 and negative deflections in leads II, III, aVF (arrows)From the collection of Dr K.C. Wu [Citation ends].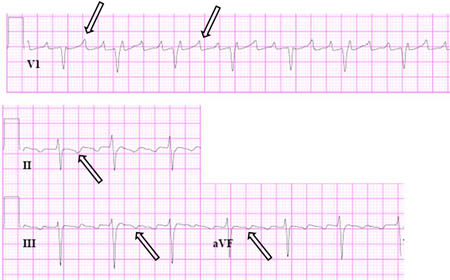
Reverse typical form (clockwise isthmus-dependent): positive flutter waves in leads II, III, and aVF, and negative flutter waves in lead V1.[Figure caption and citation for the preceding image starts]: Reverse typical atrial flutterFrom: Waldo AL. Heart. 2000 Aug;84(2):227-32; used with permission [Citation ends].
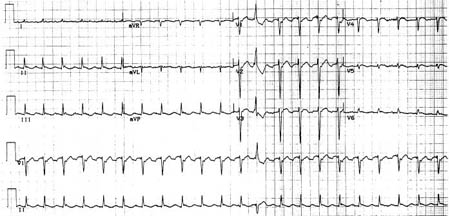 [Figure caption and citation for the preceding image starts]: Selected leads from a patient with reverse typical atrial flutter confirmed at electrophysiological study. The atrial deflections are negative in lead V1 and positive in leads II, III, aVF (arrows)Adapted from: Waldo AL. Heart. 2000 Aug;84(2):227-32; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Selected leads from a patient with reverse typical atrial flutter confirmed at electrophysiological study. The atrial deflections are negative in lead V1 and positive in leads II, III, aVF (arrows)Adapted from: Waldo AL. Heart. 2000 Aug;84(2):227-32; used with permission [Citation ends].
Atypical form (non-isthmus-dependent): continuous undulation of the atrial complex, not meeting criteria for typical or reverse typical flutter, with atrial rates >240 bpm.[2][4][21][Figure caption and citation for the preceding image starts]: Atypical flutter with right bundle branch blockFrom the collection of Dr K.C. Wu [Citation ends].
 [Figure caption and citation for the preceding image starts]: Close up of leads II, III, V1 showing the continuously undulating pattern of atrial deflections not fitting the criteria for typical or reverse typical atrial flutterFrom the collection of Dr K.C. Wu [Citation ends].
[Figure caption and citation for the preceding image starts]: Close up of leads II, III, V1 showing the continuously undulating pattern of atrial deflections not fitting the criteria for typical or reverse typical atrial flutterFrom the collection of Dr K.C. Wu [Citation ends].
If a patient has atrial flutter with 2:1 block, the diagnosis may not be clear on ECG. Consider use of vagal manoeuvres (such as carotid sinus massage) or intravenous adenosine to confirm the diagnosis, while monitoring the ECG.[5]
If a vagal manoeuvre is performed, this can unmask atrial activity (by causing slowing of AV node conduction and induction of intermittent AV block) and reveal dissociated P waves.[5]
Only use adenosine if deemed necessary for diagnosis and if resuscitation equipment is available.[5]
Consider a 24-hour ambulatory ECG recording. However, tachycardia episodes are usually sporadic and may not be frequent enough to be recorded on ambulatory monitoring.[5]
Result
continuous regular electrical activity (if a regular AV block is present), most commonly a saw-tooth pattern
typically there is a 2:1 AV block with a ventricular rate of 150 bpm
changes diagnostic of typical, reverse typical, or atypical atrial flutter
full blood count
Test
Always order in all patients.
Result
may indicate systemic illness (such as infection)
thyroid function tests
Test
To rule out underlying thyroid disease.
Result
normal; abnormal if underlying thyroid disease is present
renal function and serum electrolytes
Test
Electrolyte abnormalities are generally not the sole cause of atrial flutter, but imbalances should be checked and corrected.
Result
normal; abnormal if underlying electrolyte disturbances are present
chest x-ray
Test
Order a chest x-ray; atrial flutter is often associated with a known history of, or suggestive presentation for, lung disease (e.g., pulmonary embolism).
Result
normal; may be abnormal if underlying lung disease is present
transthoracic echocardiography (TTE)
Test
Always request a TTE as a baseline investigation to check:[5]
Atrial sizes, ventricular function, and for valvular and pericardial disease
Right ventricular systolic pressures, which may indicate the presence or absence of pulmonary hypertension seen in underlying lung disease.
Result
possible structural heart disease
Investigations to consider
pulmonary function tests
Test
Recommended by the European Society of Cardiology if you suspect lung disease as a cause.[5] However, in practice, other investigations such as high-resolution CT or CT pulmonary angiography may be used instead.
Result
normal; abnormal if underlying lung disease is present
digitalis level
Test
Consider if the patient is taking a digitalis drug (e.g., digoxin) to check for digitalis toxicity, although this is a rare cause of atrial flutter.
Result
normal; elevated in digitalis toxicity
high-sensitivity troponin
Test
Order if you suspect acute myocardial infarction (MI). See our topics ST-elevation myocardial infarction and Non-ST elevation myocardial infarction.
Result
normal; elevated in MI
CT pulmonary angiography with clinical probability scoring
Test
Consider if you suspect pulmonary embolism, if indicated by clinical probability scoring.[22] See our topic Pulmonary embolism.
Result
normal; direct visualisation of thrombus in a pulmonary artery in pulmonary embolism
electrophysiological studies
Test
Electrophysiology studies require specialist input from an electrophysiologist and are usually indicated to establish the diagnosis of atrial flutter, particularly when catheter ablation is planned.[5]
Electrophysiological studies may also be used if:
Atrial flutter is recurrent, particularly if anti-arrhythmic drug therapy has been ineffective or not tolerated because of adverse effects
The ventricular rate is difficult to control with drugs
Atrial flutter persists despite resolution of the acute underlying illness.
Result
map of re-entrant circuit
atrial electrogram
Test
Although the diagnosis of atrial flutter is usually clear on the 12-lead ECG, an atrial electrogram (which should be performed by a specialist) can help visualise flutter waves if the diagnosis is uncertain. However, it is rarely used in practice.
Result
flutter waves
exercise tolerance testing
Test
May be useful if the patient has apparent pre-excitation or a catecholamine-dependent arrhythmia.[5] Can also be considered if there is a history that suggests an exercise-induced arrhythmia.
Result
may demonstrate exercise-induced arrhythmia
myocardial ischaemia testing
Test
Organise myocardial ischaemia testing if the patient has angina or if you suspect underlying ischaemia (e.g., if significant risk factors for coronary artery disease are present).[5]
Result
may show evidence of myocardial ischaemia
Use of this content is subject to our disclaimer