Investigations
1st investigations to order
ECG
Test
Record and interpret a resting 12-lead ECG within 10 minutes of the point of first medical contact.[1]
Discuss the patient immediately with the cardiology team and involve senior support if the ECG shows evidence of ST-elevation myocardial infarction (STEMI) to activate your local STEMI protocol.[1] See ST-elevation myocardial infarction.
Be aware that the ECG may be normal in more than 30% of patients.[1] Furthermore, unstable angina is generally not associated with ECG changes (based on the opinion of our experts).
However, abnormal findings that suggest non-ST-elevation ACS include:[1]
ST depression; this indicates a worse prognosis
Transient ST elevation
T-wave changes.
Record additional leads if the standard leads are inconclusive, if total vessel occlusion is suspected, or in cases of suspected inferior STEMI.[1]
Leads V7–V9 may detect left circumflex artery occlusion and leads V3R and V4R may detect right ventricular myocardial infarction.[1]
Order repeated resting ECGs if the patient has recurrent symptoms or you are unsure about the diagnosis.[1]
Always compare the current ECG with previous ECGs wherever possible.[1]
How to record an ECG. Demonstrates placement of chest and limb electrodes.
[Figure caption and citation for the preceding image starts]: Position of ECG leads V7-V9Image used with permission from BMJ 2002;324:831 [Citation ends].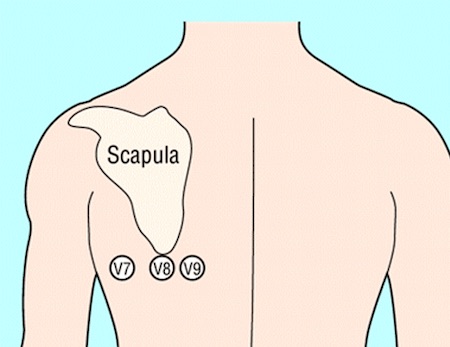 [Figure caption and citation for the preceding image starts]: Position of right precordial ECG leads V3R and V4RImage used with permission from BMJ 2002;324:831 [Citation ends].
[Figure caption and citation for the preceding image starts]: Position of right precordial ECG leads V3R and V4RImage used with permission from BMJ 2002;324:831 [Citation ends].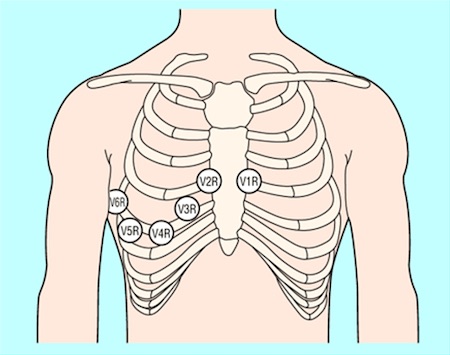 [Figure caption and citation for the preceding image starts]: ECG showing inferolateral ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing inferolateral ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].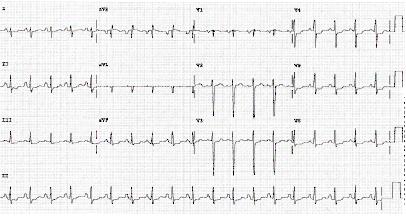 [Figure caption and citation for the preceding image starts]: ECG showing T wave inversion in leads V1-V4, III and aVF.BMJ Learning/Professor Kevin Tanner; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing T wave inversion in leads V1-V4, III and aVF.BMJ Learning/Professor Kevin Tanner; used with permission [Citation ends].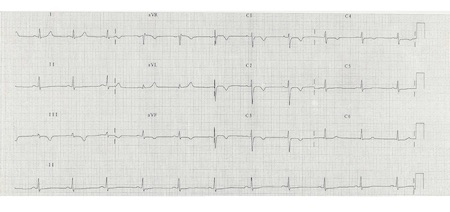
Result
typically no ECG changes; ST depression (indicates a worse prognosis), transient ST elevation, and T-wave changes may be seen
high-sensitivity troponin
Test
Measure high-sensitivity cardiac troponin (hs-cTn) immediately after presentation and obtain results within 60 minutes in all patients with suspected acute coronary syndrome to rule out acute myocardial infarction; there will be no dynamic rise above the 99th percentile in patients with unstable angina.[1]
Use a diagnostic algorithm (ideally the 0/1 hour protocol recommended by the European Society of Cardiology, with blood draws at 0 hours and 1 hour) to measure hs-cTn over time in all patients except those who are clinically unstable. Cut-off values for hs-cTn are dependent on the assay used; check your local protocol.[1]
Use the algorithm in the context of other clinical criteria such as a detailed history of the chest pain and any ECG findings.[1]
Some patients may need an additional measurement of troponin at 3 hours (e.g., if the first two hs-cTn measurements of the 0/1 algorithm are inconclusive, and no alternative diagnoses explaining the condition have been made).
Practical tip
Reassess the patient if they have a raised hs-cTn.
Troponin can be acutely raised due to other causes such as myocarditis, aortic dissection, or acute pulmonary embolism.[73]
Chronic elevation of high-sensitivity troponin is also common in patients with renal dysfunction and heart failure.[1]
Troponin levels may remain elevated for 1-2 weeks following recent myocardial infarction and/or percutaneous coronary intervention.
Interpret hs-cTn in the context of the clinical scenario.
Result
no dynamic elevation above the 99th percentile
chest x-ray
Test
The UK National Institute for Health and Care Excellence recommends ordering a chest x-ray only if you suspect other diagnoses or to rule out complications of acute coronary syndrome.[73] However, in our expert’s opinion you should order a chest x-ray for all patients with acute chest pain to look for other causes such as pneumothorax or a widened mediastinum in aortic dissection, or complications of acute coronary syndrome such as pulmonary oedema due to heart failure.[77]
Practical tip
Ensure an ECG is recorded and interpreted before considering a chest x-ray. If the ECG indicates ST-elevation myocardial infarction, refer the patient immediately to cardiology for consideration of primary percutaneous coronary intervention to avoid the delay that may be associated with requesting a chest x-ray.
Result
other causes of acute chest pain such as pneumothorax or a widened mediastinum in aortic dissection
complications of acute coronary syndrome such as pulmonary oedema due to heart failure
full blood count
Test
Check full blood count to evaluate:
Thrombocytopenia to estimate risk of bleeding; unstable angina treatment increases the risk of bleeding
Possible secondary causes of unstable angina (i.e., secondary blood loss, anaemia)
Anaemia is common in unstable angina and persistent or worsening anaemia in acute coronary syndrome is associated with increased mortality and major bleeding.[1]
Result
normal, thrombocytopenia, anaemia
urea, electrolytes, and creatinine
Test
Measure renal function to:
Determine serum creatinine and estimated glomerular filtration rate; these are key elements in assessing the Global Registry of Acute Coronary Events (GRACE) risk score[1]
Determine the choice/dose of anticoagulant[1]
Prevent contrast-induced nephropathy if an invasive strategy is planned in a patient with chronic kidney disease.[1]
Be aware that a patient with chronic kidney disease may have a chronically raised troponin.[2] Patients with chronic kidney disease may also have electrolyte abnormalities that can cause ECG abnormalities.
Result
baseline levels
liver function tests
Test
Measure liver function to include in the assessment of bleeding risk before starting anticoagulation.
Result
baseline levels
blood glucose
Test
Check blood glucose in any patient with known diabetes or hyperglycaemia on admission to hospital regardless of a history of diabetes.[1]
Monitor blood glucose levels frequently if the patient has known diabetes or hyperglycaemia on admission.[1]
Manage hyperglycaemia in patients admitted with acute coronary syndrome by keeping blood glucose <11 mmol/L (<198 mg/dL) while avoiding hypoglycaemia.[71] See Management of hyperglycaemia under Management recommendations.
Result
normal, hyperglycaemia
C-reactive protein (CRP)
Test
The UK National Institute for Health and Care Excellence does not recommend using CRP to diagnose an acute coronary syndrome.[73] However, in our expert’s opinion, CRP is commonly ordered to rule out other causes of acute chest pain (e.g., pneumonia).
Result
elevated if infection present
lipid profile
Test
Recommended for risk stratification.
Target LDL <2.6 mmol/L (<100 mg/dL) if coronary artery disease present.
Result
normal or increased total cholesterol and LDL
coagulation profile
Test
Recommended at baseline, as treatment options affect coagulation.
Result
normal
Investigations to consider
echocardiography
Test
Organise urgent echocardiography for any patient with signs of acute heart failure or haemodynamic instability or who is in cardiac arrest.[1] This should only be performed by those with consultant training.
Use a point-of-care transthoracic echocardiogram to:
Look for regional wall motion abnormalities of the left ventricle in patients with an atypical presentation or equivocal ECG.[1][2][85][86]
Look for mechanical complications of acute MI (see Acute MI complications - mechanical below):[86]
Left ventricular function
Right ventricular function
Ventricular septal rupture
Left ventricular free wall rupture
Acute mitral regurgitation
Pericardial effusion
Cardiac tamponade.
Suggest alternative aetiologies associated with chest pain (e.g., acute aortic disease, pulmonary embolism).[1][86]
A pre-discharge echocardiogram is indicated for all patients post-acute MI to assess left ventricular function after coronary reperfusion therapy and to guide prognostication.[71][87]
Result
no new regional wall motion abnormalities
invasive coronary angiography
Test
Invasive coronary angiography (with or without revascularisation) may be considered by the cardiology team for a patient with suspected unstable angina (with a negative troponin testing result) based on the risk assessment and clinical presentation.[71] Patients with unstable angina have a significantly lower risk of death compared with those with non-ST-elevation myocardial infarction and get less benefit from an immediate invasive approach.[88] An inpatient invasive strategy (coronary angiography within 72 hours of admission, with follow-on percutaneous coronary intervention if indicated) is generally recommended for patients with a high index of suspicion for unstable angina, particularly for those who have an intermediate or higher risk of adverse cardiovascular events.[1]
Result
flow-limiting stenosis
functional (stress) testing
Test
Functional (stress) testing (e.g., stress echocardiography, perfusion/stress cardiac magnetic resonance [CMR] imaging, myocardial perfusion scan) may be considered by the cardiology team as part of the initial work-up in patients with suspected acute coronary syndrome but non-elevated (or inconclusive) high-sensitivity cardiac troponin (hs-cTn), no ECG changes, and no recurrence of pain.[1]
Result
stress echocardiography: reversible regional wall motion abnormalities
perfusion/stress CMR: reversible (ischaemic) defect
myocardial perfusion imaging: unmatched perfusion defect between rest and stress scan
coronary computed tomography angiography
Test
Coronary computed tomography angiography may be considered by the cardiology team if the patient has no ischaemic changes on ECG and has been pain-free for several hours.[1]
Result
flow-limiting stenosis
Use of this content is subject to our disclaimer
