The gold standard for establishing the diagnosis of myocarditis is the endomyocardial biopsy (EMB). However, this test has a yield of 10% to 20% and is not indicated for most patients with suspected myocarditis.[4]Dec GW. Introduction to clinical myocarditis. In: Cooper LT, ed. Myocarditis: from bench to bedside. Totowa, NJ: Humana Press; 2003:257-81.[55]Bozkurt B, Colvin M, Cook J, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 2016 Nov 3;134(23):e579-646.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000455
http://www.ncbi.nlm.nih.gov/pubmed/27832612?tool=bestpractice.com
Thus, the appropriate evaluation of patients with suspected myocarditis begins with a complete history and physical examination. If myocarditis is still suspected, then further work-up with a 12-lead ECG, laboratory evaluation of cardiac biomarkers and two-dimensional echo should be performed.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[21]Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126.
https://academic.oup.com/eurheartj/article/43/40/3997/6675633?login=false
http://www.ncbi.nlm.nih.gov/pubmed/36017572?tool=bestpractice.com
[56]Expert Panel on Cardiac Imaging, Rajiah P, Kirsch J, Bolen MA, et al. ACR Appropriateness Criteria® Nonischemic myocardial disease with clinical manifestations (ischemic cardiomyopathy already excluded). J Am Coll Radiol. 2021 May;18(5S):S83-105.
https://www.jacr.org/article/S1546-1440(21)00115-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33651982?tool=bestpractice.com
There is no general consensus on which patients should undergo EMB; local guidelines should be consulted.[5]Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology working group on myocardial and pericardial diseases. Eur Heart J. 2013 Sep;34(33):2636-48.
https://academic.oup.com/eurheartj/article/34/33/2636/408735
http://www.ncbi.nlm.nih.gov/pubmed/23824828?tool=bestpractice.com
[55]Bozkurt B, Colvin M, Cook J, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 2016 Nov 3;134(23):e579-646.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000455
http://www.ncbi.nlm.nih.gov/pubmed/27832612?tool=bestpractice.com
[57]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
[58]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[59]Seferović PM, Tsutsui H, McNamara DM, et al. Heart Failure Association of the ESC, Heart Failure Society of America and Japanese Heart Failure Society position statement on endomyocardial biopsy. Eur J Heart Fail. 2021 Jun;23(6):854-71.
https://onlinelibrary.wiley.com/doi/10.1002/ejhf.2190
http://www.ncbi.nlm.nih.gov/pubmed/34010472?tool=bestpractice.com
Contrast-enhanced cardiac magnetic resonance imaging (MRI) has been shown to assist in the diagnosis of myocarditis by providing detailed tissue characterisation.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[21]Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126.
https://academic.oup.com/eurheartj/article/43/40/3997/6675633?login=false
http://www.ncbi.nlm.nih.gov/pubmed/36017572?tool=bestpractice.com
[56]Expert Panel on Cardiac Imaging, Rajiah P, Kirsch J, Bolen MA, et al. ACR Appropriateness Criteria® Nonischemic myocardial disease with clinical manifestations (ischemic cardiomyopathy already excluded). J Am Coll Radiol. 2021 May;18(5S):S83-105.
https://www.jacr.org/article/S1546-1440(21)00115-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33651982?tool=bestpractice.com
[60]Friedrich MG, Strohm O, Schulz-Menger, et al. Contrast media-enhanced magnetic resonance imaging visualizes myocardial changes in the course of viral myocarditis. Circulation. 1998 May 12;97(18):1802-9.
https://www.ahajournals.org/doi/full/10.1161/01.cir.97.18.1802
http://www.ncbi.nlm.nih.gov/pubmed/9603535?tool=bestpractice.com
Positron emission tomography-computed tomography (PET-CT), especially 18F-fluorodeoxyglucose (FDG) PET-CT, can also be of value.[21]Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126.
https://academic.oup.com/eurheartj/article/43/40/3997/6675633?login=false
http://www.ncbi.nlm.nih.gov/pubmed/36017572?tool=bestpractice.com
The approach may be modified for children with suspected myocarditis. The 2021 American Heart Association (AHA) statement on paediatric myocarditis lays out a new paradigm for myocarditis based on diagnostic strata and also provides guidance on approach.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
The AHA statement classifies myocarditis as 1) biopsy proven, 2) cardiac MRI confirmed, 3) clinically suspected, and 4) possible myocarditis.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
Thus, when possible and safe, EMB continues to be the reference standard for diagnosis of confirmed myocarditis in children. In the absence of biopsy, clinical diagnosis with or without MRI will provide necessary information for the diagnosis.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
History
Patients presenting with myocarditis are usually aged <50 years. A history of viral prodrome 2-3 weeks prior to the onset of myocarditis is commonly present. Symptoms may include chest pain, dyspnoea, orthopnoea, syncope, fatigue, and palpitations.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
In children, a viral prodrome will be the most common history, followed by history suggestive of arrhythmias or syncope.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
The common symptoms include fever, fatigue, respiratory symptoms, abdominal pain, emesis, and lethargy.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
The patient's medical history may be significant for autoimmune disease such as collagen-vascular diseases as well as inflammatory bowel disease, diabetes mellitus, sarcoidosis, thyrotoxicosis, granulomatosis with polyangiitis (formerly known as Wegener's granulomatosis), or Loeffler's syndrome. In addition, a history of travel to endemic areas where causative organisms are found may suggest a specific infectious aetiology.
A thorough medication history along with other possible exposures to toxic substances or cocaine should be obtained to exclude any drug or toxic aetiologies. These include anthracyclines (e.g., doxorubicin, daunorubicin, epirubicin, idarubicin), fluoropyrimidines (e.g., fluorouracil, capecitabine), immunotherapies (e.g., ipilimumab, tremelimumab, nivolumab, pembrolizumab, cemiplimab, atezolizumab, avelumab, durvalumab, and trastuzumab), arsenic, zidovudine, carbon monoxide, ethanol, iron, interleukin-2, cocaine, amphetamine, smallpox or mpox vaccine, SARS-CoV-2 (COVID-19) mRNA vaccine (may occur with other types of COVID-19 vaccines), catecholamines (e.g., adrenaline, noradrenaline, dopamine), cyclophosphamide, heavy metals (copper, iron, lead), radiation, antibiotics (penicillins, cephalosporins, sulfonamides), amphotericin B, thiazide diuretics, anticonvulsants (carbamazepine, phenytoin, phenobarbital), digoxin, lithium, amitriptyline, clozapine, snake venom, bee venom, black widow spider venom, scorpion venom, and wasp venom.
Physical examination
A thorough examination for both the cardiorespiratory findings and other general findings that may point to possible aetiology should be performed. Findings can include rales, elevated neck veins, S3 gallop, S3 and S4 summation gallop, pericardial friction rub, peripheral hypoperfusion, sinus tachycardia, atrial and ventricular arrhythmias, hypotension, altered sensorium, hepatomegaly, and lymphadenopathy. Resting tachycardia is an especially important sign in adolescents where the symptoms can be masked significantly in both acute and chronic myocarditis.
12-lead ECG
A 12-lead ECG should be ordered immediately on presentation in anyone with chest pain or cardiac symptoms.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
In myocarditis it most commonly displays non-specific ST-segment and T-wave abnormalities; however, ST-segment elevation and depression frequently occur. Children can present with atrial and ventricular arrhythmias and such a presentation can be a marker of poor outcomes.[61]Ichikawa R, Sumitomo N, Komori A, et al. The follow-up evaluation of electrocardiogram and arrhythmias in children with fulminant myocarditis. Circ J. 2011;75(4):932-8.
https://www.doi.org/10.1253/circj.cj-10-0918
http://www.ncbi.nlm.nih.gov/pubmed/21343655?tool=bestpractice.com
A component of pericarditis is common in children and can be evident as non-specific ST-segment changes in all of the precordial leads.
Laboratory evaluation
Cardiac biomarkers should be ordered immediately in any patient with suspected myocarditis. Creatine kinase and creatine kinase-MB levels are often mildly elevated. Troponin (I or T) levels have shown to be a more reliable indicator of myocardial damage, including in children.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
Serum B-type natriuretic peptide may be helpful in distinguishing primary cardiac from primary pulmonary aetiologies of dyspnoea when the physical examination and initial work-up is unclear or non-specific. In myocarditis it is elevated in response to ventricular distention such as occurs in congestive heart failure.[57]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
Two-dimensional echocardiogram
This should be ordered in every patient suspected of having myocarditis.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[56]Expert Panel on Cardiac Imaging, Rajiah P, Kirsch J, Bolen MA, et al. ACR Appropriateness Criteria® Nonischemic myocardial disease with clinical manifestations (ischemic cardiomyopathy already excluded). J Am Coll Radiol. 2021 May;18(5S):S83-105.
https://www.jacr.org/article/S1546-1440(21)00115-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33651982?tool=bestpractice.com
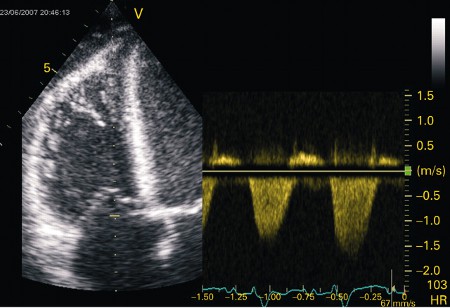
Myocarditis can cause global and regional left ventricular motion abnormalities, systolic and diastolic dysfunction, and dilatation.[Figure caption and citation for the preceding image starts]: Apical 4-chamber transthoracic echocardiogram in a patient with myocarditis. The right ventricle is dilated with hypokinesis. Triscupid regurgitation is present with a reduced continuous wave Doppler gradient indicating right ventricular failureFrom: Rasmussen TB, Dalager S, Andersen NH, et al. BMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0997 [Citation ends].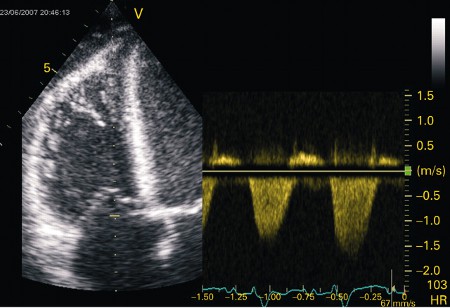 [Figure caption and citation for the preceding image starts]: Apical 4-chamber echocardiogram in a patient presenting with myocarditis showing a slightly dilated left ventricle with spontaneous ultrasonic contrast indicating severely impaired left ventricular systolic functionFrom: Rasmussen TB, Dalager S, Andersen NH, et al. BMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0997 [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber echocardiogram in a patient presenting with myocarditis showing a slightly dilated left ventricle with spontaneous ultrasonic contrast indicating severely impaired left ventricular systolic functionFrom: Rasmussen TB, Dalager S, Andersen NH, et al. BMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0997 [Citation ends].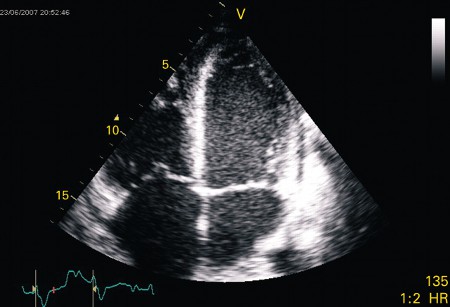 Special attention should be paid to evaluation for clots which can change therapies and risk profile. Development of intracardiac thrombosis can occur due to a prothrombotic, proinflammatory state as well as stagnant blood in the dysfunctional heart.[62]Skouri HN, Dec GW, Friedrich MG, et al. Noninvasive imaging in myocarditis. J Am Coll Cardiol. 2006 Nov 21;48(10):2085-93.
https://www.doi.org/10.1016/j.jacc.2006.08.017
http://www.ncbi.nlm.nih.gov/pubmed/17112998?tool=bestpractice.com
Special attention should be paid to evaluation for clots which can change therapies and risk profile. Development of intracardiac thrombosis can occur due to a prothrombotic, proinflammatory state as well as stagnant blood in the dysfunctional heart.[62]Skouri HN, Dec GW, Friedrich MG, et al. Noninvasive imaging in myocarditis. J Am Coll Cardiol. 2006 Nov 21;48(10):2085-93.
https://www.doi.org/10.1016/j.jacc.2006.08.017
http://www.ncbi.nlm.nih.gov/pubmed/17112998?tool=bestpractice.com
Endomyocardial biopsy (EMB)
The potential risks and benefits of EMB should always be carefully assessed, particularly during the acute presentation, as the risk of arrhythmia or ventricular perforation is highest at this time. There is no general consensus on which patients should undergo EMB; recommendations vary and local guidelines should be consulted.[5]Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology working group on myocardial and pericardial diseases. Eur Heart J. 2013 Sep;34(33):2636-48.
https://academic.oup.com/eurheartj/article/34/33/2636/408735
http://www.ncbi.nlm.nih.gov/pubmed/23824828?tool=bestpractice.com
[55]Bozkurt B, Colvin M, Cook J, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 2016 Nov 3;134(23):e579-646.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000455
http://www.ncbi.nlm.nih.gov/pubmed/27832612?tool=bestpractice.com
[57]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
[58]McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.
https://academic.oup.com/eurheartj/article/42/36/3599/6358045
http://www.ncbi.nlm.nih.gov/pubmed/34447992?tool=bestpractice.com
[59]Seferović PM, Tsutsui H, McNamara DM, et al. Heart Failure Association of the ESC, Heart Failure Society of America and Japanese Heart Failure Society position statement on endomyocardial biopsy. Eur J Heart Fail. 2021 Jun;23(6):854-71.
https://onlinelibrary.wiley.com/doi/10.1002/ejhf.2190
http://www.ncbi.nlm.nih.gov/pubmed/34010472?tool=bestpractice.com
[63]Cooper LT, Baughman KL, Feldman AM, et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Circulation. 2007 Nov 6;116(19):2216-33.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.107.186093
http://www.ncbi.nlm.nih.gov/pubmed/17959655?tool=bestpractice.com
[64]Ammirati E, Frigerio M, Adler ED, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail. 2020 Nov;13(11):e007405.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7673642
http://www.ncbi.nlm.nih.gov/pubmed/33176455?tool=bestpractice.com
A statement on dilated cardiomyopathies from the AHA recommends biopsy 'in those patients with clinically suspected unexplained acute myocarditis who require inotropic support or mechanical circulatory support and those with Mobitz type 2 second-degree or higher heart block, sustained or symptomatic ventricular tachycardia, or failure to respond to guideline-based medical management within 1-2 weeks'.[55]Bozkurt B, Colvin M, Cook J, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 2016 Nov 3;134(23):e579-646.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000455
http://www.ncbi.nlm.nih.gov/pubmed/27832612?tool=bestpractice.com
The 2022 AHA/American College of Cardiology/Heart Failure Society of America (HFSA) heart failure (HF) guidelines state 'Endomyocardial biopsy may be advantageous in patients with heart failure in which a histological diagnosis, such as myocarditis, may influence treatment decisions'.[57]Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001063
http://www.ncbi.nlm.nih.gov/pubmed/35363499?tool=bestpractice.com
A joint statement from Heart Failure Association of European Society of Cardiology (ESC), HFSA, and Japanese HF Society recommends EMB 'in patients with fulminant/acute myocarditis presenting with cardiogenic shock or acute HF and left ventricular (LV) dysfunction, with or without malignant ventricular arrhythmias and/or conduction abnormalities'. They also recommend considering EMB in 'haemodynamically stable patients with clinical symptoms and diagnostic criteria (electrocardiographic abnormalities, elevated troponin levels, and imaging findings) suggestive of myocarditis, in the absence of significant coronary artery disease'.[59]Seferović PM, Tsutsui H, McNamara DM, et al. Heart Failure Association of the ESC, Heart Failure Society of America and Japanese Heart Failure Society position statement on endomyocardial biopsy. Eur J Heart Fail. 2021 Jun;23(6):854-71.
https://onlinelibrary.wiley.com/doi/10.1002/ejhf.2190
http://www.ncbi.nlm.nih.gov/pubmed/34010472?tool=bestpractice.com
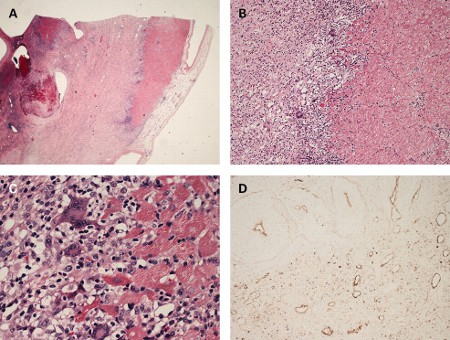
[Figure caption and citation for the preceding image starts]: Histological findings in a patient with giant cell myocarditis. A: severe myocardial necrosis and fibrotic replacement of the cardiomyocytes with granulation tissue and fibrosis is present in a section from the anterolateral left ventricular wall; B: a sharp demarcating border between vital and necrotic myocardium is seen, confirmed by additional immunohistochemical staining for myoglobin; C: at the inflammatory border, cells consisting of prominent multi-nucleated giant cells, macrophages, lymphocytes, and eosinophilic granulocytes are seen in close proximity to vital myocardium; D: immunohistochemical staining for complement 4d is positive in all vessels, suggestive of complement cascade activationFrom: Rasmussen TB, Dalager S, Andersen NH, et al. BMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0997 [Citation ends].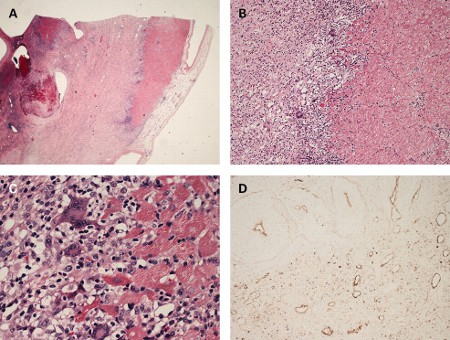
In children, AHA guidelines continue to mark biopsies as the reference test for myocarditis diagnosis.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
It is important to note that with immunohistochemistry, the ability to assess for inflammatory cells has greatly increased. Additionally, the biopsies can be used for viral polymerase chain reaction (PCR) testing to diagnose viral myocarditis with specificity, and to analyse immune-mediated injury and potentially inflammatory markers at a molecular level.[65]Bowles NE, Ni J, Kearney DL, et al. Detection of viruses in myocardial tissues by polymerase chain reaction. evidence of adenovirus as a common cause of myocarditis in children and adults. J Am Coll Cardiol. 2003 Aug 6;42(3):466-72.
https://www.doi.org/10.1016/s0735-1097(03)00648-x
http://www.ncbi.nlm.nih.gov/pubmed/12906974?tool=bestpractice.com
Cardiac MRI
Cardiac MRI is as an important tool in the assessment of suspected myocarditis, particularly when trying to distinguish acute myocarditis from acute MI.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[56]Expert Panel on Cardiac Imaging, Rajiah P, Kirsch J, Bolen MA, et al. ACR Appropriateness Criteria® Nonischemic myocardial disease with clinical manifestations (ischemic cardiomyopathy already excluded). J Am Coll Radiol. 2021 May;18(5S):S83-105.
https://www.jacr.org/article/S1546-1440(21)00115-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33651982?tool=bestpractice.com
[60]Friedrich MG, Strohm O, Schulz-Menger, et al. Contrast media-enhanced magnetic resonance imaging visualizes myocardial changes in the course of viral myocarditis. Circulation. 1998 May 12;97(18):1802-9.
https://www.ahajournals.org/doi/full/10.1161/01.cir.97.18.1802
http://www.ncbi.nlm.nih.gov/pubmed/9603535?tool=bestpractice.com
In some cases, findings from cardiac MRI can also be useful in determining the aetiology of myocarditis.[66]Mahrholdt H, Wagner A, Deluigi CC, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006 Oct 10;114(15):1581-90.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.105.606509
http://www.ncbi.nlm.nih.gov/pubmed/17015795?tool=bestpractice.com
Lake Louise consensus criteria were updated in 2018 to propose that presence of both T2 and T1 findings provide strong evidence for myocardial inflammation.[67]Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018 Dec 18;72(24):3158-76.
https://www.sciencedirect.com/science/article/pii/S0735109718388430
http://www.ncbi.nlm.nih.gov/pubmed/30545455?tool=bestpractice.com
In children, the primary purpose of cardiac MRI is to identify myocardial injury, and to differentiate acute myocarditis from non-inflammatory cardiomyopathies.[15]Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001001
http://www.ncbi.nlm.nih.gov/pubmed/34229446?tool=bestpractice.com
Other tests
Coronary angiography: this should be performed when the presenting symptoms and findings are indistinguishable from the acute coronary syndromes.
FDG PET-CT: helps diagnose myocarditis by providing metabolic information of inflammation as increased FDG uptake. The role of 18F-FDG PET-CT is useful in chronic myocarditis, where CMR does not have the same accuracy as in acute myocarditis.[68]Chen W, Jeudy J. Assessment of myocarditis: cardiac MR, PET/CT, or PET/MR? Curr Cardiol Rep. 2019 Jun 26;21(8):76.
http://www.ncbi.nlm.nih.gov/pubmed/31243587?tool=bestpractice.com
MRI-guided EMB: this is a promising new technology that seems to significantly increase the sensitivity of EMB in the diagnosis of myocarditis.[69]Mahrholdt H, Goedecke C, Wagner A, et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation. 2004 Mar 16;109(10):1250-8.
https://www.ahajournals.org/doi/10.1161/01.cir.0000118493.13323.81
http://www.ncbi.nlm.nih.gov/pubmed/14993139?tool=bestpractice.com
This is still in the developmental phase and requires validation in larger studies.
 [Figure caption and citation for the preceding image starts]: Apical 4-chamber echocardiogram in a patient presenting with myocarditis showing a slightly dilated left ventricle with spontaneous ultrasonic contrast indicating severely impaired left ventricular systolic functionFrom: Rasmussen TB, Dalager S, Andersen NH, et al. BMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0997 [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber echocardiogram in a patient presenting with myocarditis showing a slightly dilated left ventricle with spontaneous ultrasonic contrast indicating severely impaired left ventricular systolic functionFrom: Rasmussen TB, Dalager S, Andersen NH, et al. BMJ Case Reports 2009; doi:10.1136/bcr.09.2008.0997 [Citation ends].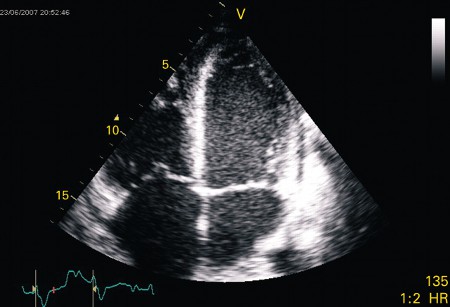 Special attention should be paid to evaluation for clots which can change therapies and risk profile. Development of intracardiac thrombosis can occur due to a prothrombotic, proinflammatory state as well as stagnant blood in the dysfunctional heart.[62]
Special attention should be paid to evaluation for clots which can change therapies and risk profile. Development of intracardiac thrombosis can occur due to a prothrombotic, proinflammatory state as well as stagnant blood in the dysfunctional heart.[62]