Aetiology
Pathology involving the tongue, floor of mouth, palate, tonsils, or other oral cavity structures can lead to oral phase dysphagia. The problem in this scenario is often recognised as difficulty with initiating the swallow.
Pharyngeal disorders can cause dysphagia when dysfunction of the base of tongue, pharynx, larynx, or cricopharyngeal muscle occurs. This may be manifest by reports of food sticking in the throat, symptoms of aspiration, hoarseness, cough, pain in the throat, or even referred pain to the ear.
Oesophageal dysphagia may be as a result of oesophageal motility disorders, intrinsic or extrinsic masses, webs, rings, reflux disease, or lower oesophageal sphincter disorders. These pathologies will more likely present with sensation of food sticking in the lower aspect of the neck or chest, regurgitation of food, chest pain, or heartburn.
Dysphagia is often multifactorial in nature. For example, an elderly patient may have weak pharyngeal musculature, with cervical osteophytes and oesophageal reflux. Each issue alone may not be problematic, but combined they may cause significant dysphagia.
Oropharyngeal infection/inflammation
Infections such as pharyngitis, oesophageal candidiasis, epiglottitis, and retropharyngeal abscess can cause dysphagia, as can radiation- and/or chemotherapy-induced oral mucositis.[9]
Oral cavity structural abnormalities
Hypertrophic tonsils
Causes dysphagia for solids by interfering with transfer of bolus from oral cavity to pharynx.
May be associated with obstructive sleep apnoea, recurrent infections, and snoring.
Lingual tonsils (at the base of the tongue) may be difficult to visualise but may also become hypertrophic and interfere with swallowing. Can be visualised with flexible nasopharyngoscopy or indirect laryngoscopy with a dental mirror.[Figure caption and citation for the preceding image starts]: Hypertrophic tonsils causing severely narrowed pharyngeal openingFrom the collection of Dr S. Charous [Citation ends].
 [Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Hypertrophic tonsilsFrom the collection of Dr S. Charous [Citation ends].
Oral cavity tumours (especially cancers)
Can affect any of the structures in the oral cavity and become large enough to cause obstruction and prevent food passage.
Can affect function of any of the structures by invasion into surrounding tissue: for example, carcinoma of the tongue with floor of mouth invasion that leads to impaired tongue mobility, resulting in difficulty swallowing.
More common in smokers and alcohol drinkers.
Becoming more common in non-smokers because of human papillomavirus-induced squamous cell carcinomas involving the tonsils and base of the tongue.
Often associated with pain, altered speech, neck mass, or bloody sputum.
Dentition
Edentulous patients or patients with poor dentition may have difficulty chewing food and may therefore be unable to form an appropriately sized food bolus to be transferred into the pharynx.
Oropharyngeal structural abnormalities
Zenker's diverticulum
Located proximal to upper oesophageal sphincter.
The incidence increases by age; more frequent in women.
Prevalence 50% in seventh and eighth decades.
Is associated with regurgitation of undigested food, intermittent solid food dysphagia, halitosis, and excessive salivation.
Barium swallow is the best diagnostic test.[Figure caption and citation for the preceding image starts]: Zenker’s diverticulum: lateral view with barium oesophagramFrom the collection of Dr S. Charous, Clinical Professor of Otolaryngology - Head and Neck Surgery, Loyola University Medical Center; used with permission. [Citation ends].
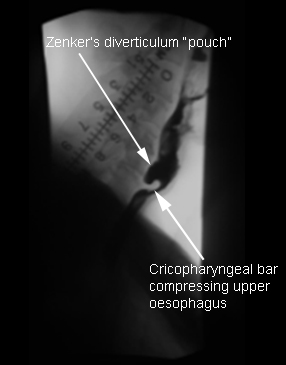
Can be missed or difficult to visualise on oesophageal endoscopy.[10]
Pharyngeal/laryngeal tumours
Symptoms may include progressive solid food dysphagia, weight loss, and otalgia (referred pain).
Hoarseness, symptoms of aspiration (especially of liquids), and shortness of breath are often associated with laryngeal tumours.
Vast majority of malignancies are squamous cell carcinomas, often very aggressive when this is the primary site with frequent metastases.
Endoscopy with biopsy is the best diagnostic test.[11][Figure caption and citation for the preceding image starts]: Laryngeal/pharyngeal squamous cell carcinomaFrom the collection of Dr S. Charous [Citation ends].

Stenosis
Mostly caused by prior radiation, surgery, or chemical ingestion.
May be idiopathic, but this is rare.
Presents as solid food dysphagia or symptoms of aspiration.
Flexible fibre-optic nasopharyngoscopy/laryngoscopy, oesophagogastroduodenoscopy (OGD), and barium swallow are helpful.
Extrinsic compression
Cervical lymphadenopathy, cricopharyngeal bar, cervical spine osteophytes, or thyromegaly.[Figure caption and citation for the preceding image starts]: Endoscopic view of pharynx showing osteophytes pressing inwards on posterior pharyngeal wall, obscuring view of larynx with epiglottis in backgroundFrom the collection of Dr S. Charous [Citation ends].
 [Figure caption and citation for the preceding image starts]: Lateral x-ray during barium swallow, demonstrating osteophytes displacing flow of barium in upper oesophagusFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Lateral x-ray during barium swallow, demonstrating osteophytes displacing flow of barium in upper oesophagusFrom the collection of Dr S. Charous [Citation ends]. [Figure caption and citation for the preceding image starts]: Thyroid tumour compressing cervical oesophagusFrom the collection of Dr S. Charous [Citation ends].
[Figure caption and citation for the preceding image starts]: Thyroid tumour compressing cervical oesophagusFrom the collection of Dr S. Charous [Citation ends].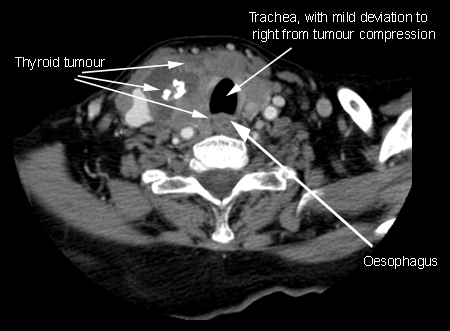
Flexible fibre-optic nasopharyngoscopy/laryngoscopy and barium swallow can usually identify the defect.
Oropharyngeal neuromuscular abnormalities
Neuromuscular discoordination, involving the central nervous system and or the peripheral nervous system, can result in oral or pharyngeal dysphagia.[12] Neurological examination and evaluation of neurological symptoms are helpful in directing the physician to the underlying aetiology of the dysfunction. The following are common neuromuscular causes of oral or pharyngeal dysphagia; stroke in this group is the most common cause:
Stroke: some 40% to 70% of people with stroke experience dysphagia[2]
Vocal cord paralysis
Amyotrophic lateral sclerosis
Multiple sclerosis
Brain and skull base tumours
Post-operative resections of skull base or brain tumours (especially and often involving cranial nerves IX, X, and XII)
Sjogren’s syndrome[15]
Myasthenia gravis
Inflammatory myopathies
Wilson's disease
Progressive supranuclear palsy
Oculopharyngeal muscular dystrophy
Muscle tension dysphagia, which describes excessive laryngeal and pharyngeal tension that disrupts swallowing; it is a diagnosis of exclusion made with speech therapists and cannot yet be diagnosed with conventional testing.[16]
Oesophageal structural abnormalities
Stricture
The main symptom is solid food dysphagia.
OGD or barium oesophagrams are the best diagnostic test.
Dysphagia is most prevalent when the luminal diameter is <15 mm (normal is 20 mm).[17]
Acid reflux accounts for 60% to 70% of cases of strictures and mainly occurs in the region of the lower oesophageal sphincter.[18]
Caustic agents and radiotherapy may lead to strictures.
Pills such as potassium chloride, doxycycline, quinidine, non-steroidal anti-inflammatory drugs, iron, and alendronic acid may cause strictures.[19]
Intramural lesions
Foreign body: acute dysphagia could occur as a result of foreign bodies and food impaction in the oesophagus. These most often will obstruct at the level of the upper or lower oesophageal sphincters.
Oesophageal/cardia carcinomas: patients typically present with reflux in early disease, and dysphagia and odynophagia in locally advanced or late disease.[20] Dysphagia alone or with unintentional weight loss is the most common presenting symptom.[21] Adenocarcinoma and squamous cell carcinoma account for over 95% of all cases of oesophageal cancer.[21] Squamous cell carcinoma is often associated with alcohol and tobacco consumption, and with human papillomavirus infection; adenocarcinoma with gastro-oesophageal reflux disease (GORD), Barrett’s oesophagus, high body mass index, and male sex.[20] Approximately 75% of all oesophageal adenocarcinomas are located in the distal oesophagus, whereas squamous cell carcinomas occur more frequently in the proximal-to-middle oesophagus.[22][23] OGD with biopsy is usually diagnostic.[24]
Benign tumours: rare; include leiomyoma, granular cell tumours, and papillomas.
Oesophageal metastases: metastasis to the oesophagus is rare, but most frequently occurs in the context of advanced lung or breast cancer. Other possible primary carcinomas include ovarian and colonic cancer.[25]
Extramural lesions compressing the oesophagus
Mediastinal masses
Bronchial carcinoma
Cervical osteoarthritis/cervical osteophytes[26]
Patients usually have symptoms of underlying disease with recently added solid food dysphagia
Best diagnosed with barium study.[11]
Oesophageal ring
Manifest by intermittent solid food dysphagia; if found presumed to be the cause of symptoms.
Mucosal ring (Schatzki ring): prevalence of 0.2% to 1.4%. Located at gastro-oesophageal junction.
Muscular rings: located 1.5 cm proximal to the gastro-oesophageal junction. Typically asymptomatic.[27]
Anatomical abnormalities
Oesophageal diverticulum: known as traction diverticulum secondary to pulling of the oesophageal wall. Located in the middle third of the oesophagus. Barium study is the most useful test to identify them.
Hiatus hernia: is typically asymptomatic, associated with GORD, and can cause bleeding and incarceration.
Webs: found in 5% to 15% of patients with benign causes of dysphagia who undergo OGD.[27]
Oesophageal motor abnormalities
Idiopathic achalasia
Oesophageal motility disease with insufficient lower oesophageal sphincter relaxation and loss of oesophageal peristalsis.
Progressive dysphagia to solids followed by liquids is seen in 82% to 100% of patients.
Oesophageal manometry is useful in detecting motility abnormalities of achalasia.[28][29][30][31]
Scleroderma
Causes oesophageal hypomotility and incompetence of lower oesophageal sphincter.
Can lead to chronic gastro-oesophageal reflux with subsequent stricture formation.
Oesophageal manometry along with clinical correlation is helpful in diagnosis.[32]
Diffuse oesophageal spasm
Mostly manifest by recurrent chest pains associated with meals.
More common with ingestion of very hot or very cold foods.
Is diagnosed by manometry, which reveals simultaneous contractions.[29][30][31][33]
Finding on barium swallow study is 'corkscrew' oesophageal body from a simultaneous contraction.[29][Figure caption and citation for the preceding image starts]: Corkscrew oesophagus from diffuse oesophageal spasm seen on a barium swallow studyFrom the collection of Dr S. Charous [Citation ends].

Hypocontracting oesophagus
Ineffective oesophageal motility with low amplitude, poorly co-ordinated peristalsis.
Hypotensive lower oesophageal sphincter.
Gastro-oesophageal reflux is significant and can lead to strictures.
Dysphagia is usually mild.
Nutcracker oesophagus
Is associated with chest pain.
Normal peristalsis with increased distal oesophageal mean amplitudes and hypertensive lower oesophageal sphincter.
Eosinophilic oesophagitis
Chronic immune-mediated condition often associated with concurrent allergic diseases including food allergies, allergic rhinitis, atopic dermatitis, or asthma.[35][36]
Three times more common in men than in women.[36][37][38] Eosinophilic oesophagitis appears to be more common in white people than in African-Americans or Asian people.[39][40] The peak incidence is seen in young adults and in the third and fourth decades of life.[36][37]
Patients may present with dysphagia, heartburn, chest pain, acute food impaction, and/or associated other symptoms consistent with gastro-oesophageal reflux.[35]
OGD shows multiple oesophageal rings with narrowing and decreased distensibility of oesophageal lumen from submucosal fibrosis and remodelling.[35]
Diagnosis is confirmed with biopsy of the oesophageal mucosa during endoscopy.[36][41][42][43][44] In the US, at least 2-4 biopsies are taken; at least 6 biopsies are recommended in Europe.[36][43][44]
Use of this content is subject to our disclaimer