Investigations
1st investigations to order
MRI - brain
Test
Should be performed on high field magnet (3 T is preferred, but 1.5 T is acceptable), with intravenous gandolinium-based contrast.[Figure caption and citation for the preceding image starts]: Representative axial magnetic resonance images using fluid-attenuated inversion recovery (FLAIR) showing typical lesions seen in MS in the periventricular regions. Comparable slices using the contrast agent gadolinium illustrate blood-brain barrier breakdown/active inflammation in 2 of the lesions. The FLAIR lesions that do not enhance are likely to be older, with a combination of gliosis and low-level chronic inflammation and degenerationFrom the collection of Dr Lael A. Stone [Citation ends].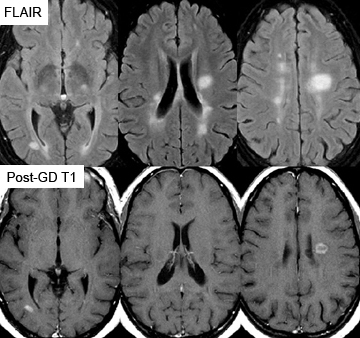
Sagittal three-dimensional (3D) fluid-attenuated inversion recovery (FLAIR) with multiplanar reconstruction acquisition is recommended. Axial T2-weighted FLAIR should be obtained if this sequence is not available.[3]
Almost all patients with MS will have abnormal cranial MRI, but the interpretation of the MRI may be difficult. Images must be interpreted by specialists who are very familiar with typical MS findings on MRI.
Sagittal fluid-attenuated inversion recovery (FLAIR) images can help distinguish between MS lesions and non-specific white matter changes, such as seen in association with hypertension, diabetes, age >50, smoking, migraine, high cholesterol, and toxin exposures.[Figure caption and citation for the preceding image starts]: Sagittal fluid-attenuated inversion recovery (FLAIR) images with typical MS lesions involve the corpus callosum either as discrete lesions or as finger-like projections perpendicular to the corpus callosum. Note also the enlargement of the ventricles and diffuse atrophy of more advanced MSFrom the collection of Dr Lael A. Stone [Citation ends].
MRI is also used for assessment of disease activity and monitoring of treatment effectiveness.[3]
Result
hyperintensities in the periventricular white matter; most sensitive images are sagittal FLAIR
MRI - spinal cord
Test
MRI of the spinal cord is recommended for all patients. Many patients with MS will have cervical spinal cord lesions and the specificity of this finding is very high.[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging scan of the cervical spine at high (≥1 Tesla) magnetic field strength illustrating a lesion that may cause myelopathic symptoms of bowel and bladder dysfunction as well as spastic paraparesisFrom the collection of Dr Lael A. Stone [Citation ends].
The cervical and thoracolumbar spinal cord, including conus, should be imaged. A 1.5 T or 3 T scanner can be used. The use of sagittal gadolinium-enhanced sequences is recommended.[3] MRI is also used for assessment of disease activity and monitoring of treatment effectiveness.[3]
Result
demyelinating lesions in the spinal cord, particularly the cervical spinal cord; detection of alternate diagnosis, such as cervical spondylosis
FBC
Test
Indicated to exclude alternative diagnoses or concomitant illnesses.
Result
should be normal
comprehensive metabolic panel
Test
Indicated to exclude alternative diagnoses or concomitant illnesses.
Result
should be normal
thyroid-stimulating hormone
Test
Indicated to exclude alternative diagnoses or concomitant illnesses.
Result
should be normal
vitamin B12
Test
Indicated to exclude alternative diagnoses or concomitant illnesses.
Result
should be normal
Investigations to consider
antibody testing for neuromyelitis optica spectrum disorders (NMOSD)
Test
Testing for antibodies characteristic of NMOSD (anti-aquaporin 4 [AQP4] and anti-myelin oligodendrocyte glycoprotein [MOG] antibodies) is recommended in patients with long segments of spinal cord demyelination with or without optic neuritis, and in patients with recurrent optic neuritis with normal brain imaging.[7][8]
Cell-based assays are more specific than enzyme-linked immunosorbent assay (ELISA) and should be used if available.
Result
positive in NMOSD
cerebrospinal fluid evaluation
Test
Due to the invasive nature of the testing, all other non-invasive tests should be pursued first.[4]
Note that the cerebrospinal fluid (CSF) is normal in 10% to 20% of MS cases.
How to perform a diagnostic lumbar puncture in adults. Includes a discussion of patient positioning, choice of needle, and measurement of opening and closing pressure.
Result
glucose and protein should be normal; cell count may be slightly elevated but never above 50/microlitre; oligoclonal bands and elevated CSF IgG and IgG synthesis rates are present in 80% of MS cases
evoked potentials
Test
Performed in patients for whom MRI is contraindicated.
Visual evoked potentials are most commonly abnormal, with somatosensory and auditory evoked potentials less so.
Somatosensory evoked potentials can be painful for the patient, as well as technically difficult.
These studies are useful to assist in establishing the diagnosis but they are not helpful for monitoring response to treatment.
Result
prolongation of conduction, particularly asymmetrical prolongation in the visual evoked potentials
Use of this content is subject to our disclaimer
