Complications
Once a dental abscess extends beyond the bone into the surrounding soft tissue, diffuse inflammation (cellulitis) develops. As the body’s defences are mobilised to combat an oral/facial infection, the cellulitis progresses into a brawny infiltrative stage. In this stage, suppuration (pus) is often present but is not localised to a specific area. A space-related abscess develops when the infection with suppuration becomes localised. Once the infection is in the soft tissue, it can spread by direct extension through the mucosa, skin, or muscle, or dissect along anatomical fascial planes or layers.[20]
Clinically, there is associated pain, erythema, oedema, fever, and malaise.[20]
Primary infections of the maxillary sinus are typically not of dental origin; however, owing to the proximity of the maxillary posterior teeth to the antral floor, there can be direct spread of a maxillary posterior periapical abscess through the antral floor leading to a secondary infection of the maxillary sinus mucosa.
Typical presenting symptoms include discharge and pain, and on clinical examination there will often be percussion sensitivity and decreased transillumination.
Treatment involves symptomatic relief and the use of antibiotic therapy.
In some cases, oral-antral communication is a complication of tooth extraction and requires secondary repair.
A major consideration for all odontogenic infections is the potential for airway obstruction due to extension of the infection into the fascial spaces surrounding the oropharynx.
Dysphagia, drooling, stridor, and dysphonia suggests involvement of deeper structures in the hypopharynx and the potential for impending airway obstruction.[20]
Planning and execution of successful airway management requires a team approach involving the anaesthetist, surgeon, and surgical team members.[47] In some cases, needle decompression of the abscess prior to attempted intubation or tracheotomy may be beneficial. In cases where there is a concern for potential airway compromise, a contingency plan for an urgent surgical airway should be in place if intubation attempts are not successful.
A potentially life-threatening, diffuse cellulitis involving the submental space, as well as the bilateral sublingual and submandibular spaces. Dental infections from a lower molar account for 80% of cases. The mortality rate is 5%.[20][46][59]
Progresses rapidly without respect to anatomical barriers and may lead to airway obstruction, which necessitates an urgent tracheotomy.
Symptoms include fever, malaise, dysphagia, pain with swallowing, difficulty breathing, and trismus.
Early operative intervention and airway control with intubation or tracheotomy are critical.
An abscess located in the tissues in the back of the throat behind the posterior pharyngeal wall.
Can occur due to extension of an odontogenic infection. Caused by a bacterial infection starting in the nasopharynx, sinuses, middle ear, tonsils, or adenoids.
Most commonly seen in infants and young children.
Difficult to diagnose due to its occurrence in the deep tissue. Presenting symptoms may include fever, malaise, neck pain and stiffness, stridor, cough, and drooling.
Can lead to airway obstruction, sepsis, or communication of the infection into the mediastinum.[20][59]
Can occur due to direct extension of an odontogenic infection; however, more commonly originates from the adjacent sinuses with the frontal sinus being the most frequent source in adults.[59]
Considered a very serious infection, as it can spread via direct extension or through retrograde venous blood flow via the angular or ophthalmic veins to the cavernous sinus.
Patients typically present with fever, pain, exophthalmos, and severe eyelid/periorbital oedema, often to the point where the eye is completely swollen shut.
Recommended treatment is surgery and appropriate antibiotic therapy.
Can lead to blindness or cavernous sinus thrombosis without appropriate treatment.
A rare, potentially fatal, progressive, dissecting soft tissue infection that spreads rapidly in the subcutaneous tissue forming large necrotic lesions. It is more common in the limbs or abdominal wall than the head and neck.[44][59][60] One review identified 125 cases in patients with dental infections.[61]
More frequent in immunocompromised patients or patients with diabetes.
Affected skin can be painful or paraesthetic, with a mottled blue-to-purple appearance and poorly defined erythematous margins.
Requires aggressive treatment with debridement and intravenous antibiotic therapy, with or without hyperbaric oxygen.
Serious, life-threatening complication of odontogenic infection involving the parapharyngeal or retropharyngeal space that spreads inferiorly via the fascial planes of the neck or the carotid sheath to involve the mediastinum and/or pericardium.
Diagnostic signs, seen later in the course of the infection, include pain, stiff neck with neck swelling under the sternocleidomastoid muscle and crepitation, dysphagia, dyspnoea, and possible airway obstruction.
Difficult to diagnose early and, therefore, has a very high mortality rate (42.8%).[64][65][66]
Localised suppurative infection in the cerebral parenchyma primarily in the temporal lobe or cerebellum. Can be the result of septic metastasis or cavernous sinus thrombophlebitis.
Although rare, it has been reported after dental infections, extractions, periodontal surgery, and dental prophylaxis.
Increased incidence in immunosuppressed patients (e.g., HIV infection/AIDS, transplant recipients).
May present with fever, severe headaches, projectile vomiting, and seizures. Other signs depend on the location of the infection in the brain.
Treatment involves surgical drainage, intravenous antibiotics, anticonvulsants, and corticosteroids.
Twenty-five percent of all brain abscesses occur in children between 4 and 7 years, most often presenting with multiple abscesses. This age group might be particularly susceptible because the first phase of teeth exfoliation takes place during this period.[67]
Extremely rare but serious complication where a thrombosis develops in the cavernous sinus of the brain. May be related to odontogenic infection in the midface, periorbital, or infratemporal regions. It has been estimated that 7% of cases of cavernous sinus thrombosis are caused by odontogenic infection.[20][59][69]
May present with fever, eye pain and sensitivity to pressure, papillary dilation, proptosis, ophthalmoplaegia, ptosis, abducens nerve paralysis, papilloedema, and signs of central nervous system irritation.
Requires early recognition and treatment with intravenous antibiotics and anticoagulants.
Although rare, it is the most common neurological complication of an odontogenic infection. Can be the result of septic metastasis or cavernous sinus thrombophlebitis.
Typically presents with fever, chills, severe headache, vomiting, and a stiff neck. On clinical examination, the patient may have a positive Kernig's and/or Brudzinski's sign.[59]
Treatment involves empirical intravenous antibiotic therapy and appropriate supportive care.
Unusual complication, with few cases of odontogenic infection-associated ARDS reported in the literature.[66][71][72]
Most commonly caused by sepsis/septic shock.
Early recognition and aggressive management is key, otherwise pulmonary fibrosis can develop.
Diagnosis is based on a high index of suspicion with the sudden onset of respiratory distress along with chest x-ray and ABG findings.
Treatment includes management of underlying sepsis or other aetiology, along with ventilator support with positive end-expiratory pressure to improve ventilation and maintain acceptable ABG levels.
Odontogenic infections, as well as various dental procedures, can lead to odontogenic sepsis. Pulmonary infections due to odontogenic sepsis have been described; however, whether this is truly due to sepsis or secondary to bacterial translocation via direct anatomical routes remains controversial.[63]
Aggressive odontogenic infections can potentially be life-threatening, particularly in developing countries.
Death is most commonly due to airway obstruction with a retropharyngeal or parapharyngeal abscess, or other complications such as pyothorax, mediastinitis, cavernous sinus thrombosis, or haemorrhage.
The primary principle of management of odontogenic infections is elimination of the source of the infection, which is the tooth.
When effective root canal treatment can’t be completed, or with periodontally hopeless teeth or a partially impacted wisdom tooth, extraction is the definitive treatment, along with surgical incision and drainage as indicated.
In some cases, removal of the tooth alone establishes adequate drainage without an associated incision and drainage.
Minor scarring may be associated with direct excision of fistula tracts, if present, after successful treatment of the abscess.
Can also occur with extra-oral surgical incision and drainage.
Some patients may request scar revision at a later date.
Acute or chronic inflammation of the bone that develops from the invasion of organisms from a periapical abscess. Occurs most frequently in the mandible and only rarely in the maxilla. Can involve the periosteum, cortical, or cancellous bone or marrow.[20][43][44]
More frequent in immunocompromised patients.
Osteoradionecrosis is a form of osteomyelitis that involves previously irradiated bone. Medication-related osteonecrosis of the jaw is also a form related to bisphosphonates and denosumab.[21]
Typically presents with pain, fever, sinus tract formation, exposed bone with sequestrum, and paraesthesia.
Treatment involves antibiotic therapy and debridement if necessary.
Odontogenic infections, as well as various dental procedures, can lead to an odontogenic sepsis. Most often caused by bacteria that normally reside in the mouth and throat. Bacteria originating from the mouth account for between 35% and 45% of infective endocarditis cases.[62]
Can be very difficult to diagnose, as many of the symptoms are non-specific (e.g., fever, fatigue, weight loss, cough, chest pain, or a new or altered heart murmur).[63]
Develops most commonly adjacent to the involved tooth as an intra-oral draining tract; however, in some cases, it may develop an extra-oral cutaneous sinus tract on the cheek or chin.[Figure caption and citation for the preceding image starts]: Panoramic radiograph with gutta percha tracking of intra-oral fistula; shows large periapical radiolucency related to failed root canal treatment (note the multiple root canal-treated teeth)From the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].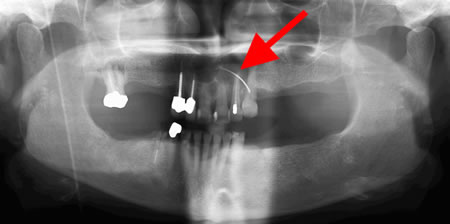 [Figure caption and citation for the preceding image starts]: Extra-oral sinus tract in the right anterior neck related to retained necrotic mandibular first molarFrom the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].
[Figure caption and citation for the preceding image starts]: Extra-oral sinus tract in the right anterior neck related to retained necrotic mandibular first molarFrom the personal collection of Melanie S. Lang and Thomas B. Dodson [Citation ends].
Due to epithelisation of the fistulous tract, some patients may require direct excision of the fistula once the abscess/infection has been successfully treated.
Site of involvement depends on the site of infection, and the type of operative intervention.
Sensory changes are the most common presentation, and are related to the trigeminal nerve. Facial nerve-related motor deficit may be seen, albeit more rarely. Paraesthesia may be seen as an initial presenting sign secondary to associated pressure/compression with oedema.
May be seen following operative intervention due to surgical manipulation related to incision and drainage.
Use of this content is subject to our disclaimer