Aetiology
Campylobacters are small, gram-negative rods that are curved in a spiral shape. The genus Campylobacter contains many species, 17 of which are pathogenic to humans.[2] Campylobacteriosis affects both humans and animals with spread occurring between species. Campylobacters are found in the gastrointestinal tract of a wide variety of wild and domestic animals, including poultry, swine, cattle, dogs, cats, and birds. Transmission to humans can occur by the consumption of contaminated food or drink (e.g., undercooked poultry or unpasteurised milk) or by contact with the faecal flora of an infected animal or human.[15][16]
Campylobacter jejuni is the primary cause of intestinal infection, causing 80% to 90% of all cases of recognised illness due to campylobacters. Most extra-intestinal infections are caused by Campylobacter fetus.[17][Figure caption and citation for the preceding image starts]: Microscopic image of Campylobacter demonstrating curved shaped rods; 48-hour culture of Campylobacter jejuniDr Robert Weaver, Image Library, US Centers for Disease Control and Prevention [Citation ends].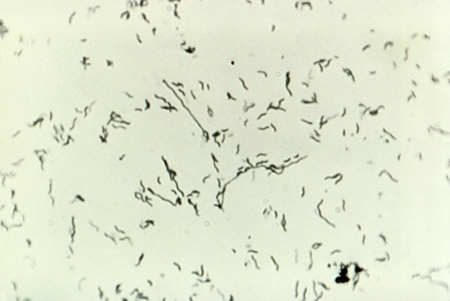
Pathophysiology
Campylobacteriosis is mostly a zoonotic infection, transmitted to humans from animals or animal products.[6] Contaminated water is also a source of infection.[18] Person-to-person transmission is extremely rare. Exposure to fewer than 500 organisms can cause disease.[14]
Campylobacter jejuni has been shown to have extensive phenotype diversity resulting in great adaptability; this has made identifying the precise mechanism of pathogenesis difficult.[19] In general, there are thought to be four main stages: adhesion to intestinal cells, colonisation, target cell invasion, and toxin production.[20] Host factors may also be important.[21]
The diarrhoeal stage is characterised by abdominal cramping and profuse diarrhoea. Bloody diarrhoea is common, occurring in 20% to 25% of cases. The sites of tissue injury include the jejunum, ileum, and colon. Biopsies of these sites will show an acute non-specific inflammatory reaction, with neutrophils, monocytes, and eosinophils present.[2][4]
Campylobacter organisms may be excreted in the faeces for several weeks after clinical recovery.[22]
In immunocompromised people, a variety of extra-intestinal manifestations have been reported, including: perinatal infection, bacteraemia, meningitis, spontaneous peritonitis, cholecystitis, endocarditis, pancreatitis, cystitis, cellulitis, hepatitis, interstitial nephritis, placental infection, septic abortion, septic arthritis, septic thrombophlebitis, pneumonia, lung abscess, and empyema.[5]
Use of this content is subject to our disclaimer