Approach
Fractures of the orbit may be seen in different scenarios of direct and indirect trauma to the globe, and the orbital, facial, or cranial bones. The most common presentations of orbital fractures are associated with zygomatic complex fractures, and orbital 'blow-out' fractures of the floor/medial wall.[1] Peri-orbital and orbital blow-out fractures are more often complicated by ocular injuries compared with other facial fracture patterns.[22]
Blow-out fractures can be classified into:
Pure: fracture of the medial wall and orbital floor causes passing of the orbital soft tissues through the hole created, causing the globe level to drop (hypoglobus) and sink back (enophthalmos).
Impure: a direct blow to the inferior orbital rim causes a buckling of the orbital margin, and results in a blow-out pattern of fracture with a concomitant rim fracture.
Advanced trauma life support (ATLS) is the initial approach in the management of any patient who may have orbital fractures and accompanying systemic injuries. Once the patient has been stabilised, a careful assessment of the orbit injury should be performed.
Orbital bone anatomy
The orbit is formed by 7 facial bones:
Zygomatic
Greater wing of sphenoid
Maxillary
Frontal
Lacrimal
Perpendicular plate of palatine
Ethmoid.
[Figure caption and citation for the preceding image starts]: Orbital bone anatomyFrom Whitaker RH, Borley NR. Instant Anatomy. 3rd ed. Oxford, UK: Blackwell; 2005; used with permission [Citation ends].
History
Patients present with a history of facial trauma. The patient should therefore be questioned about:
The mechanism of injury.
When the injury occurred.
Location of the accident.
The force involved.
The presence of oculovagal symptoms. The oculovagal reflex refers to the presence of vagal stimulation by pressure to intraorbital structures, which results in bradycardia, hypotension, nausea, and/or vomiting. Children are more sensitive.[11]
Whether vision changes have been perceived (blurred, double, or decreased vision).
If abuse is suspected, patients should be referred to appropriately trained and experienced personnel for assessment.
Physical examination
A full examination of the cranial and maxillofacial skeleton and soft tissues, and of the eye itself, should be performed. This includes:
Examination of the facial bones for deformity.
Examination of the eyelids and surrounding soft tissue. Findings may include:
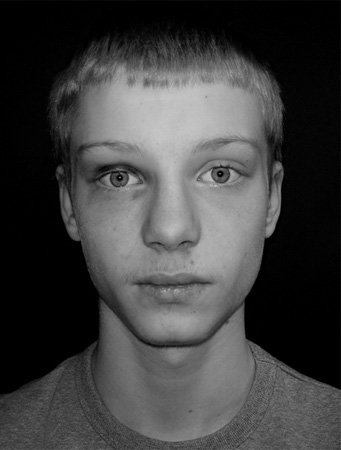
Peri-orbital ecchymosis ('panda eye')[Figure caption and citation for the preceding image starts]: Paediatric blow-out fracture: patient looking in central gaze. Mild right circumorbital ecchymosis is notedFrom Cobb A, et al. Emerg Med J. 2009;26:351-353; used with permission [Citation ends].
Peri-orbital oedema
Infra-orbital nerve sensory loss to upper lip and face
Step defect infra-orbital rim.
Inspection of the globe for perforation or other direct injury of the globe. Conjunctival excoriation is uncommon. More severe injuries are less common. Any positive findings warrant ophthalmology referral. Findings may include:
Subconjunctival haemorrhage
Derangement of globe position:
Proptosis or exophthalmos: anterior displacement of the eye in the orbit
Hypoglobus: downward displacement of the eye in the orbit
Enophthalmos: posterior displacement of the eye in the orbit.
Assessment of visual acuity (Snellen chart). Findings may include:
Visual acuity loss
Visual disturbance.
Diplopia test in 9 fields of gaze. This test is performed by asking the patient to look up, then to the left and right, look straight ahead, then to the left and right, then down, then to the left and right; note any double vision. Findings may include:
Diplopia on upward gaze: this is a pathognomonic sign of a blow-out fracture
Upgaze limitation on affected side
Pain on upward gaze
In entrapment of one globe, overswing of other eye on upward gaze may be noted, as compensatory overstimulation of both levators exists. [Figure caption and citation for the preceding image starts]: Paediatric blow-out fracture: patient looking in upward gaze. Right globe limitation by inferior soft tissue entrapment is notedFrom Cobb A, et al. Emerg Med J. 2009;26:351-353; used with permission [Citation ends].

Assessment of pupil responses, size, and shape.
Assessment of colour vision. Findings may include colour vision loss (red lost first).
Assessment of cranial nerves. Findings may include impaired pupillary light reflex (direct or consensual).
Assessment of medial canthal ligaments. Findings may include intercanthal distance increased (average intercanthal distance = 32 mm).
The classic presentation of orbital fractures in children is the absence of subconjunctival haemorrhage, with upgaze diplopia and general malaise.[11]
Imaging
Following history and physical examination, the following imaging studies may be performed:
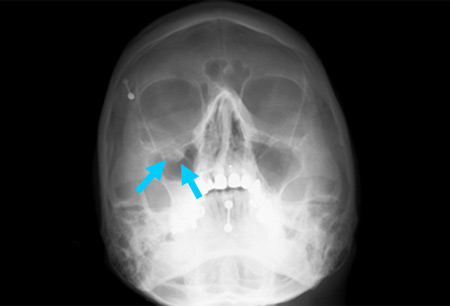
Injuries involving the mid-facial bones: occipitomental and antero-posterior film facial views are indicated. An occipitomental x-ray is only useful for impure fractures (i.e., those involving the orbital floor and infra-orbital rim). The presence of a polypoid mass (teardrop sign) protruding from the floor of the orbit into the maxillary antrum is a classic radiographic finding in blow-out fractures. The teardrop represents the herniated orbital contents, peri-orbital fat, and inferior rectus muscle. [Figure caption and citation for the preceding image starts]: Right orbital blow-out fracture; teardrop sign on occipitomental 15° x-rayFrom the personal collection of Dr Alistair Cobb [Citation ends].
In patients with significant injuries or children with entrapment: there might be suspicion of retrobulbar haemorrhage or gross facial injury; therefore, a computed tomography (CT) scan should be considered. However, in such cases, reasonably urgent review by the maxillofacial team is warranted. Magnetic resonance imaging (MRI) has been demonstrated to be equally accurate in demonstrating or excluding orbital wall fractures. It can be used when available.
Assessment of soft tissue: soft tissue herniation and entrapment may be demonstrated more clearly by MRI than by CT scanning. However, MRI may underestimate the incidence of soft tissue injuries.[23] There may be a role for rapid ultrasonographic scanning for immediate assessment of orbital fractures in the accident and emergency department.
Other tests
Forced duction test: this test is performed by an ophthalmology/maxillofacial specialist in comatose patients to determine whether the absence of movement of the eye is due to a neurological disorder or a mechanical restriction. A fine pair of ophthalmic forceps is used to gently grasp the inferior-most conjunctiva and used to attempt to elevate the eye. If there is mechanical restriction the eye will not move.
Orthoptic testing: this test includes Hess chart, cover test, binocular fixation test, and binocular fields of vision. All cases of orbital injury, real or suspected, should undergo orthoptic assessment. All patients should be referred to an orthoptist.
Use of this content is subject to our disclaimer