Differentials
Common
Cervical cancer
History
history of abnormal cervical cytology (Pap smear or liquid-based cytology); contact bleeding (bleeding related to intercourse and bimanual examination); pelvic pain; possible history of multiple sexual partners, early-onset sexual activity (<18 years), cigarette smoking, immunosuppression, lower socioeconomic status, and oral contraceptive use
Exam
cervical mass or cervical bleeding on vaginal/speculum examination
1st investigation
- colposcopy:
abnormal cervical lesions and/or cervical bleeding
More
Other investigations
- cervical biopsy:
malignant cells
More
Miscarriage
History
previous missed period; vaginal bleeding with or without clots; may be associated pelvic pain or recent postcoital bleeding
Exam
vaginal speculum examination may reveal products of conception in the upper vagina or protruding through the cervical os.
1st investigation
Other investigations
- FBC:
normal or anaemia
- rhesus blood group:
identifies maternal Rh-negative blood group, if present
More
Cervical polyp
History
contact bleeding (e.g., postcoital bleeding, postvaginal examination bleeding), patient usually aged over 40 years
Exam
speculum examination may reveal the cervical polyp
1st investigation
- none:
clinical diagnosis
More
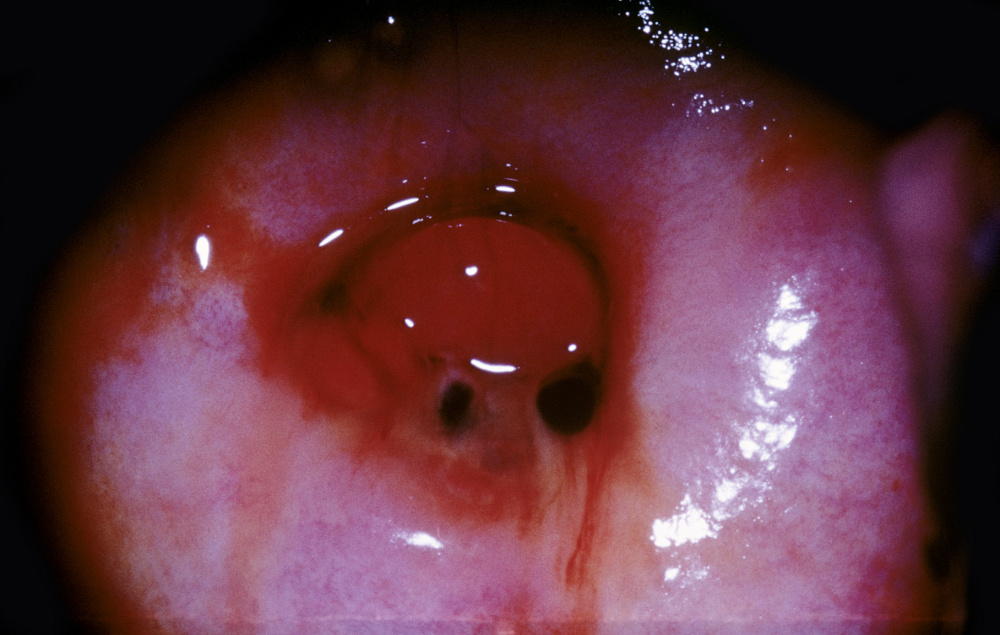
Ectropion
History
usually a history of contact bleeding (e.g., postcoital bleeding)
Exam
speculum examination of cervix reveals red rather than pink outer cervix due to shift of transformation zone
1st investigation
- colposcopy:
visualisation of suspicious area
More
Other investigations
Iatrogenic
History
use of hormonal contraception or hormone replacement therapy; missed, delayed, or erratic pill taking; erratic painless bleeding
Exam
normal examination
1st investigation
- none:
clinical diagnosis
Other investigations
- cervical cytology:
normal
More
Uncommon
Endometrial cancer
History
usually >50 years, intermenstrual bleeding, obesity, nulliparity, history of polycystic ovarian syndrome, late menopause, unopposed oestrogen use, tamoxifen use, smoking, history or family history of hereditary non-polyposis colon cancer
Exam
uterine enlargement and irregularity on bimanual examination
1st investigation
- transvaginal ultrasound:
focally thickened endometrium
More
Other investigations
- endometrial biopsy:
endometrial adenocarcinoma present
More
Ovarian cancer
History
family history of ovarian or breast cancer, known BRCA1 or BRCA2 mutation; non-specific GI symptoms might be more prominent than gynaecological symptoms (e.g., bloating, nausea, dyspepsia, diarrhoea, constipation); urinary urgency is common
Exam
pelvic mass; adnexal or rectovaginal mass on pelvic examination
1st investigation
- transvaginal ultrasound:
presence of solid, complex, septated, multiloculated mass; high blood flow
Vaginal cancer
History
history of contact bleeding (e.g., postcoital bleeding)
Exam
speculum examination may reveal vaginal tumour and suspicious areas that bleed on touch
1st investigation
- colposcopy:
abnormal vasculature, acetowhite epithelium
Other investigations
- vaginal biopsy:
malignant cells
More
Ectopic pregnancy
History
previous missed period, pelvic pain, previous history of ectopic pregnancy or pelvic infections, prior tubal surgery or use of assisted reproductive technologies
Exam
tenderness on lower abdominal palpation; pain and palpable mass on bimanual examination; cervical motion tenderness; rarely palpable adnexal mass; warning signs of possible rupture including hypotension, tachycardia, involuntary abdominal guarding, referred shoulder pain
1st investigation
- ultrasound (abdominal and transvaginal):
no intrauterine pregnancy; gestational sac in extra-uterine location; fluid sometimes present in pouch of Douglas
- serum or urine hCG:
positive
Other investigations
- FBC:
normal or anaemia
Placental abruption
History
vaginal bleeding, abdominal pain, and uterine contractions; usually occurs in second or third trimester; history of mother smoking or using cocaine, trauma (e.g., been involved in a motor vehicle accident or victim of domestic violence), hypertension, prior placental abruption
Exam
tender hard uterus, uterine contractions; hypotension and tachycardia in larger haemorrhages
1st investigation
- fetal monitoring:
abnormalities in the tracing that suggest an abruption: late decelerations, loss of variability, variable decelerations, a sinusoidal fetal heart rate tracing, and fetal bradycardia, defined as a persistent fetal heart rate below 110 beats per minute
More - FBC:
normal or anaemia or thrombocytopenia
More - type and crossmatch:
preparation for transfusion/surgery
More - ultrasound:
retroplacental haematoma (hyperechoic, isoechoic, hypoechoic); preplacental haematoma (jam-like appearance with a shimmering effect of the chorionic plate with fetal movement); increased placental thickness and echogenicity; sub-chorionic collection or marginal collection
More
Other investigations
- coagulation studies (PT, PTT, fibrinogen, fibrinogen breakdown products):
abnormal
More
Placenta praevia
History
painless vaginal bleeding, usually presents in the second or third trimester; history of previous caesarean section, previous abnormal placentation, high parity, in vitro fertilisation, advanced maternal age
Exam
absence of cervical/vaginal causes of bleeding on speculum examination; non-tender uterus; low BP; tachycardia
1st investigation
Cervicitis
History
multiple sexual partners, history of sexually transmitted infection, bacterial vaginosis, unprotected intercourse, intermenstrual/postcoital bleeding, dyspareunia, dysuria
Exam
purulent vaginal or cervical discharge; friable and tender cervix on digital examination or swab use; vulval or vaginal inflammation; strawberry cervix
1st investigation
- nucleic acid amplification test (NAAT):
positive for Chlamydia trachomatisor Neisseria gonorrhoeae
More - wet-mount examination of cervical discharge:
>10 WBCs per high-power field of vaginal fluid (leucorrhoea)
More - rapid tests (OSOM Trichomonas, Affirm VP III):
positive for Trichomonas vaginalis
More - Gram stain of cervical discharge:
Lactobacillus morphotype reduced or absent
More
Vaginitis
History
presence of intrauterine device; use of oral contraceptive pill; douching; sexual activity; poor or excessive hygiene; prior antibiotic use; HIV infection and diabetes; vaginal discharge, dysuria, dyspareunia, intermenstrual/postcoital bleeding; pruritus
Exam
discharge adherent to vaginal mucosa; erythema, or pale and shiny epithelium, decreased elasticity, friable epithelium (atrophic vaginitis); vulvar erythema or oedema can accompany candidal vaginitis
1st investigation
Sexual abuse in children
History
a high index of suspicion is required; symptoms, often non-specific, can include frequent or persistent genitourinary complaints, chronic somatic complaints (e.g., headache or recurrent abdominal pain), depression, sexualised behaviour, aggression, regression, or sleep disturbance
Exam
often normal; may be straddle injury, vaginal discharge, anogenital lesions, hymen abnormalities, anal fissures, or tags
1st investigation
- none:
diagnosis is clinical
More
Other investigations
Neonatal uterine bleeding
History
female neonate on day 3 to 5 of life
Exam
normal
1st investigation
- none:
clinical diagnosis
Other investigations
Precocious puberty
History
age <8 years, breast development, growth of axillary and pubic hair, increased growth velocity
Exam
breast development, tall stature
1st investigation
- bone age assessment:
advanced
More - serum follicle stimulating hormone (FSH) and luteinising hormone (LH):
abnormal
More - serum oestrogen:
usually elevated
- androgen panel:
dehydroepiandrosterone (DHEA) and DHEA-sulphate detected
- ultrasound pelvis:
uterine enlargement, endometrial thickening, may show ovarian cysts or tumours
Other investigations
Genital trauma
History
history of trauma, usually straddle injury; hematuria or inability to void urine if urethral injury
Exam
vulval bruising, laceration, haematoma
1st investigation
- none:
clinical diagnosis
Other investigations
- examination under anaesthesia:
variable
More
Vaginal foreign body
History
foul-smelling and/or blood-stained discharge
Exam
vaginal foreign body
1st investigation
- none:
clinical diagnosis
Other investigations
- examination under anaesthesia or sedation:
foreign body present
More
Condylomata acuminata
History
may be history of trauma to genital warts or history of other sexually transmitted infections
Exam
verrucous fleshy papules, may coalesce into plaques
1st investigation
- none:
clinical diagnosis
Other investigations
Use of this content is subject to our disclaimer