Potential causes can be divided according to age: premenarchal, during the reproductive years (non-pregnant and pregnant), and postmenopausal.
Premenarchal bleeding
Uterine bleeding occurs in 3% to 5% of female neonates on day 3-5 of life.[9]Puttemans P, Benagiano G, Gargett C, et al. Neonatal uterine bleeding as a biomarker for reproductive disorders during adolescence: a worldwide call for systematic registration by nurse midwife. J Matern Fetal Neonatal Med. 2017 Jun;30(12):1434-6.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5505234
http://www.ncbi.nlm.nih.gov/pubmed/27454348?tool=bestpractice.com
The neonatal endometrium is shed following maternal progesterone withdrawal.[10]Brosens I, Benagiano G. Is neonatal uterine bleeding involved in the pathogenesis of endometriosis as a source of stem cells? Fertil Steril. 2013 Sep;100(3):622-3.
https://www.fertstert.org/article/S0015-0282(13)00560-8/fulltext
Bleeding after this age (and prior to menarche) is always abnormal. Bleeding is associated with early development of secondary sexual characters, in particular breast development, and probably indicates precocious puberty.
Trauma is the most common cause of vaginal bleeding in girls younger than 10 years.[1]Söderström HF, Carlsson A, Börjesson A, et al. Vaginal bleeding in prepubertal girls: etiology and clinical management. J Pediatr Adolesc Gynecol. 2016 Jun;29(3):280-5.
http://www.ncbi.nlm.nih.gov/pubmed/26506030?tool=bestpractice.com
Local inflammation of the vagina due to infection or a foreign body (e.g., toilet paper) can also cause bleeding.[11]Stricker T, Navratil F, Sennhauser FH. Vaginal foreign bodies. J Paediatr Child Health. 2004 Apr;40(4):205-7.
http://www.ncbi.nlm.nih.gov/pubmed/15009550?tool=bestpractice.com
Rare but serious causes of premenarchal bleeding include sexual abuse and childhood genital malignancy of the vagina.[1]Söderström HF, Carlsson A, Börjesson A, et al. Vaginal bleeding in prepubertal girls: etiology and clinical management. J Pediatr Adolesc Gynecol. 2016 Jun;29(3):280-5.
http://www.ncbi.nlm.nih.gov/pubmed/26506030?tool=bestpractice.com
[12]Dwiggins M, Gomez-Lobo V. Current review of prepubertal vaginal bleeding. Curr Opin Obstet Gynecol. 2017 Oct;29(5):322-7.
http://www.ncbi.nlm.nih.gov/pubmed/28858895?tool=bestpractice.com
Rhabdomyosarcoma is the most common lower genital tract malignancy in young girls, with a peak incidence before age 2 years. Tumours appear as a ‘grape-like’ cluster of tissue.[13]Striegel AM, Myers JB, Sorensen MD, et al. Vaginal discharge and bleeding in girls younger than 6 years. J Urol. 2006 Dec;176(6 Pt 1):2632-5.
http://www.ncbi.nlm.nih.gov/pubmed/17085178?tool=bestpractice.com
Bleeding during reproductive age (not pregnant)
Abnormal bleeding occurs most commonly in this group.
The bleeding source may be anywhere in the reproductive tract including the uterus, the cervix, or the vagina itself. Abnormal uterine bleeding, including abnormal menstrual bleeding and intermenstrual bleeding, is discussed in a separate topic, Evaluation of abnormal uterine bleeding.
Postcoital bleeding is often caused by cervical ectropion, polyps, or cervicitis. Cervical cancer and vaginal cancer are serious causes of postcoital bleeding. Condylomata acuminata and vaginitis may also cause vaginal bleeding.
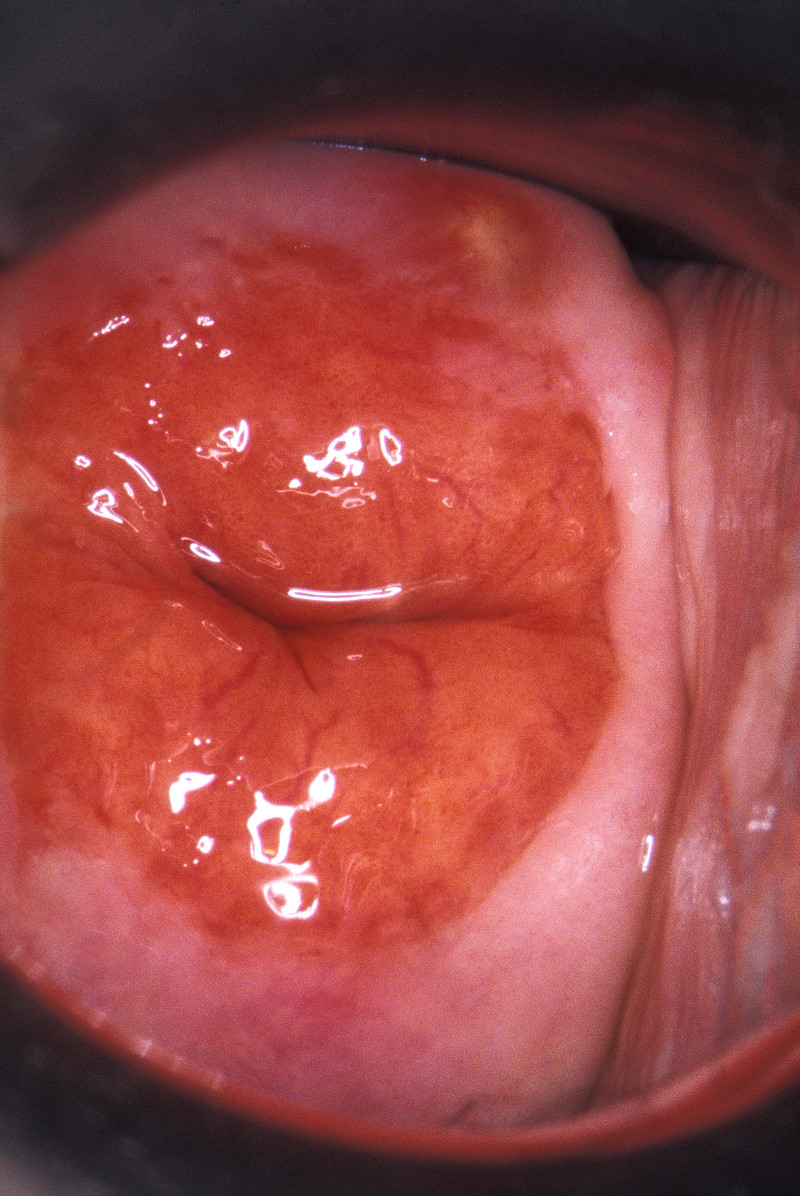
Cervical ectropion
Cervical ectropion (also called cervical erosion) occurs when endocervical glandular epithelium expands beyond the os and becomes visible on the ectocervix. The ectropion tissue is darker pink than the surrounding squamous epithelium and may be friable. Ectropions are commonly seen in adolescent women, pregnant women, and women using hormonal contraception.[14]Tarney CM, Han J. Postcoital bleeding: a review on etiology, diagnosis, and management. Obstet Gynecol Int. 2014;2014:192087.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4086375
http://www.ncbi.nlm.nih.gov/pubmed/25045355?tool=bestpractice.com
Most are asymptomatic.[Figure caption and citation for the preceding image starts]: Cervical erosionScience Photo Library; used with permission [Citation ends].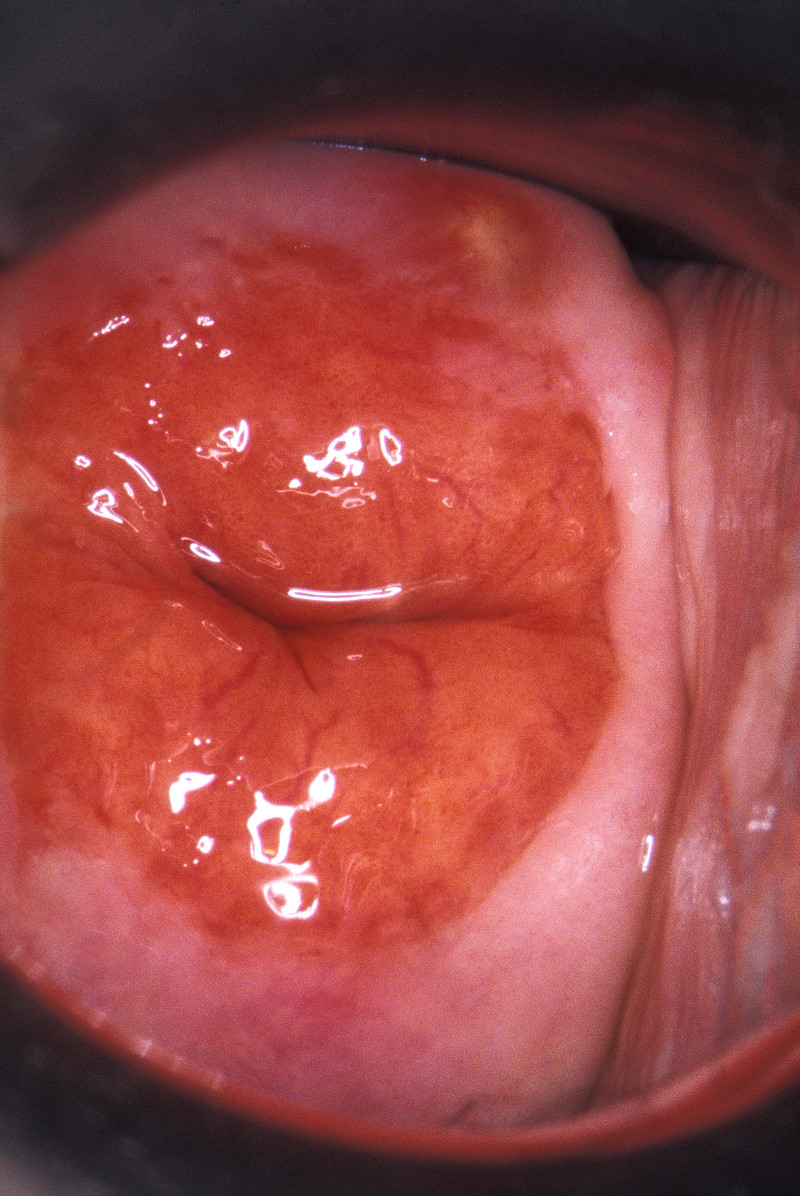
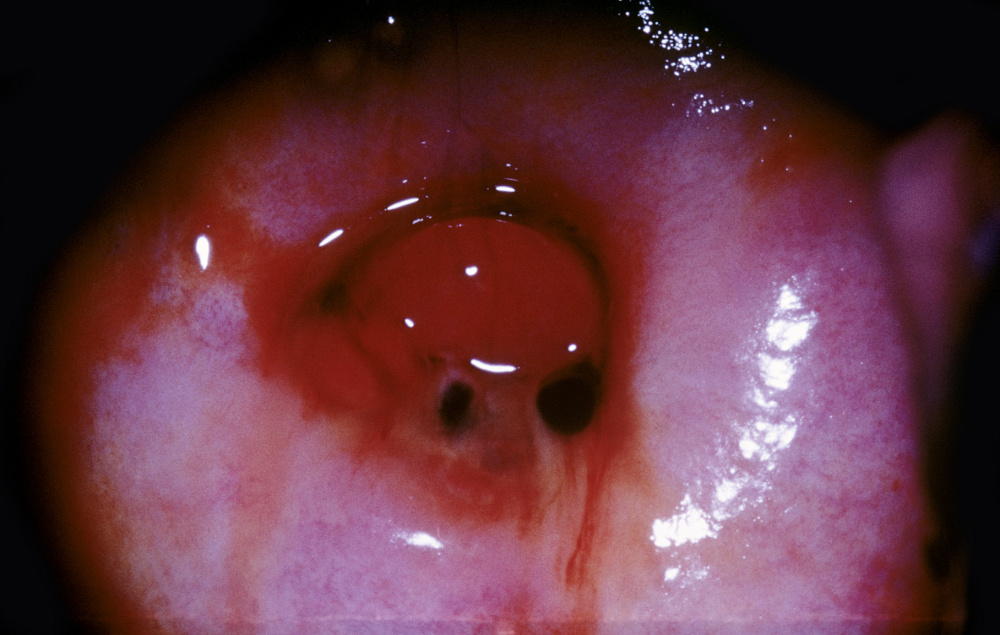
Cervical polyp
Polyps are benign neoplastic growths which can arise from the cervix or endocervix. They typically occur in multiparous patients aged over 40 years. They are often smooth, lobular, and friable. They may be detected incidentally during a speculum examination or cause postcoital bleeding.[14]Tarney CM, Han J. Postcoital bleeding: a review on etiology, diagnosis, and management. Obstet Gynecol Int. 2014;2014:192087.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4086375
http://www.ncbi.nlm.nih.gov/pubmed/25045355?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Cervical polypScience Photo Library; used with permission [Citation ends].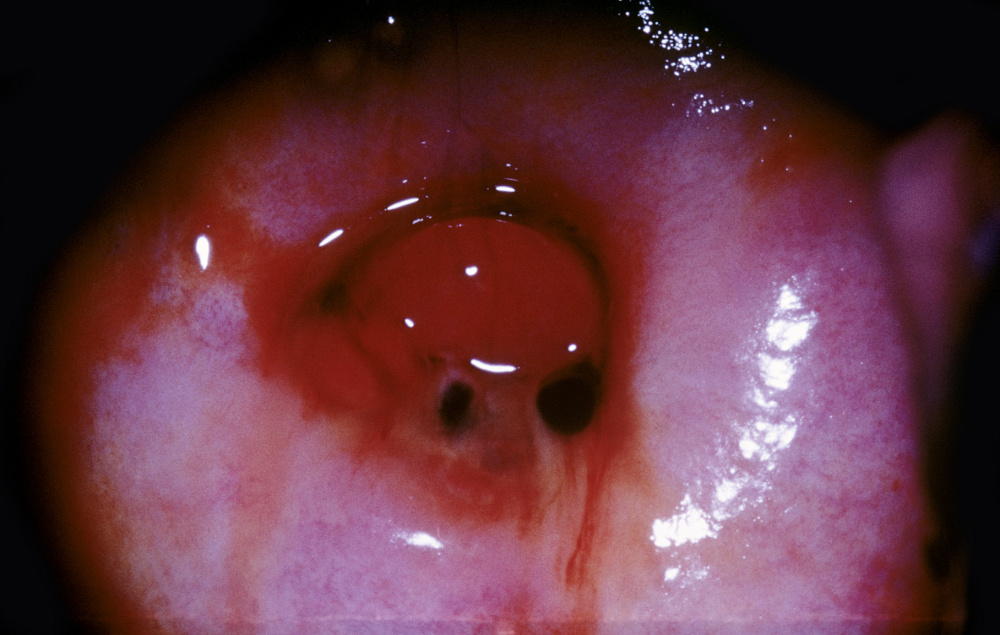
Cervicitis
Infection of the cervix can cause bleeding and is often accompanied by mucopurulent discharge. The most common causative organisms are Chlamydia trachomatis and Neisseria gonorrhoeae, although no organism is identified in many cases.[15]Workowski KA, Bachmann LH, Chan PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8344968
http://www.ncbi.nlm.nih.gov/pubmed/34292926?tool=bestpractice.com
Trichomonas vaginalis, Mycoplasma genitalium, and herpes simplex virus can also cause infectious cervicitis. Infection with these organisms can also cause symptoms of urethritis.
Cervicitis may also occur without infection if the cervix is exposed to mechanical or chemical irritants, e.g., pessaries, diaphragms, tampons, spermicides, or feminine hygiene products.[16]Wilson JF. In the clinic. Vaginitis and cervicitis. Ann Intern Med. 2009 Sep 1;151(5):ITC3-1-ITC3-15; quiz ITC3-16.[17]Taylor SN. Cervicitis of unknown etiology. Curr Infect Dis Rep. 2014 Jul;16(7):409.
http://www.ncbi.nlm.nih.gov/pubmed/24859465?tool=bestpractice.com
Cervical cancer
In addition to vaginal bleeding, cervical cancer may cause malodorous vaginal discharge, although this is rarely the only symptom. Dyspareunia and pelvic or back pain suggest more advanced disease.
Human papillomavirus (HPV) infection is the most important aetiological factor.[18]World Health Organization. Cervical cancer. Mar 2024 [internet publication].
https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
Incidence of cervical cancer correlates with early onset of sexual activity, multiple sexual partners, cigarette smoking, immunosuppression, low socioeconomic status, and oral contraceptive use.[19]International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and sexual behavior: collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer Epidemiol Biomarkers Prev. 2009 Apr;18(4):1060-9.
https://cebp.aacrjournals.org/content/18/4/1060.long
http://www.ncbi.nlm.nih.gov/pubmed/19336546?tool=bestpractice.com
[20]Hessol NA, Whittemore H, Vittinghoff E, et al. Incidence of first and second primary cancers diagnosed among people with HIV, 1985-2013: a population-based, registry linkage study. Lancet HIV. 2018 Nov;5(11):e647-55.
http://www.ncbi.nlm.nih.gov/pubmed/30245004?tool=bestpractice.com
[21]International Collaboration of Epidemiological Studies of Cervical Cancer, Appleby P, Beral V, et al. Cervical cancer and hormonal contraceptives: collaborative reanalysis of individual data for 16,573 women with cervical cancer and 35,509 women without cervical cancer from 24 epidemiological studies. Lancet. 2007 Nov 10;370(9599):1609-21.
http://www.ncbi.nlm.nih.gov/pubmed/17993361?tool=bestpractice.com
Globally, there were approximately 660,000 new cases of cervical cancer, and 350,000 related deaths in 2022.[18]World Health Organization. Cervical cancer. Mar 2024 [internet publication].
https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
One systematic review of UK women with postcoital bleeding reported that the risk of cervical cancer is 1 in 44,000 at age 20-24 years, 1 in 5600 at age 25-35 years, 1 in 2800 at age 35-44 years, and 1 in 2400 at age 45-54 years.[22]Shapley M, Jordan J, Croft PR. A systematic review of postcoital bleeding and risk of cervical cancer. Br J Gen Pract. 2006 Jun;56(527):453-60.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1839021
http://www.ncbi.nlm.nih.gov/pubmed/16762128?tool=bestpractice.com
Vaginal cancer
Primary vaginal cancer is rare, accounting for <1% of cancers affecting individuals assigned female at birth; neoplastic lesions are more commonly metastases.[23]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: vaginal cancer [internet publication].
https://www.nccn.org/guidelines/category_1
HPV infection is the most important aetiological factor.[23]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: vaginal cancer [internet publication].
https://www.nccn.org/guidelines/category_1
Vaginitis
Although vaginitis is a common condition, it is rarely severe enough to cause bleeding. There may be associated vaginal discharge, pruritus, dyspareunia, and dysuria.
Condylomata acuminata
Condylomata acuminata (genital warts) are caused by HPV infection. The infection manifests as verrucous fleshy papules that may coalesce into plaques. The warts can occur anywhere in the anogenital area, including the vaginal and cervical mucosal surfaces, where local trauma can cause bleeding.[24]Wiley DJ, Douglas J, Beutner K, et al. External genital warts: diagnosis, treatment, and prevention. Clin Infect Dis. 2002 Oct 15;35(Suppl 2):S210-24.
https://academic.oup.com/cid/article/35/Supplement_2/S210/316436
http://www.ncbi.nlm.nih.gov/pubmed/12353208?tool=bestpractice.com
Bleeding during pregnancy
Any condition which causes vaginal bleeding in a non-pregnant woman may also cause bleeding in a pregnant woman. The clinician must also consider additional, pregnancy-specific causes. The likely cause of bleeding varies according to gestation.
First trimester
Vaginal bleeding in early pregnancy could be caused by an ectopic pregnancy or miscarriage.[25]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Aug 2023 [internet publication].
https://www.nice.org.uk/guidance/ng126
Ectopic pregnancy refers to the implantation of an embryo outside the uterus, mostly commonly in the fallopian tube.[26]Panelli DM, Phillips CH, Brady PC. Incidence, diagnosis and management of tubal and nontubal ectopic pregnancies: a review. Fertil Res Pract. 2015 Oct 15;1:15.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5424401
http://www.ncbi.nlm.nih.gov/pubmed/28620520?tool=bestpractice.com
Common symptoms are abdominal pain, amenorrhoea, and vaginal bleeding.[25]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Aug 2023 [internet publication].
https://www.nice.org.uk/guidance/ng126
Red flags include unstable vital signs or signs of intraperitoneal bleeding (e.g., acute abdomen, shoulder pain, cervical motion tenderness); urgent surgical intervention may be required to avoid maternal shock and even death.
Risk factors include age over 35 years, previous ectopic pregnancy, smoking, history of pelvic inflammatory disease, prior tubal surgery, and use of assisted reproductive technologies.[26]Panelli DM, Phillips CH, Brady PC. Incidence, diagnosis and management of tubal and nontubal ectopic pregnancies: a review. Fertil Res Pract. 2015 Oct 15;1:15.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5424401
http://www.ncbi.nlm.nih.gov/pubmed/28620520?tool=bestpractice.com
Compared with pregnancies in the general population, a higher proportion of pregnancies conceived with an intrauterine device in place are ectopic.[26]Panelli DM, Phillips CH, Brady PC. Incidence, diagnosis and management of tubal and nontubal ectopic pregnancies: a review. Fertil Res Pract. 2015 Oct 15;1:15.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5424401
http://www.ncbi.nlm.nih.gov/pubmed/28620520?tool=bestpractice.com
[27]Furlong LA. Ectopic pregnancy risk when contraception fails. A review. J Reprod Med. 2002 Nov;47(11):881-5.
http://www.ncbi.nlm.nih.gov/pubmed/12497674?tool=bestpractice.com
Miscarriage is an involuntary, spontaneous loss of a pregnancy before 20-24 completed weeks (gestation varies, depending on country). It is associated with unprovoked vaginal bleeding with or without suprapubic pain. The majority of miscarriages occur in the first trimester. About 30% of all pregnancies may end in miscarriage.[28]Wilcox AJ, Weinberg CR, O'Connor JF, et al. Incidence of early loss of pregnancy. N Engl J Med. 1988 Jul 28;319(4):189-94.
http://www.ncbi.nlm.nih.gov/pubmed/3393170?tool=bestpractice.com
Second and third trimesters
Vaginal bleeding in the second or third trimester occurs less commonly than in the first trimester. Pathological causes of bleeding include bleeding from the cervix with preterm labour, bleeding from placenta praevia, vasa praevia, placental abruption, or uterine rupture.[29]Expert Panel on GYN and OB Imaging; Shipp TD, Poder L, et al. ACR appropriateness criteria® second and third trimester vaginal bleeding. J Am Coll Radiol. 2020 Nov;17(11S):S497-504.
https://www.jacr.org/article/S1546-1440(20)30942-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33153560?tool=bestpractice.com
Miscarriage and cervical change with labour give rise to physiological bleeding.
Placental abruption (premature separation of the placenta from the uterus) complicates 0.3% to 1% of births.[30]Ananth CV, Keyes KM, Hamilton A, et al. An international contrast of rates of placental abruption: an age-period-cohort analysis. PLoS One. 2015 May 27;10(5):e0125246.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4446321
http://www.ncbi.nlm.nih.gov/pubmed/26018653?tool=bestpractice.com
Some cases occur following abdominal trauma.[31]El-Kady D, Gilbert WM, Anderson J, et al. Trauma during pregnancy: an analysis of maternal and fetal outcomes in a large population. Am J Obstet Gynecol. 2004 Jun;190(6):1661-8.
http://www.ncbi.nlm.nih.gov/pubmed/15284764?tool=bestpractice.com
The precise aetiology of non-traumatic cases is unknown. Risk factors include pre-eclampsia, smoking, hypertension, maternal cocaine use, and previous placental abruption.[32]Ananth CV, Smulian JC, Vintzileos AM. Incidence of placental abruption in relation to cigarette smoking and hypertensive disorders during pregnancy: a meta-analysis of observational studies. Obstet Gynecol. 1999 Apr;93(4):622-8.
http://www.ncbi.nlm.nih.gov/pubmed/10214847?tool=bestpractice.com
[33]Addis A, Moretti ME, Ahmed Syed F, et al. Fetal effects of cocaine: an updated meta-analysis. Reprod Toxicol. 2001 Jul-Aug;15(4):341-69.
http://www.ncbi.nlm.nih.gov/pubmed/11489591?tool=bestpractice.com
[34]Rasmussen S, Irgens LM, Dalaker K. Outcome of pregnancies subsequent to placental abruption: a risk assessment. Acta Obstet Gynecol Scand. 2000 Jun;79(6):496-501.
http://www.ncbi.nlm.nih.gov/pubmed/10857875?tool=bestpractice.com
Bleeding is usually accompanied by abdominal pain and contractions.
Placenta praevia is defined as the placenta overlying the cervical os. It can be complete, partial, or marginal, and may resolve as pregnancy progresses. Symptomatic placenta praevia typically presents as second or third trimester painless vaginal bleeding.[29]Expert Panel on GYN and OB Imaging; Shipp TD, Poder L, et al. ACR appropriateness criteria® second and third trimester vaginal bleeding. J Am Coll Radiol. 2020 Nov;17(11S):S497-504.
https://www.jacr.org/article/S1546-1440(20)30942-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33153560?tool=bestpractice.com
Risk factors include previous abnormal placentation, previous caesarean delivery, advanced maternal age, increasing parity, in vitro fertilisation, short interpregnancy intervals, and illicit drug use.[35]Silver RM, Branch DW. Placenta accreta spectrum. N Engl J Med. 2018 Apr 19;378(16):1529-36.[36]Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Effects of birth spacing on maternal health: a systematic review. Am J Obstet Gynecol. 2007 Apr;196(4):297-308.
http://www.ncbi.nlm.nih.gov/pubmed/17403398?tool=bestpractice.com
Low-dose acetylsalicylic acid (ASA) for the prevention of pre-eclampsia does not appear to increase risk for antepartum bleeding.[37]American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Gynecology. ACOG Committee Opinion No. 743: low-dose aspirin use during pregnancy. Obstet Gynecol. 2018 Jul;132(1):e44-52.
https://journals.lww.com/greenjournal/fulltext/2018/07000/acog_committee_opinion_no__743__low_dose_aspirin.57.aspx
http://www.ncbi.nlm.nih.gov/pubmed/29939940?tool=bestpractice.com
[38]Roberge S, Bujold E, Nicolaides KH. Meta-analysis on the effect of aspirin use for prevention of preeclampsia on placental abruption and antepartum hemorrhage. Am J Obstet Gynecol. 2018 May;218(5):483-9.
https://www.ajog.org/article/S0002-9378(17)32812-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29305829?tool=bestpractice.com
ASA to prevent pre-eclampsia may increase risk for postnatal bleeding; evidence is inconsistent.[39]Souter V, Painter I, Sitcov K, et al. Propensity score analysis of low-dose aspirin and bleeding complications in pregnancy. Ultrasound Obstet Gynecol. 2024 Jan;63(1):81-7.
https://obgyn.onlinelibrary.wiley.com/doi/10.1002/uog.27472
http://www.ncbi.nlm.nih.gov/pubmed/37674400?tool=bestpractice.com
[40]Hastie R, Tong S, Wikström AK, et al. Aspirin use during pregnancy and the risk of bleeding complications: a Swedish population-based cohort study. Am J Obstet Gynecol. 2021 Jan;224(1):95.e1-95.
http://www.ncbi.nlm.nih.gov/pubmed/32687818?tool=bestpractice.com
[41]Yip KC, Luo Z, Huang X, et al. The role of aspirin dose and initiation time in the prevention of preeclampsia and corresponding complications: a meta-analysis of RCTs. Arch Gynecol Obstet. 2022 Jun;305(6):1465-79.
http://www.ncbi.nlm.nih.gov/pubmed/34999942?tool=bestpractice.com
[42]Henderson JT, Vesco KK, Senger CA, et al. Aspirin use to prevent preeclampsia and related morbidity and mortality: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2021 Sep 28;326(12):1192-206.
https://jamanetwork.com/journals/jama/fullarticle/2784500
http://www.ncbi.nlm.nih.gov/pubmed/34581730?tool=bestpractice.com
Postmenopausal bleeding
Vaginal bleeding is common in the first 4 to 6 months of oestrogen and progesterone hormone replacement therapy (HRT). Persistent postmenopausal vaginal bleeding, and any postmenopausal bleeding in a woman who is not using HRT, requires further investigation.
Over 90% of women with endometrial cancer experience postmenopausal bleeding, and 9% of women with postmenopausal bleeding have endometrial cancer.[43]Clarke MA, Long BJ, Del Mar Morillo A, et al. Association of endometrial cancer risk with postmenopausal bleeding in women: a systematic review and meta-analysis. JAMA Intern Med. 2018 Sep 1;178(9):1210-22.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6142981
http://www.ncbi.nlm.nih.gov/pubmed/30083701?tool=bestpractice.com
Postmenopausal bleeding is also associated with ovarian cancer.[44]Bankhead CR, Collins C, Stokes-Lampard H, et al. Identifying symptoms of ovarian cancer: a qualitative and quantitative study. BJOG. 2008 Jul;115(8):1008-14.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2607526
http://www.ncbi.nlm.nih.gov/pubmed/18651882?tool=bestpractice.com
Atrophic vaginitis associated with hypo-oestrogenism is common in postmenopausal women. Bleeding associated with atrophic vaginitis may be encountered after mechanical trauma associated with intercourse, with the use of imperfectly fitting vaginal pessaries, or unprovoked.