Monitoring
Surveillance at a spina bifida centre is recommended at least every 3 months during the first 2 years, every 6 months for pre-school children, and annually for school-age children, adolescents, and adults. It is essential that every clinical encounter include a systematic review of signs and symptoms of:
Shunt malfunction (headache, vomiting, somnolence, personality change, rapid head growth, seizures)
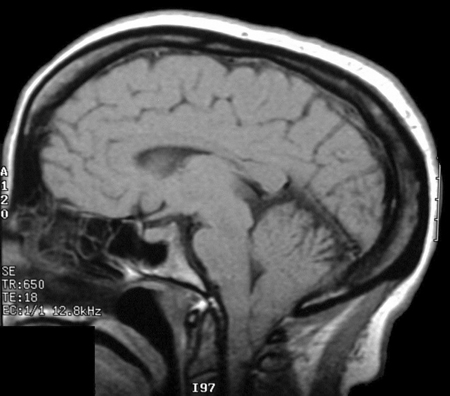
Chiari II malformation (ophthalmoplegia; sleep apnoea; arching of the neck; dysphagia)[Figure caption and citation for the preceding image starts]: Brain MRI scan showing Chiari malformationFrom the collection of Dr Nienke P. Dosa; used with permission [Citation ends].
Syrinx (shoulder numbness; hyperreflexia or asymmetry of the upper extremities; progressive scoliosis; hand weakness; ulnar nerve entrapment; carpal tunnel syndrome)
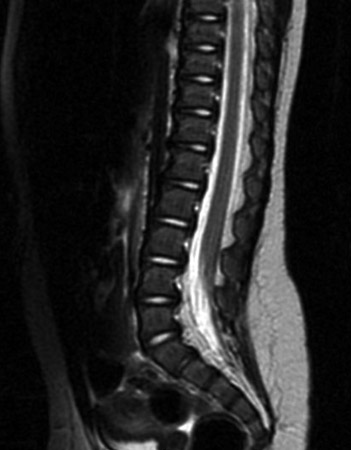
Tethered cord (back pain; rapidly progressive scoliosis; evolving cavovarus deformity; leg spasms; change in motor or sensory level; change in bowel, bladder, or sexual functioning; progressive symptoms associated with Chiari malformation)[Figure caption and citation for the preceding image starts]: Spine MRI scan showing tethered cordFrom the collection of Dr Nienke P. Dosa; used with permission [Citation ends].
Bowel and bladder functioning.
Furthermore, the skin should always be inspected for pressure or friction sores at common pressure sites, including areas overlying the ischial tuberosities, coccyx, calcaneus, and ankles, and between the toes.
Additional assessments and follow-up investigations depend on the age group.
Infancy
Because bladder function can change significantly as spinal shock from cele repair resolves, it is essential to monitor upper tracts with serial renal and bladder ultrasound studies on a quarterly basis during the first year of life. Hydronephrosis warrants further investigation with video-urodynamics or a voiding cystourethrogram (VCUG). Urodynamics is recommended between 6 to 12 months of age to determine whether clean intermittent catheterisation is needed. If a child develops urinary tract infections (UTIs), video-urodynamics or VCUG is used to identify reflux and to guide initiation of antibiotic prophylaxis.
Asymptomatic infants who have stable, mild, or moderate ventriculomegaly may be monitored safely for up to 5 months with cranial ultrasound as long as cortical mantle thickness is at least 3.5 cm. Hydrocephalus is unlikely to progress after 9 months of age.
An MRI of the head is obtained after shunt placement and used as a baseline study to document ventricle size and structural brain anomalies, including the Chiari II malformation. Comparison studies may be obtained if there are signs or symptoms of shunt malfunction. CT head may also be obtained as a baseline study, although caution should be used to limit radiation exposure whenever possible.
Early childhood
The focus should be on careful review of fine motor, gross motor, language, social, and adaptive functioning, and the developmental and social support services that are in place to assist the family. Formal developmental assessment using standardised instruments is necessary to assess these elements. In addition, specific attention should be paid to physiotherapy goals, orthotics, and/or other equipment needs. Concerns regarding vision should be elicited because visual motor integration difficulties can be an early sign of non-verbal learning disability.
Changes should be noted in walking ability and endurance. New muscle atrophy and any loss of motor milestones (crawling, walking, and sitting) should be evaluated. Equipment used should be discussed, such as leg braces, bath equipment, and wheeled mobility, as well as the presence of stairs in the home and ability to traverse them.
Height, weight, and BMI should be measured at each visit. Short stature may result from a combination of scoliosis and precocious puberty.
Strabismus affects up to 20% of children with myelomeningocele. Ophthalmological referral is recommended.
Orthopaedic assessment should include re-evaluation of scoliosis, kyphosis, hip adduction contractures, and orthopaedic deformities such as club foot, equinovarus, calcaneus valgus, or vertical talus. Manual muscle testing of the lower and upper extremities should be performed, with particular focus on changes in muscle tone or atrophy (e.g., presence of spasticity, asymmetry in muscle strength). An anteroposterior pelvis x-ray is usually done at age 2 years to establish whether there is hip dysplasia or dislocation, which may affect gait or sitting balance, or contribute to pressure sores on the hips or buttocks.[115] Scoliosis series is necessary for evaluation of progression of the curve every 1 to 2 years, or if there is concern of progression.
Routine surveillance of bladder function with serial renal and bladder ultrasound studies is recommended every 6 to 12 months until school age (annually for older children and adolescents). If hydronephrosis is noted, video-urodynamics or voiding cystourethrogram is performed in order to identify reflux and to guide initiation of antibiotic prophylaxis. Although a baseline urodynamic study is usually performed between 6 and 12 months old, it is also indicated whenever there is concern regarding a change in bladder function. It is used to determine whether the patient has a high-risk versus low-risk bladder with regards to upper tract deterioration. Some centres include annual urodynamic studies in their protocol for tethered cord surveillance.[157]
Independence with self-care for bowel and bladder management should be attained by the age of 7 years. The antegrade colonic enema is a safe surgical treatment option for severe constipation and faecal soiling that facilitates independence and that has been shown to improve the quality of life for children and families.[158]
CT head study and shunt series is indicated in the acute setting only if there are signs or symptoms of shunt malfunction. MRI is preferred in the non-acute setting for detailed visualisation of neuroanatomy to guide surgical intervention.
Sleep study is indicated if there is slow growth, frequent wheezing, choking, or gagging, or if history suggests sleep apnoea.[159][160]
School age and adolescence
School performance, social functioning, and independence with self-care (e.g., intermittent catheterisation, daily skin checks, and transfer technique) should be the focus in this age group. It is appropriate to involve the patient directly from an early age. Youths should be offered part of an appointment without parents, to discuss sensitive topics such as risk-taking behaviour and mood, and should be a key informant during the history if cognitively able.
It is important to monitor school performance closely, because academic decline can be a subtle presentation of shunt malfunction. The presence of non-verbal learning disability, executive dysfunction, and attention deficit should be evaluated. Neuropsychological assessment to identify subtle short-term memory deficits and visual-motor difficulties should be arranged for children who do not respond to adaptations and appropriate educational interventions.
It is also important to specifically ask about exercise and nutrition, and to review lifestyle measures for the prevention of obesity.
Mobility should be monitored, and notes should be made of the chosen forms of functional mobility (walking, with devices, or wheeled). Maintenance of knee range of motion becomes difficult with limb growth, and may require soft-tissue releases (hamstrings) to maintain walking efficiency. Ankle muscle imbalance may also require correction to keep the foot in a weight-bearing position. Bone surgery to prevent foot deformity with growth and to correct tibial torsion can be offered. Surgical correction for scoliosis may be considered if severe, but may adversely affect walking and transfers. Anterior spinal fusion is preferred over combined anterior-posterior fusion for this reason.[161] It is necessary to ensure that the child has access to the kitchen and bathroom to develop skills, and is able to leave the home in case of emergency, via stairs or ramp if needed.
For adolescents who have had augmentation cystoplasty (a procedure aimed at improving urinary continence), it is recommended that electrolytes, urea, and creatinine be monitored annually. Creatinine clearance, in addition to electrolytes, urea, and creatinine, should also be monitored annually for patients with an ileal conduit (indicated when adherence and/or fine motor difficulties preclude independence with bladder management).
Screening renal and bladder ultrasound should be obtained annually if the patient is stable and there are no intercurrent UTIs. As for the younger age groups, MRI or CT head and shunt series is indicated only if there are signs or symptoms of shunt malfunction. A sleep study is usually necessary if there is a history of sleep apnoea. MRI brain and spine should be ordered if there are progressive symptoms associated with the Chiari malformation. Plain posteroanterior or lateral spine films should be obtained at the onset of the pre-adolescent growth spurt and monitored every 6 to 12 months if there is a clinical scoliosis. Gait analysis may assist in planning orthopaedic procedures. Pressure mapping of the seating device may help determine areas of pressure and facilitate correction for recurrent ischial pressure sores.
Adults
Although most patients with spina bifida do not have an intellectual disability, many of those with shunted hydrocephalus have some degree of non-verbal learning disability and/or executive dysfunction. This can have a significant impact on their ability to navigate the healthcare system and to follow through on medical recommendations. It is therefore important to explore social support and agency connections for independent living, transportation, and coordination of care. Detailed information should also be sought regarding difficulties with short-term memory, decision making, taking initiative, and organisation. It is important to identify adaptations (e.g., reminder watch for catheterisation) and supports (vocational counselling) that are in place for the adult patient with non-verbal learning disability and/or executive dysfunction.
Funding streams for durable medical equipment and home health services should also be identified. It is useful to ask the patient to identify key individuals or entities with which communication may be anticipated. Guardianship should be considered for adults who cannot give informed consent or manage finances.
Orthopaedic assessment should address baseline functioning and any changes in mobility, transfers, presence of back or leg pain, past orthopaedic surgeries, and history of fractures. Activities of daily living should be discussed with regards to how they are completed, what equipment is used, and if the equipment is appropriate and in good repair. This includes braces, crutches or walker, wheelchair, bath equipment, and ramp or lift. Household accessibility for daily activities and community transportation options should also be reviewed.
Screening renal and bladder ultrasound is obtained annually if the patient is stable and there are no intercurrent UTIs. For patients who have had augmentation cystoplasty (a procedure aimed at improving urinary continence), it is recommended that electrolytes, urea, and creatinine be monitored annually. In addition, an annual cystoscopy to evaluate for bladder cancer is recommended beginning 10 years after the surgery is performed, due to a lifetime risk of developing bladder cancer at the anastomosis site. Creatinine clearance, as well as electrolytes, urea, and creatinine, should be monitored once a year for patients with an ileal conduit (indicated when adherence and/or fine motor difficulties preclude independence with bladder management).
An MRI brain and spine and shunt series is recommended in early adulthood to document baseline anatomy. A CT head and shunt series is obtained in the acute setting if there are signs or symptoms of shunt malfunction such as headache and swelling along the shunt tract. An MRI spine is also obtained if there are symptoms of tethered cord such as back pain, rapidly progressive scoliosis, change in motor or sensory level, or change in bowel or bladder functioning. Shunt status should always be evaluated if there are signs or symptoms of tethered cord. MRI brain and spine is indicated if there are progressive symptoms associated with the Chiari malformation such as choking, gagging, new ophthalmoplegia or dysarthria, arching of neck, occipital notch tenderness, and sleep apnoea. Sleep study is obtained if there is a history of sleep apnoea.
Careful skin examination for pressure or friction injury at insensate areas is essential. Pressure mapping of the seating device may help determine areas of pressure and facilitate correction for recurrent ischial pressure sores. Patients should be reminded about proper transfer technique and to periodically elevate their legs. This is because venous stasis and lymphoedema are common among adults with spina bifida.[127]
Use of this content is subject to our disclaimer