History and exam
Key diagnostic factors
common
constitutional symptoms
In bubonic plague the onset of fever, malaise, and prostration is sudden and coincides with lymphadenitis. Fever is almost always present.[27]
Patients with septicaemic plague also present with systemic features such as fever and hypotension.
lymphadenitis (bubonic plague)
Characterised by tender, swollen lymph nodes close to the site of a flea bite (possibly with necrotic areas). Inguinal nodes are most commonly affected. Anterior cervical nodes are usually inflamed in plague pharyngitis.[34][Figure caption and citation for the preceding image starts]: Axillary buboFrom the image collection of the CDC; used with permission [Citation ends].
haemoptysis (pneumonic plague)
Pneumonic plague has a sudden onset and usually causes blood-stained sputum.
Pneumonic plague is the most likely clinical form after a deliberate release of aerosolised Yersinia pestis.
diarrhoea (yersiniosis)
Adults generally present with diarrhoea, which may last for ≥3 weeks.
abdominal pain (yersiniosis)
Yersiniosis may cause abdominal pain indistinguishable from appendicitis. In adults, abdominal pain may last for ≥3 weeks.
Other diagnostic factors
common
pleuritic chest pain (pneumonic plague)
Pneumonic plague has a sudden onset and usually causes pleuritic chest pain.
Pneumonic plague is the most likely clinical form after a deliberate release of aerosolised Yersinia pestis.
dyspnoea (pneumonic plague)
May be a symptom of primary pneumonic plague.
Risk factors
strong
exposure to fleas (plague)
The rat flea Xenopsylla cheopis is the most efficient plague vector, but a wide range of animal fleas can transmit plague. Domestic animals, such as dogs or cats, may also become infected with plague after contact with infected rats or rabbits or after being bitten by an infected flea. Owners or veterinary staff may become infected after flea bites or after inhaling droplets containing the plague bacilli. Five of 23 patients with cat-associated plague reported from western states of the US between 1977 and 1998 died.[16][Figure caption and citation for the preceding image starts]: A female Xenopsylla cheopis flea, also known as the oriental rat fleaFrom the image collection of the CDC; used with permission [Citation ends].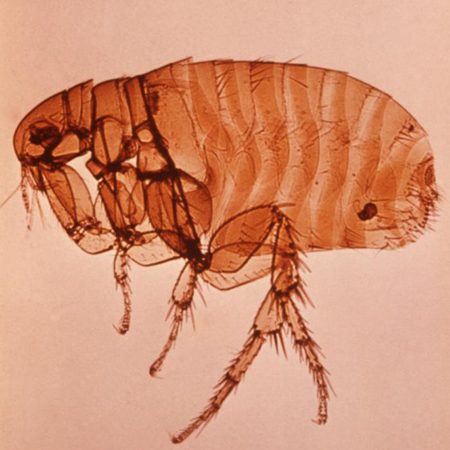
residence in, or travel to, an endemic area (plague)
Plague exists worldwide. It is endemic in rural areas of central and southern Africa (especially Madagascar, Democratic Republic of Congo, and Uganda), central Asia and the Indian subcontinent, northeastern parts of South America, and western parts of the US. Cases are most common in Africa (particularly Madagascar).[10][11] Currently, the most endemic countries are Madagascar, the Democratic Republic of the Congo, and Peru.[9]
The US contains extensive natural foci of plague, but cases are rare, probably because these areas are sparsely inhabited. The natural foci of plague in North America occur in 15 western regions of the US and its bordering countries, including southwestern Canada and northern Mexico.[12] CDC: map of plague in the US Opens in new window
contact with infected animals (plague)
Domestic animals, such as dogs or cats, may become infected with plague after contact with infected rats or rabbits or after being bitten by an infected flea. Owners or veterinary staff may become infected after flea bites or after inhaling droplets containing the plague bacilli. Five of 23 patients died with cat-associated plague reported from western states of the US between 1977 and 1998.[16]
bioterrorism (plague)
Yersinia pestis is categorised as a tier 1 bioterrorism select agent due to its low infectious dose, high case fatality rate, and history of use as an agent of bioterrorism.[2]
From antiquity through to the 20th century, plague has been used as a biological weapon. Aerosolised plague bacilli released in a confined space would cause significant mortality. An outbreak of pneumonic plague in a non-endemic area should raise suspicion of deliberate release.
young children (yersiniosis)
Yersinia enterocolitica infection is most common in young children but also affects adults. In one report, 77% of cases occurred in children aged <12 months.[24]
Complications such as erythema nodosum and reactive arthritis are more common in adults.
consumption of raw or undercooked pork products (yersiniosis)
The highest incidence of Yersinia enterocolitica infection is in northern Europe, where consuming raw or undercooked pork products is a major risk factor.[25]
weak
exposure to people with plague (plague)
Pneumonic plague is the only clinical form that is transmissible from person to person; however, this is uncommon.[7]
iron-overload syndromes (yersiniosis)
Syndromes such as beta-thalassaemia and haemachromatosis are a risk factor for Yersinia enterocolitica bacteraemia.[3]
chronic liver disease, diabetes, alcoholism (yersiniosis)
Risk factors for Yersinia enterocolitica bacteraemia.[3]
Use of this content is subject to our disclaimer