Investigations
1st investigations to order
fetal monitoring
Test
In cases of suspected placental abruption, the fetal heart rate should be monitored continuously, at least initially. Depending on how stable the mother and fetus are, and gestational age at presentation, monitoring may later be done intermittently on a case-by-case basis.
Result
abnormalities in the tracing that suggest an abruption: late decelerations, loss of variability, variable decelerations, a sinusoidal fetal heart rate tracing, and fetal bradycardia, defined as a persistent fetal heart rate below 110 beats per minute
Hb and haematocrit
Test
Should be ordered in all women with bleeding or in whom abruption is suspected. May be normal if not much blood has been lost, or before volume replacement has occurred. In cases of severe blood loss or prolonged bleeding, anaemia may be present.
Result
normal or low
coagulation studies
Test
Includes PT, PTT, fibrinogen, and fibrinogen breakdown products.
Should be ordered in all women suspected of having placental abruption. Particularly important in cases with fetal death, or where clotting seems impaired. Likely to be abnormal, particularly in cases of large abruptions associated with fetal death, and in cases of concealed abruption.
Disseminated intravascular coagulation (DIC) occurs typically in the presence of abruptions large enough to cause fetal death, and should be suspected if the mother bleeds persistently without clotting.
A simple test to confirm DIC is to take some blood in a plain tube (without anticoagulation), and then invert the tube at 1-minute intervals. The blood should clot within 8 to10 minutes; failure to do so may be taken as evidence of DIC.
If DIC occurs, the fibrinogen levels will be low. In addition, the PT will be prolonged.
Result
abnormal
Kleihauer-Betke (K-B) test
Test
Should only be ordered in Rh-negative women to assess the need for additional Rh immune globulin.[50] The level of fetal red blood cells aids in determining the amount of Rh immune globulin to administer.[50]
Although a positive K-B test in cases of abruption would be expected, studies have not found this to be so.[51][52] Most women with a clinical abruption will have a negative K-B test, whereas the test may be positive in women without abruption. For this reason, routinely performing a K-B test to aid in the diagnosis of abruption is not recommended.[51][58]
Result
fetal red blood cells in the maternal circulation; variable
ultrasound
Test
Ultrasound may or may not be helpful in the diagnosis of placental abruption.[46][53] Detection rates of only 12% to 25% are generally reported.[54] However, in skilled hands, high rates of diagnosis have been reported.[55] If there is ultrasound evidence of placental abruption, the positive predictive value is high.[56][Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].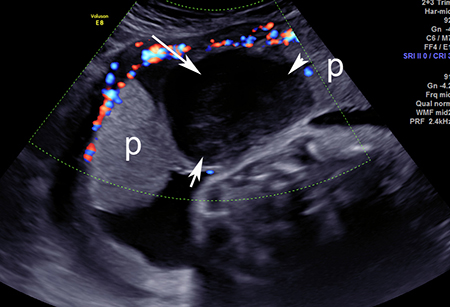 [Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].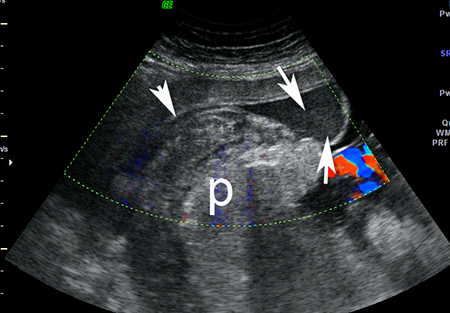 [Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].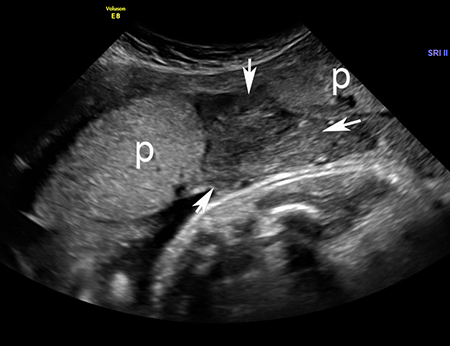
Ultrasound may be performed by a transabdominal, transvaginal, or transperineal approach, although transabdominal ultrasound is the preferred initial procedure for assessment of the placenta.[46] Transvaginal ultrasound may be used if transabdominal examination is inconclusive or inadequate.[46] Transperineal ultrasound may be beneficial in the presence of bulging or ruptured membranes.[46] Colour flow Doppler ultrasound is useful because a lack of blood flow may help distinguish between clots in the uterus (in which case blood flow will be not be demonstrable), and normal placental tissue, which will demonstrate blood flow.[46]
Retroplacental haematomas are associated with the worst prognosis. However, in most situations, the sensitivity of ultrasound for abruption may not be high enough, and therefore the diagnosis must be made clinically.[46] Ultrasound is also crucial for excluding other causes for the bleeding or pain such as placenta praevia, vasa previa, or uterine rupture.[46]
Result
retroplacental haematoma (hyperechoic, isoechoic, hypoechoic); pre-placental haematoma (jiggling appearance with a shimmering effect of the chorionic plate with fetal movement); increased placental thickness and echogenicity; sub-chorionic collection or marginal collection
Investigations to consider
placental pathology
Test
May give some insight as to the cause of the abruption. Acute abruptions may not be diagnosed by pathology, whereas abruptions that occur from a long-standing process may often have evidence of the inciting process on pathological examination.
Result
retroplacental clot, evidence of thrombosis or infarction within the placenta, inflammatory lesions of the placenta, or perivillous fibrin deposition
Use of this content is subject to our disclaimer