Approach
A high index of suspicion must be maintained in order to diagnose placental abruption. The diagnosis should be suspected in any pregnant woman who presents with vaginal bleeding and/or abdominal pain in the second half of pregnancy.[46] If the fetus is dead and classic clinical signs of abruption are present, the diagnosis is relatively easy. The diagnosis may be more difficult in women with concealed abruption.[46] In such women, ultrasound may be particularly helpful. In some cases, abruption may be seen on ultrasound as a clot behind the placenta, as a clot within the amniotic cavity, or as a thickened, heterogeneous placenta.[46] In other cases, placental abruption may be totally asymptomatic. Occasionally, abruption may be found incidentally on ultrasound performed for other reasons.
History and physical examination
If possible a detailed history should be obtained to try to ascertain whether the pregnant woman has any of the risk factors associated with placental abruption. Questions should include whether the mother smokes or uses cocaine, if she has been subject to any trauma (e.g., been involved in a motor vehicle accident or victim of domestic violence), or if she has hypertension.
A detailed obstetric history should be taken, including questions on prior caesarean deliveries, preterm premature rupture of membranes, prior placental abruption, multi-fetal gestations, multiparity, and known uterine fibroids or uterine malformations.
Common symptoms are abdominal pain, uterine contractions, and uterine tenderness. Vaginal bleeding is also considered a classic symptom, but it is important to note that it may not be present in cases of concealed abruption, particularly if the placenta is located posteriorly within the uterus. In these women lower back pain may be the only presenting symptom.[47] Fetal death is common if more than 50% of the placenta is separated.[48]
Fetal monitoring
In cases of suspected placental abruption, the fetal heart rate should be monitored continuously, at least initially. Abnormalities in the tracing that suggest an abruption include late decelerations, loss of variability, variable decelerations, a sinusoidal fetal heart rate tracing, and fetal bradycardia, defined as a persistent fetal heart rate below 110 beats per minute.[18][49] Depending on how stable the mother and fetus are, and the gestational age at presentation, the monitoring may later be done intermittently on a case-by-case basis.
Laboratory tests
Haemoglobin (Hb), haematocrit (Hct), and coagulation studies (prothrombin time [PT], partial thromboplastin time [PTT], fibrinogen, and fibrinogen breakdown products) should be ordered immediately in all pregnant women with bleeding in whom abruption is suspected. Soon after abruption, these test results may return to normal. If severe blood loss has occurred over a period of time, the Hb and Hct levels may be low (<10 mg/dL and <30%, respectively).
Disseminated intravascular coagulation (DIC) occurs typically in the presence of abruptions large enough to cause fetal death and should be suspected if the mother bleeds persistently without clotting. A simple test to confirm DIC is to take some blood in a plain tube (without anticoagulation), and then invert the tube at 1-minute intervals. The blood should clot within 8 to 10 minutes; failure to do so may be taken as evidence of DIC. If DIC occurs, the fibrinogen levels will be low. In addition, the PT will be prolonged.
A Kleihauer-Betke (K-B) test should be ordered in Rh-negative women to assess the need for additional Rh immune globulin.[50] It is rarely positive in cases of abruption, and may be positive in women without abruption. For this reason, performing a K-B test to aid in the diagnosis of abruption is not recommended.[51][52]
Ultrasound
Ultrasound may or may not be helpful in the diagnosis of placental abruption but is a useful initial investigation.[46][53][Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].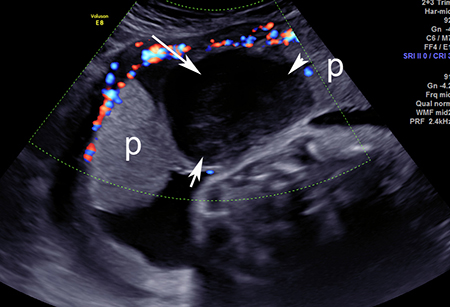 [Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].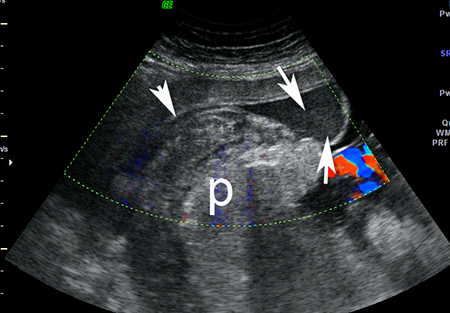 [Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of placental abruption: normal placenta is marked 'p'; area of abruption depicted by white arrowsFrom the collection of Dr Y Oyelese; used with permission [Citation ends].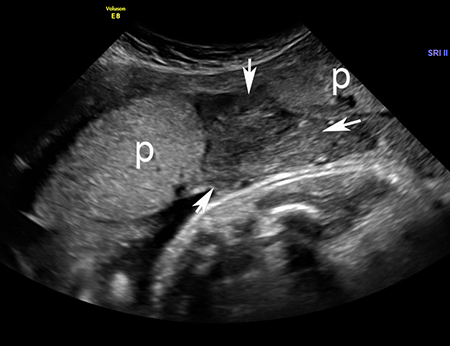 Detection rates of only 12% to 25% are generally reported.[54] However, in skilled hands, high rates of diagnosis have been reported.[55] If there is ultrasound evidence of placental abruption, the positive predictive value is high.[56] Retroplacental haematomas are associated with the worst prognosis. However, in most situations, the sensitivity of ultrasound for abruption may not be high enough, and therefore the diagnosis must be made clinically.[46] Ultrasound is also crucial for excluding other causes for the bleeding or pain, such as placenta praevia , vasa previa, or uterine rupture.[46]
Detection rates of only 12% to 25% are generally reported.[54] However, in skilled hands, high rates of diagnosis have been reported.[55] If there is ultrasound evidence of placental abruption, the positive predictive value is high.[56] Retroplacental haematomas are associated with the worst prognosis. However, in most situations, the sensitivity of ultrasound for abruption may not be high enough, and therefore the diagnosis must be made clinically.[46] Ultrasound is also crucial for excluding other causes for the bleeding or pain, such as placenta praevia , vasa previa, or uterine rupture.[46]
Ultrasound may be performed by a transabdominal, transvaginal, or transperineal approach, although transabdominal ultrasound is the preferred initial procedure for assessment of the placenta.[46] Transvaginal ultrasound may be used if transabdominal examination is inconclusive or inadequate.[46] Transperineal ultrasound may be beneficial in the presence of bulging or ruptured membranes.[46] Absence of blood flow on Colour flow Doppler ultrasound may help in distinguishing between clots in the uterus (in which case blood flow will be not be demonstrable) and normal placenta (which would demonstrate blood flow), and is therefore recommended to support the diagnosis.[46]
Helpful ultrasound signs include any of the following:[57]
Retroplacental haematoma (hyperechoic, isoechoic, hypoechoic)
Pre-placental haematoma (jiggling appearance with a shimmering effect of the chorionic plate with fetal movement)
Increased placental thickness and echogenicity
Sub-chorionic collection
Marginal collection.
A placenta in the lower uterine segment reaching the internal os suggests placenta praevia rather than abruption.[46] Although a placenta praevia may separate prematurely, these are not usually regarded as abruptions. Caution is necessary not to mistake a clot overlying the cervix for a placenta praevia.
Pathology
Placental pathology may give some insight as to the cause of the abruption. Acute abruptions may not be diagnosed by pathology, whereas abruptions that occur from a long-standing process may often have evidence of the inciting process on pathological examination. Lesions found may include retroplacental clot, evidence of thrombosis or infarction within the placenta, inflammatory lesions of the placenta, or perivillous fibrin deposition.
Use of this content is subject to our disclaimer