Approach
Residing in or travelling to areas of endemicity are important epidemiological clues. Men are infected more often than women, presumably due to increased outdoor environmental exposures. Detailing of potential employment or recreational exposures in the outdoors is important. Because blastomycosis is a common infection in dogs, disease to dogs in the endemic area can be a clue to the diagnosis. Otherwise, there are no pathognomonic features.
Symptoms
The majority of people acutely infected with Blastomyces dermatitidis develop asymptomatic, self-limiting pulmonary infections. Patients with overt disease may have cough or constitutional symptoms. The presentation is frequently as a community-acquired pneumonia with purulent sputum. A high level of clinical suspicion is needed as the diagnosis is often missed or delayed. Patients frequently undergo one or more courses of antibiotics before the disease is considered, after the patient has failed to improve or worsens. The course may be weeks or months. Other presentations may include:
Acute monoarticular septic arthritis
Skin lesions (nodular, ulcerated, or verrucous)
Focal neurological symptoms or altered level of consciousness
Dysuria or other symptoms of prostatitis.
In addition, many people have evidence of past asymptomatic disease according to serological or skin testing, but the specificity and sensitivity of these tests are not reliable.
Physical examination
Rales may be heard on pulmonary auscultation. Complete examination of the skin is important to evaluate for cutaneous lesions, as well as careful examination of the joints to rule out osteoarticular involvement. Focal neurological deficits may be found. Men may have prostatic or testicular tenderness. [Figure caption and citation for the preceding image starts]: Cutaneous blastomycosis on the forearmPersonal files of Larry Baddour, MD [Citation ends].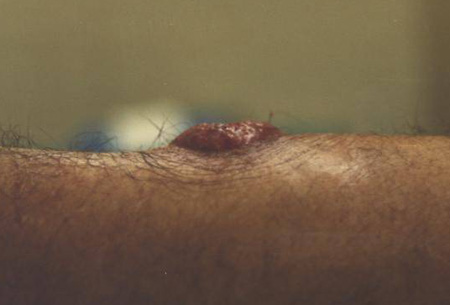 [Figure caption and citation for the preceding image starts]: Cutaneous blastomycosis on the lower extremityLuAnn Ziemer, Office of Medical Photography, Mayo Clinic, Rochester, MN [Citation ends].
[Figure caption and citation for the preceding image starts]: Cutaneous blastomycosis on the lower extremityLuAnn Ziemer, Office of Medical Photography, Mayo Clinic, Rochester, MN [Citation ends]. [Figure caption and citation for the preceding image starts]: Cutaneous blastomycosis on the lower extremityLuAnn Ziemer, Office of Medical Photography, Mayo Clinic, Rochester, MN [Citation ends].
[Figure caption and citation for the preceding image starts]: Cutaneous blastomycosis on the lower extremityLuAnn Ziemer, Office of Medical Photography, Mayo Clinic, Rochester, MN [Citation ends]. [Figure caption and citation for the preceding image starts]: Cutaneous manifestation of disseminated blastomycosisPersonal files of Larry Baddour, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Cutaneous manifestation of disseminated blastomycosisPersonal files of Larry Baddour, MD [Citation ends].
Diagnostic studies
Enzyme immunoassay (EIA) urine antigen testing should be considered in the first instance in patients presenting with community-acquired pneumonia of unknown aetiology who have not responded to one or more courses of antibiotics, and that have a relevant epidemiological history.[30][31] EIA urine antigen tests have a quick turnaround time if available locally, and a positive result indicates probable acute pulmonary blastomycosis.[30][31] While urine is preferred, the assay is also clinically available for use on serum, cerebrospinal fluid (CSF) or bronchoalveolar lavage samples.[2][32]
Patients with pulmonary involvement should also have a chest x-ray and respiratory tract specimen smear and culture if possible. If expectorated sputum is unobtainable or non-revealing, bronchoscopy is performed. Patients with joint involvement undergo arthrocentesis with Gram stain and culture. Negative results are a clue to the diagnosis. Those with skin lesions undergo biopsy. [Figure caption and citation for the preceding image starts]: Pulmonary blastomycosis with focal infiltrates on chest x-rayDr Robert Orenstein, DO, Associate Professor of Medicine, Division of Infectious Diseases, Mayo Clinic, Scottsdale, AZ [Citation ends]. [Figure caption and citation for the preceding image starts]: Pulmonary blastomycosis presenting as a miliary pattern on chest x-rayDr Robert Orenstein, DO, Associate Professor of Medicine, Division of Infectious Diseases, Mayo Clinic, Scottsdale, AZ [Citation ends].
[Figure caption and citation for the preceding image starts]: Pulmonary blastomycosis presenting as a miliary pattern on chest x-rayDr Robert Orenstein, DO, Associate Professor of Medicine, Division of Infectious Diseases, Mayo Clinic, Scottsdale, AZ [Citation ends]. [Figure caption and citation for the preceding image starts]: Close-up of reticulonodular findings on chest x-ray in disseminated blastomycosisPersonal files of Larry Baddour, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Close-up of reticulonodular findings on chest x-ray in disseminated blastomycosisPersonal files of Larry Baddour, MD [Citation ends].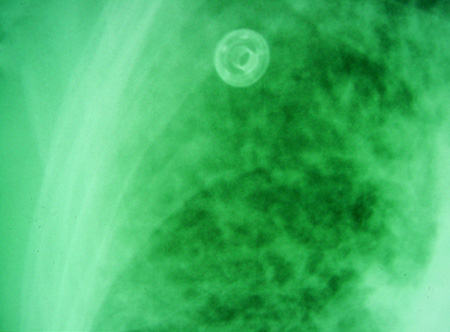
The direct pathological examination of clinical specimens such as sputum, bronchoalveolar washings, endoscopic lymph node needle aspiration, or cutaneous lesions is sufficient to provide quick diagnosis.[2][33] The hallmark of the pathological diagnosis is the demonstration of the characteristic yeast form, usually 8 to 15 micrometres in diameter, with a thick refractile cell wall and typical single broad-based budding.[2][34][35] The yeast form can be seen on haematoxylin-and-eosin, Gomori-methenamine silver, or periodic acid-Schiff staining.[35][Figure caption and citation for the preceding image starts]: Direct potassium hydroxide preparation at 40x magnification of a sputum specimenNancy L. Wengenack, PhD, D(ABMM), Director of Mycology and Mycobacteriology Laboratories, Assistant Professor of Microbiology abd Lab Medicine, Mayo Clinic, Rochester, MN [Citation ends].
For definitive diagnosis, these specimens should also be sent for fungal culture to confirm B dermatitidis, as this remains the gold standard diagnostic method.[2][36] Laboratory identification of B dermatitidis in culture historically depended on conversion from the mould to yeast form at 37°C (98.6°F). However, most laboratories use a commercially available DNA probe assay to confirm the mould form as B dermatitidis.[4][36][37][Figure caption and citation for the preceding image starts]: Direct potassium hydroxide preparation at 20x magnification of a sputum specimenNancy L. Wengenack, PhD, D(ABMM), Director of Mycology and Mycobacteriology Laboratories, Assistant Professor of Microbiology and Lab Medicine, Mayo Clinic, Rochester, MN [Citation ends].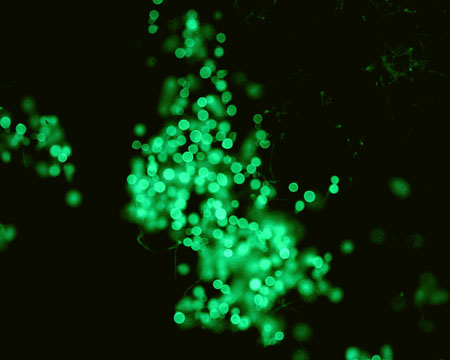
Other tests often follow more routine investigations once the diagnosis is considered:
Although a fungal serological panel is available and often ordered, it is not of sufficient sensitivity to rule out the disease and useful only if positive.[2]
Fungal blood cultures are done when disseminated disease is suspected, most usually in a patient who is immunocompromised.
Pathological examination of lesions associated with blastomycosis generally reveals findings of acute inflammation with or without necrosis, granuloma formation, and multi-nucleated giant cells.[35]
MRI may reveal evidence of intracranial blastomycosis.
Polymerase chain reaction detection of fungal organisms in bronchoalveolar lavage or tissue specimens is available in some research laboratories, but is not US Food and Drug Administration (FDA) approved or widely available clinically.[38][39][Figure caption and citation for the preceding image starts]: Axial T1 gadolinium-enhanced MRI image of cerebral blastomycosisDr William Marshall, MD, Assistant Professor of Medicine, Division of Infectious Diseases, Mayo Clinic, Rochester, MN [Citation ends].

Use of this content is subject to our disclaimer