Etiology
Stenosing tenosynovitis is caused by inflammation and catching as the tendon passes through its retinacular sheath.[1][2][3][5][16] The retinacular sheath is a fibro-osseous canal that functions as a pulley system to reorient the vector of pull of the tendon toward the hand and digits. Repetitive shear stress through the canal causes irritation to the tendon and its synovial lining (tenosynovium) with inflammation and hypertrophy, along with fibrosis of the retinacular sheath. Over time, the canal will narrow to a point that precludes smooth gliding of the tendon: stenosing tenosynivitis.[17][18] It may involve any of the 21 extrinsic (9 flexor and 12 extensor) tendons of the hand and wrist.[Figure caption and citation for the preceding image starts]: Tendons of the left handCreated by the BMJ Group [Citation ends].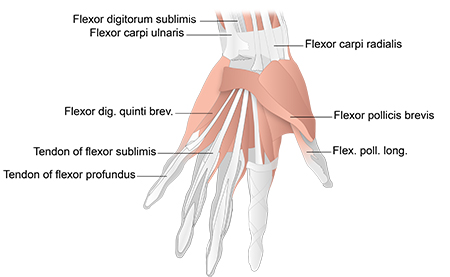 [Figure caption and citation for the preceding image starts]: Tendons of forefingerCreated by the BMJ Group [Citation ends].
[Figure caption and citation for the preceding image starts]: Tendons of forefingerCreated by the BMJ Group [Citation ends].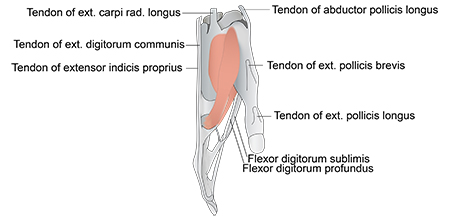 [Figure caption and citation for the preceding image starts]: Tendons of the back of the wristCreated by the BMJ Group [Citation ends].
[Figure caption and citation for the preceding image starts]: Tendons of the back of the wristCreated by the BMJ Group [Citation ends]. [Figure caption and citation for the preceding image starts]: Transverse section across the wristCreated by the BMJ Group [Citation ends].
[Figure caption and citation for the preceding image starts]: Transverse section across the wristCreated by the BMJ Group [Citation ends].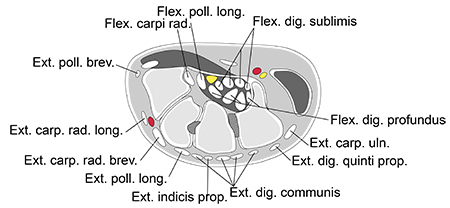
Pathophysiology
The most remarkable pathologic findings are found on the retinacular sheath surface.[19] They consist of degenerative changes and fibrocartilaginous metaplasia.[10][16] Inflammatory cells and synovial hypertrophy are rarely present. In response to canal narrowing, the tendon fibers "bunch up" proximal to the stenosed edge, forming what would be felt as a nodule or mass that catches upon passing through the pulley or sheath, or locks the tendon in flexion when gliding is no longer possible.[15][20]
Classification
Stenosing tendinopathies[2]
Trigger finger: tendonitis of the digital flexor tendon at the A1 pulley leading to catching and locking.
de Quervain disease: tendonitis of the abductor pollicis longus and extensor pollicis brevis tendons as they pass through the first dorsal compartment sheath of the wrist at the radial styloid process.
Intersection syndrome: tendonitis of the second dorsal compartment tendons as they pass under the first dorsal compartment tendons.
Extensor pollicis longus tenosynovitis.
Extensor carpi ulnaris tenosynovitis.
Flexor carpi radialis tenosynovitis.
Trigger digit classification[3]
Grade 1 (pretrigger): pain; history of catching; normal motion on exam; tenderness over the A1 pulley.
Grade 2 (active): catching present on exam, full extension possible actively.
Grade 3 (passive): locked digit in flexion (grade IIIA) or extension (grade IIIB); full motion achieved passively with assistance.
Grade 4 (contracture): fixed flexion contracture of the proximal interphalangeal joint.
Only trigger digit has a formal classification.
Trigger finger classification[4]
Grade 0: mild crepitus in the non-triggering finger.
Grade 1: no triggering, but uneven finger movements.
Grade 2: triggering is actively correctable.
Grade 3: usually correctable by the other hand.
Grade 4: the digit is locked.
Use of this content is subject to our disclaimer