Epicondylitis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
initial presentation
rest + ice + NSAID + brace/strap
The mainstay of initial treatment for medial and lateral epicondylitis is rest, ice, and activity modification of the wrist, elbow, and forearm for 6 weeks.[1]Carter RM. Epicondylitis. J Bone Joint Surg Am. 1925;7:553-62.[4]Jobe FW, Ciccotti MG. Lateral and medial epicondylitis of the elbow. J Am Acad Orthop Surg. 1994 Jan;2(1):1-8. http://www.ncbi.nlm.nih.gov/pubmed/10708988?tool=bestpractice.com [24]Ciccotti MG, Ramani MN. Medial epicondylitis. Tech Hand Up Extrem Surg. 2003 Dec;7(4):190-6. http://www.ncbi.nlm.nih.gov/pubmed/16518220?tool=bestpractice.com [59]Johnson GW, Cadwallader K, Scheffel SB, et al. Treatment of lateral epicondylitis. Am Fam Physician. 2007 Sep 15;76(6):843-8. http://www.ncbi.nlm.nih.gov/pubmed/17910298?tool=bestpractice.com
Oral nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended during the initial 10-21 days following injury. Short-term studies have demonstrated that oral diclofenac for 28 days for lateral epicondylitis is associated with improved pain but not statistically improved grip strength.[60]Pattanittum P, Turner T, Green S, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev. 2013;(5):CD003686. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003686.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/23728646?tool=bestpractice.com [61]Labelle H, Guibert R. Efficacy of diclofenac in lateral epicondylitis of the elbow also treated with immobilization. The University of Montreal Orthopaedic Research Group. Arch Fam Med. 1997 May-Jun;6(3):257-62. http://www.ncbi.nlm.nih.gov/pubmed/9161352?tool=bestpractice.com
In addition to NSAIDs, an inelastic, nonarticular, proximal forearm strap for lateral epicondylitis may be utilized. Short-term use of this bracing technique for up to 12 weeks following injury has been shown to be beneficial in lateral epicondylitis.[62]Kroslak M, Pirapakaran K, Murrell GAC. Counterforce bracing of lateral epicondylitis: a prospective, randomized, double-blinded, placebo-controlled clinical trial. J Shoulder Elbow Surg. 2019 Feb;28(2):288-295. https://www.doi.org/10.1016/j.jse.2018.10.002 http://www.ncbi.nlm.nih.gov/pubmed/30658774?tool=bestpractice.com There is no difference in symptom improvement using a brace confined to a forearm compared with a brace with a strap above the elbow.[63]Bisset LM, Collins NJ, Offord SS. Immediate effects of 2 types of braces on pain and grip strength in people with lateral epicondylalgia: a randomized controlled trial. J Orthop Sports Phys Ther. 2014 Feb;44(2):120-8. http://www.ncbi.nlm.nih.gov/pubmed/24405258?tool=bestpractice.com
Conservative treatment should be continued for about 6 weeks.
The use of transcutaneous electrical nerve stimulation (TENS) devices does not appear to provide additional benefit.[64]Chesterton LS, Lewis AM, Sim J, et al. Transcutaneous electrical nerve stimulation as adjunct to primary care management for tennis elbow: pragmatic randomised controlled trial (TATE trial). BMJ. 2013 Sep 2;347:f5160. http://www.bmj.com/content/347/bmj.f5160 http://www.ncbi.nlm.nih.gov/pubmed/23999980?tool=bestpractice.com
Primary options
diclofenac potassium: 50 mg orally (immediate-release) three times daily when required, maximum 150 mg/day
OR
ibuprofen: 400-800 mg orally every 6-8 hours when required, maximum 2400 mg/day
OR
naproxen: 500 mg orally twice daily when required
OR
meloxicam: 15 mg once orally daily when required
OR
celecoxib: 200 mg orally once daily when required
no response to initial treatment at 6 weeks
physical therapy ± local anesthetic injection
The physical exam should be repeated to re-evaluate for other etiologic processes. Radiographic and/or electrophysiological studies may also be indicated to further evaluate the patient.
Formal physical therapy procedures, with or without local injections of local anesthetic, may be beneficial and should include an eccentric loading program.[65]Herd CR, Meserve BB. A systematic review of the effectiveness of manipulative therapy in treating lateral epicondylalgia. J Man Manip Ther. 2008;16(4):225-37. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2716156 http://www.ncbi.nlm.nih.gov/pubmed/19771195?tool=bestpractice.com [66]Raman J, MacDermid JC, Grewal R. Effectiveness of different methods of resistance exercises in lateral epicondylosis - a systematic review. J Hand Ther. 2012 Jan-Mar;25(1):5-25. http://www.ncbi.nlm.nih.gov/pubmed/22075055?tool=bestpractice.com [67]Cullinane FL, Boocock MG, Trevelyan FC. Is eccentric exercise an effective treatment for lateral epicondylitis? A systematic review. Clin Rehabil. 2014 Jan;28(1):3-19. http://www.ncbi.nlm.nih.gov/pubmed/23881334?tool=bestpractice.com [68]Olaussen M, Holmedal O, Lindbaek M, et al. Treating lateral epicondylitis with corticosteroid injections or non-electrotherapeutical physiotherapy: a systematic review. BMJ Open. 2013 Oct 29;3(10):e003564. http://bmjopen.bmj.com/content/3/10/e003564.long http://www.ncbi.nlm.nih.gov/pubmed/24171937?tool=bestpractice.com [69]Peterson M, Butler S, Eriksson M, et al. A randomized controlled trial of eccentric vs. concentric graded exercise in chronic tennis elbow (lateral elbow tendinopathy). Clin Rehabil. 2014 Sep;28(9):862-72. http://www.ncbi.nlm.nih.gov/pubmed/24634444?tool=bestpractice.com [70]McQueen KS, Powell RK, Keener T, et al. Role of strengthening during nonoperative treatment of lateral epicondyle tendinopathy. J Hand Ther. 2021 Oct-Dec;34(4):619-26. http://www.ncbi.nlm.nih.gov/pubmed/33250396?tool=bestpractice.com Radial nerve mobilization techniques have also been found to provide effective short-term pain relief in a small randomized controlled trial.[71]Yilmaz K, Yigiter Bayramlar K, Ayhan C, et al. Investigating the effects of neuromobilization in lateral epicondylitis. J Hand Ther. 2022 Jan-Mar;35(1):97-106. http://www.ncbi.nlm.nih.gov/pubmed/33563509?tool=bestpractice.com
Some physicians inject both lidocaine and bupivacaine. They do this on the basis that lidocaine has a rapid onset, allowing the injection to have good diagnostic value, whereas bupivacaine is longer-acting with a longer onset.
Patients should be monitored every 6-8 weeks for 6 months to assess progress, such as whether they have returned to work or are participating in any sport.
lateral epicondylitis refractory to treatment 6-12 months after initial presentation
surgery
Surgical intervention for both medial and lateral epicondylitis is limited to refractory cases.[4]Jobe FW, Ciccotti MG. Lateral and medial epicondylitis of the elbow. J Am Acad Orthop Surg. 1994 Jan;2(1):1-8. http://www.ncbi.nlm.nih.gov/pubmed/10708988?tool=bestpractice.com [24]Ciccotti MG, Ramani MN. Medial epicondylitis. Tech Hand Up Extrem Surg. 2003 Dec;7(4):190-6. http://www.ncbi.nlm.nih.gov/pubmed/16518220?tool=bestpractice.com [59]Johnson GW, Cadwallader K, Scheffel SB, et al. Treatment of lateral epicondylitis. Am Fam Physician. 2007 Sep 15;76(6):843-8. http://www.ncbi.nlm.nih.gov/pubmed/17910298?tool=bestpractice.com All patients should be informed preoperatively of possible decreased grip strength after surgery.[4]Jobe FW, Ciccotti MG. Lateral and medial epicondylitis of the elbow. J Am Acad Orthop Surg. 1994 Jan;2(1):1-8. http://www.ncbi.nlm.nih.gov/pubmed/10708988?tool=bestpractice.com
Systematic reviews have suggested that the current evidence is insufficient to support or refute the effectiveness of surgical intervention.[79]Buchbinder R, Johnston RV, Barnsley L, et al. Surgery for lateral elbow pain. Cochrane Database Syst Rev. 2011;(3):CD003525. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003525.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/21412883?tool=bestpractice.com [80]Bateman M, Littlewood C, Rawson B, et al. Surgery for tennis elbow: a systematic review. Shoulder Elbow. 2019 Feb;11(1):35-44. https://www.doi.org/10.1177/1758573217745041 http://www.ncbi.nlm.nih.gov/pubmed/30719096?tool=bestpractice.com
Systematic reviews and one randomized controlled trial (published subsequent to systematic review searches) report no significant differences between arthroscopic and open surgery (e.g., functional outcomes, failure rate, pain relief) in patients with lateral epicondylitis.[81]Moradi A, Pasdar P, Mehrad-Majd H, et al. Clinical Outcomes of Open versus Arthroscopic Surgery for Lateral Epicondylitis, Evidence from a Systematic Review. Arch Bone Jt Surg. 2019 Mar;7(2):91-104. http://www.ncbi.nlm.nih.gov/pubmed/31211187?tool=bestpractice.com [82]Wang W, Chen J, Lou J, et al. Comparison of arthroscopic debridement and open debridement in the management of lateral epicondylitis: A systematic review and meta-analysis. Medicine (Baltimore). 2019 Nov;98(44):e17668. https://www.doi.org/10.1097/MD.0000000000017668 http://www.ncbi.nlm.nih.gov/pubmed/31689781?tool=bestpractice.com [83]Clark T, McRae S, Leiter J, et al. Arthroscopic Versus Open Lateral Release for the Treatment of Lateral Epicondylitis: A Prospective Randomized Controlled Trial. Arthroscopy. 2018 Dec;34(12):3177-3184. https://www.doi.org/10.1016/j.arthro.2018.07.008 http://www.ncbi.nlm.nih.gov/pubmed/30509427?tool=bestpractice.com One review found that postoperative complications (such as mild flexion-extension limitation, hematoma, wound infection, revision requirement, forearm paresthesias for 2 weeks after surgery) were significantly more common following open surgery.[81]Moradi A, Pasdar P, Mehrad-Majd H, et al. Clinical Outcomes of Open versus Arthroscopic Surgery for Lateral Epicondylitis, Evidence from a Systematic Review. Arch Bone Jt Surg. 2019 Mar;7(2):91-104. http://www.ncbi.nlm.nih.gov/pubmed/31211187?tool=bestpractice.com Arthroscopic surgery was associated with increased operative time.[82]Wang W, Chen J, Lou J, et al. Comparison of arthroscopic debridement and open debridement in the management of lateral epicondylitis: A systematic review and meta-analysis. Medicine (Baltimore). 2019 Nov;98(44):e17668. https://www.doi.org/10.1097/MD.0000000000017668 http://www.ncbi.nlm.nih.gov/pubmed/31689781?tool=bestpractice.com [83]Clark T, McRae S, Leiter J, et al. Arthroscopic Versus Open Lateral Release for the Treatment of Lateral Epicondylitis: A Prospective Randomized Controlled Trial. Arthroscopy. 2018 Dec;34(12):3177-3184. https://www.doi.org/10.1016/j.arthro.2018.07.008 http://www.ncbi.nlm.nih.gov/pubmed/30509427?tool=bestpractice.com
Long-term follow up data are limited. Single-surgeon series (with mean follow-up >9.8 years) report subjective overall improvement in >90% of patients who underwent an open surgical procedure for lateral epicondylitis.[84]Dunn JH, Kim JJ, Davis L, et al. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008 Feb;36(2):261-6. http://www.ncbi.nlm.nih.gov/pubmed/18055917?tool=bestpractice.com [85]Coleman B, Quinlan JF, Matheson JA. Surgical treatment for lateral epicondylitis: a long-term follow-up of results. J Shoulder Elbow Surg. 2010 Apr;19(3):363-7. https://www.doi.org/10.1016/j.jse.2009.09.008 http://www.ncbi.nlm.nih.gov/pubmed/20004594?tool=bestpractice.com In one series, patient satisfaction averaged 8.9/10.[84]Dunn JH, Kim JJ, Davis L, et al. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008 Feb;36(2):261-6. http://www.ncbi.nlm.nih.gov/pubmed/18055917?tool=bestpractice.com
ultrasound-guided minimally invasive tenotomy
Ultrasound-guided minimally invasive tenotomy has shown symptomatic improvement in nonrandomized studies.[87]Dakkak M, Patel V, King D, et al. Ultrasound-guided tenotomy for lateral epicondylitis with TenJet improves physical functional and decreased pain outcomes at 1 year: a case series review. JSES Int. 2023 Sep;7(5):872-6. https://pmc.ncbi.nlm.nih.gov/articles/PMC10499850 http://www.ncbi.nlm.nih.gov/pubmed/37719823?tool=bestpractice.com
It is a safe and effective treatment option for chronic refractory lateral and medial elbow tendinopathy, showing significant pain and function improvements over one year. Further research is required to assess its effectiveness in diverse patient populations using controlled study designs.[88]Barnes DE, Beckley JM, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2015 Jan;24(1):67-73. http://www.ncbi.nlm.nih.gov/pubmed/25306494?tool=bestpractice.com
dry needling
Dry needling is a low-cost, minimally invasive, and low-risk therapy for refractory lateral epicondylitis. It involves multiple needle insertions into the extensor carpi radialis brevis tendon and is usually performed percutaneously under local anesthetic. Dry needling has been shown to provide symptomatic improvement in a few small studies.[89]Uygur E, Aktaş B, Özkut A, et al. Dry needling in lateral epicondylitis: a prospective controlled study. Int Orthop. 2017 Nov;41(11):2321-5. http://www.ncbi.nlm.nih.gov/pubmed/28828509?tool=bestpractice.com [90]Nagarajan V, Ethiraj P, Prasad P A, et al. Local corticosteroid injection versus dry needling in the treatment of lateral epicondylitis. Cureus. 2022 Nov;14(11):e31286. https://pmc.ncbi.nlm.nih.gov/articles/PMC9733488 http://www.ncbi.nlm.nih.gov/pubmed/36514597?tool=bestpractice.com
extracorporeal shock wave therapy
Extracorporeal shock wave therapy may be effective in patients with risk factors precluding surgery, or who wish to avoid surgery.[91]Kohia M, Brackle J, Byrd K, et al. Effectiveness of physical therapy treatments on lateral epicondylitis. J Sport Rehabil. 2008 May;17(2):119-36. http://www.ncbi.nlm.nih.gov/pubmed/18515912?tool=bestpractice.com
Systematic reviews suggest that extracorporeal shock wave therapy may be of modest benefit in the management of lateral epicondylitis, but high-quality RCTs are required.[92]Xiong Y, Xue H, Zhou W, et al. Shock-wave therapy versus corticosteroid injection on lateral epicondylitis: a meta-analysis of randomized controlled trials. Phys Sportsmed. 2019 Sep;47(3):284-289. https://www.doi.org/10.1080/00913847.2019.1599587 http://www.ncbi.nlm.nih.gov/pubmed/30951399?tool=bestpractice.com [93]Yao G, Chen J, Duan Y, et al. Efficacy of Extracorporeal Shock Wave Therapy for Lateral Epicondylitis: A Systematic Review and Meta-Analysis. Biomed Res Int. 2020;2020:2064781. https://www.doi.org/10.1155/2020/2064781 http://www.ncbi.nlm.nih.gov/pubmed/32309425?tool=bestpractice.com
injection with nonanesthetic agents
Injection modalities, including autologous blood, platelet-rich plasma, hyaluronic acid, and botulinum toxin, have been proposed as treatments for recalcitrant lateral and medial epicondylitis.
Autologous blood or platelet-rich plasma is injected into the tendons and is thought to stimulate a local inflammatory response. The use of injections with autologous blood/platelet-rich plasma may be considered as alternate treatments to surgical intervention, but the evidence for these therapies is currently limited.[94]Ahmad Z, Brooks R, Kang SN, et al. The effect of platelet-rich plasma on clinical outcomes in lateral epicondylitis. Arthroscopy. 2013 Nov;29(11):1851-62.
http://www.ncbi.nlm.nih.gov/pubmed/24060428?tool=bestpractice.com
[  ]
How do platelet-rich therapies affect outcomes in people with musculoskeletal soft tissue injuries?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.680/fullShow me the answer The UK National Institute for Health and Care Excellence (NICE) recommends autologous blood products for the treatment of tendinopathy; however, their effectiveness is uncertain.[96]National Institute for Health and Care Excellence. Autologous blood injection for tendinopathy. Jan 2013 [internet publication].
https://www.nice.org.uk/guidance/ipg438
]
How do platelet-rich therapies affect outcomes in people with musculoskeletal soft tissue injuries?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.680/fullShow me the answer The UK National Institute for Health and Care Excellence (NICE) recommends autologous blood products for the treatment of tendinopathy; however, their effectiveness is uncertain.[96]National Institute for Health and Care Excellence. Autologous blood injection for tendinopathy. Jan 2013 [internet publication].
https://www.nice.org.uk/guidance/ipg438
Two systematic reviews in patients with lateral epicondylitis reported that autologous blood or platelet-rich plasma significantly improved pain and elbow function in the intermediate term (12-26 weeks), and that platelet-rich plasma injection improved function and pain at 24 weeks, compared with corticosteroid injections.[97]Houck DA, Kraeutler MJ, Thornton LB, et al. Treatment of Lateral Epicondylitis With Autologous Blood, Platelet-Rich Plasma, or Corticosteroid Injections: A Systematic Review of Overlapping Meta-analyses. Orthop J Sports Med. 2019 Mar;7(3):2325967119831052. https://www.doi.org/10.1177/2325967119831052 http://www.ncbi.nlm.nih.gov/pubmed/30899764?tool=bestpractice.com [98]Li A, Wang H, Yu Z, et al. Platelet-rich plasma vs corticosteroids for elbow epicondylitis: A systematic review and meta-analysis. Medicine (Baltimore). 2019 Dec;98(51):e18358. https://www.doi.org/10.1097/MD.0000000000018358 http://www.ncbi.nlm.nih.gov/pubmed/31860992?tool=bestpractice.com
However, a subsequent Cochrane review concluded that autologous blood/platelet-rich plasma injections provide little or no clinically important benefit for pain or function in patients with lateral elbow pain.[99]Karjalainen TV, Silagy M, O'Bryan E, et al. Autologous blood and platelet-rich plasma injection therapy for lateral elbow pain. Cochrane Database Syst Rev. 2021 Sep 30;9:CD010951.
http://www.ncbi.nlm.nih.gov/pubmed/34590307?tool=bestpractice.com
It also reported that it is uncertain whether the injections improve treatment success or pain relief (>50%).[99]Karjalainen TV, Silagy M, O'Bryan E, et al. Autologous blood and platelet-rich plasma injection therapy for lateral elbow pain. Cochrane Database Syst Rev. 2021 Sep 30;9:CD010951.
http://www.ncbi.nlm.nih.gov/pubmed/34590307?tool=bestpractice.com
[  ]
How do platelet-rich therapies affect outcomes in people with musculoskeletal soft tissue injuries?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.680/fullShow me the answer
]
How do platelet-rich therapies affect outcomes in people with musculoskeletal soft tissue injuries?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.680/fullShow me the answer
Reduced pain following botulinum toxin injection has been reported in people with lateral epicondylitis, but there is also a high risk of complications, including digital paresis and weakness.[100]Wong SM, Hui AC, Tong PY, et al. Treatment of lateral epicondylitis with botulinum toxin: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2005 Dec 6;143(11):793-7. http://www.ncbi.nlm.nih.gov/pubmed/16330790?tool=bestpractice.com [101]Kalichman LB, Bannuru RR, Severin M, et al. Injection of botulinum toxin for treatment of chronic lateral epicondylitis: systematic review and meta-analysis. Sem Arthritis Rheum. 2011 Jun;40(6):532-8. http://www.ncbi.nlm.nih.gov/pubmed/20822798?tool=bestpractice.com [102]Zhang T, Adatia A, Zarin W, et al. The efficacy of botulinum toxin type A in managing chronic musculoskeletal pain: a systematic review and meta analysis. Inflammopharmacology. 2011 Feb;19(1):21-34. http://www.ncbi.nlm.nih.gov/pubmed/21076878?tool=bestpractice.com [103]Lin YC, Wu WT, Hsu YC, et al. Comparative effectiveness of botulinum toxin versus non-surgical treatments for treating lateral epicondylitis: a systematic review and meta-analysis. Clin Rehabil. 2018 Feb;32(2):131-145. https://www.doi.org/10.1177/0269215517702517 http://www.ncbi.nlm.nih.gov/pubmed/28349703?tool=bestpractice.com
Hyaluronic acid injections have been shown to improve pain and grip strength in patients with chronic lateral epicondylitis when compared with placebo. No serious adverse effects were reported and improvement persisted after 1 year.[104]Petrella RJ, Cogliano A, Decaria J, et al. Management of tennis elbow with sodium hyaluronate periarticular injections. Sports Med Arthrosc Rehabilit Ther Technol. 2010 Feb 2;2:4. http://www.biomedcentral.com/1758-2555/2/4 http://www.ncbi.nlm.nih.gov/pubmed/20205851?tool=bestpractice.com However, few high-quality studies are available.
low-level laser therapy
Optimally dosed low-level laser therapy administered directly to the lateral elbow tendon insertions seems to offer short-term pain relief and less disability in lateral epicondylitis, both alone and in conjunction with an exercise regimen. There is conflicting evidence for the efficacy of this intervention.[105]Bjordal JM, Lopes-Martins RA, Joensen J, et al. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musculoskelet Disord. 2008 May 29;9:75. http://www.biomedcentral.com/1471-2474/9/75 http://www.ncbi.nlm.nih.gov/pubmed/18510742?tool=bestpractice.com [106]Baxter GD, Bleakley C, McDonough S. Clinical effectiveness of laser acupuncture: a systematic review. J Acupunct Meridian Stud. 2008 Dec;1(2):65-82. http://www.jams-kpi.com/article/S2005-2901(09)60026-1/fulltext http://www.ncbi.nlm.nih.gov/pubmed/20633458?tool=bestpractice.com [107]Chang WD, Wu JH, Yang WJ, et al. Therapeutic effects of low-level laser on lateral epicondylitis from differential interventions of Chinese-Western medicine: systematic review. Photomed Laser Surg. 2010 Jun;28(3):327-36. http://www.ncbi.nlm.nih.gov/pubmed/19874256?tool=bestpractice.com [108]Tumilty S, Munn J, McDonough S, et al. Low level laser treatment of tendinopathy: a systematic review with meta-analysis. Photomed Laser Surg. 2010 Feb;28(1):3-16. http://www.ncbi.nlm.nih.gov/pubmed/19708800?tool=bestpractice.com [109]Roberts DB, Kruse RJ, Stoll SF. The effectiveness of therapeutic class IV (10 W) laser treatment for epicondylitis. Lasers Surg Med. 2013 Jul;45(5):311-7. http://www.ncbi.nlm.nih.gov/pubmed/23733499?tool=bestpractice.com
medial epicondylitis refractory to treatment 6-12 months after initial presentation
surgery
Surgical intervention for both medial and lateral epicondylitis is limited to refractory cases.[4]Jobe FW, Ciccotti MG. Lateral and medial epicondylitis of the elbow. J Am Acad Orthop Surg. 1994 Jan;2(1):1-8.
http://www.ncbi.nlm.nih.gov/pubmed/10708988?tool=bestpractice.com
[24]Ciccotti MG, Ramani MN. Medial epicondylitis. Tech Hand Up Extrem Surg. 2003 Dec;7(4):190-6.
http://www.ncbi.nlm.nih.gov/pubmed/16518220?tool=bestpractice.com
[59]Johnson GW, Cadwallader K, Scheffel SB, et al. Treatment of lateral epicondylitis. Am Fam Physician. 2007 Sep 15;76(6):843-8.
http://www.ncbi.nlm.nih.gov/pubmed/17910298?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Surgery for refractory medial epicondylitis: probe placed on area of degenerative tendon showing loss of normal tendon appearanceFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].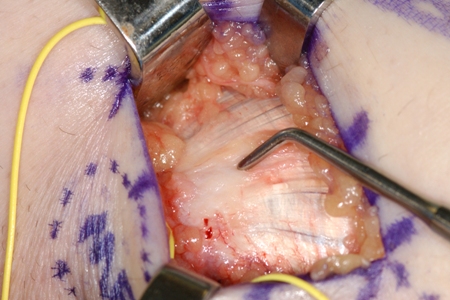 [Figure caption and citation for the preceding image starts]: Surgery for refractory medial epicondylitis: pickups lifting off area of degenerative tendon after elliptical incision to excise this areaFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Surgery for refractory medial epicondylitis: pickups lifting off area of degenerative tendon after elliptical incision to excise this areaFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].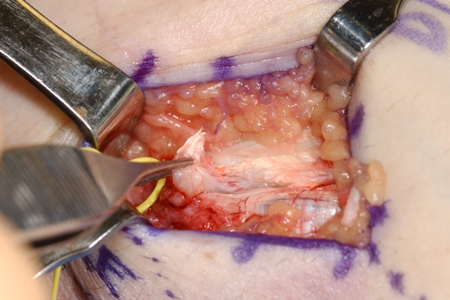 [Figure caption and citation for the preceding image starts]: Markings for swing incision location for patient with chronic refractory medial epicondylitisFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Markings for swing incision location for patient with chronic refractory medial epicondylitisFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].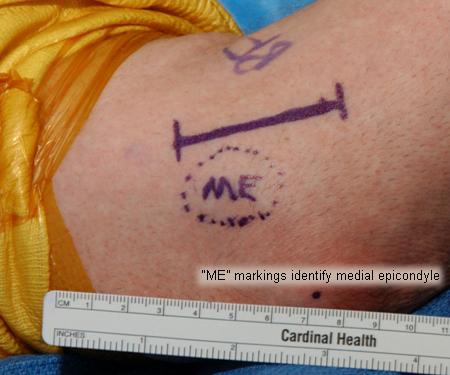 [Figure caption and citation for the preceding image starts]: Surgery for refractory medial epicondylitis: degenerative tendon removedFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Surgery for refractory medial epicondylitis: degenerative tendon removedFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].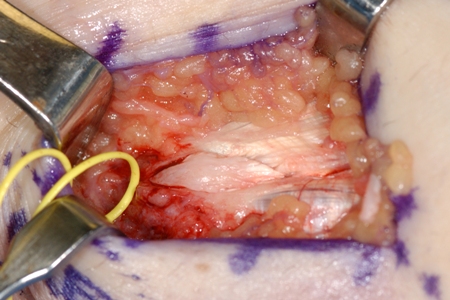 [Figure caption and citation for the preceding image starts]: Surgery for refractory medial epicondylitis: medial epicondyle exposedFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Surgery for refractory medial epicondylitis: medial epicondyle exposedFrom the collection of Dr Brian Fitzgerald, Naval Medical Center San Diego, CA; used with permission [Citation ends].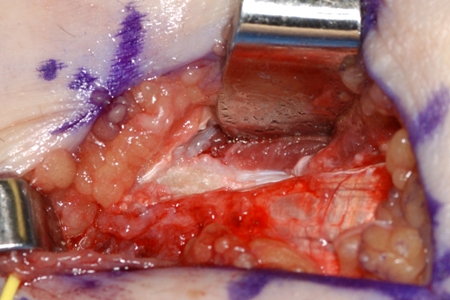
Surgical intervention for medial epicondylitis involves the open debridement and excision of the undersurface of the flexor pronator mass. Mean subjective estimate of elbow function has been found to improve from 38% to 98% of normal after surgery for medial epicondylitis.[86]Vangsness CT Jr, Jobe FW. Surgical treatment of medial epicondylitis: results in 35 elbows. J Bone Joint Surg Br. 1991 May;73(3):409-11. http://www.bjj.boneandjoint.org.uk/content/jbjsbr/73-B/3/409.full.pdf http://www.ncbi.nlm.nih.gov/pubmed/1670439?tool=bestpractice.com
Possible adverse effects of surgery include injury to ulnar nerve and/or weakness with wrist flexion.
ultrasound-guided minimally invasive tenotomy
Ultrasound-guided minimally invasive tenotomy has shown symptomatic improvement in nonrandomized studies.[87]Dakkak M, Patel V, King D, et al. Ultrasound-guided tenotomy for lateral epicondylitis with TenJet improves physical functional and decreased pain outcomes at 1 year: a case series review. JSES Int. 2023 Sep;7(5):872-6. https://pmc.ncbi.nlm.nih.gov/articles/PMC10499850 http://www.ncbi.nlm.nih.gov/pubmed/37719823?tool=bestpractice.com
It is a safe and effective treatment option for chronic refractory lateral and medial elbow tendinopathy, showing significant pain and function improvements over one year. Further research is required to assess its effectiveness in diverse patient populations using controlled study designs.[88]Barnes DE, Beckley JM, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2015 Jan;24(1):67-73. http://www.ncbi.nlm.nih.gov/pubmed/25306494?tool=bestpractice.com
injection with nonanesthetic agents
Injection modalities, including autologous blood, platelet-rich plasma, hyaluronic acid, and botulinum toxin, have been proposed as treatments for recalcitrant lateral and medial epicondylitis.
Autologous blood or platelet-rich plasma injected into the tendons and is thought to stimulate a local inflammatory response. The use of injections with autologous blood/platelet-rich plasma may be considered as alternate treatments to surgical intervention, but the evidence for these therapies is currently limited.[94]Ahmad Z, Brooks R, Kang SN, et al. The effect of platelet-rich plasma on clinical outcomes in lateral epicondylitis. Arthroscopy. 2013 Nov;29(11):1851-62. http://www.ncbi.nlm.nih.gov/pubmed/24060428?tool=bestpractice.com [95]Krogh TP, Bartels EM, Ellingsen T, et al. Comparative effectiveness of injection therapies in lateral epicondylitis: a systematic review and network meta-analysis of randomized controlled trials. Am J Sports Med. 2013 Jun;41(6):1435-46. http://www.ncbi.nlm.nih.gov/pubmed/22972856?tool=bestpractice.com The UK National Institute for Health and Care Excellence (NICE) recommends autologous blood products for the treatment of tendinopathy; however, their effectiveness is uncertain.[96]National Institute for Health and Care Excellence. Autologous blood injection for tendinopathy. Jan 2013 [internet publication]. https://www.nice.org.uk/guidance/ipg438
Two systematic reviews in patients with lateral epicondylitis reported that autologous blood or platelet-rich plasma significantly improved pain and elbow function in the intermediate term (12-26 weeks), and that platelet-rich plasma injection improved function and pain at 24 weeks, compared with corticosteroid injections.[97]Houck DA, Kraeutler MJ, Thornton LB, et al. Treatment of Lateral Epicondylitis With Autologous Blood, Platelet-Rich Plasma, or Corticosteroid Injections: A Systematic Review of Overlapping Meta-analyses. Orthop J Sports Med. 2019 Mar;7(3):2325967119831052. https://www.doi.org/10.1177/2325967119831052 http://www.ncbi.nlm.nih.gov/pubmed/30899764?tool=bestpractice.com [98]Li A, Wang H, Yu Z, et al. Platelet-rich plasma vs corticosteroids for elbow epicondylitis: A systematic review and meta-analysis. Medicine (Baltimore). 2019 Dec;98(51):e18358. https://www.doi.org/10.1097/MD.0000000000018358 http://www.ncbi.nlm.nih.gov/pubmed/31860992?tool=bestpractice.com
However, a subsequent Cochrane review concluded that autologous blood/platelet-rich plasma injections provide little or no clinically important benefit for pain or function in patients with lateral elbow pain.[99]Karjalainen TV, Silagy M, O'Bryan E, et al. Autologous blood and platelet-rich plasma injection therapy for lateral elbow pain. Cochrane Database Syst Rev. 2021 Sep 30;9:CD010951.
http://www.ncbi.nlm.nih.gov/pubmed/34590307?tool=bestpractice.com
It also reported that it is uncertain whether the injections improve treatment success or pain relief (>50%).[99]Karjalainen TV, Silagy M, O'Bryan E, et al. Autologous blood and platelet-rich plasma injection therapy for lateral elbow pain. Cochrane Database Syst Rev. 2021 Sep 30;9:CD010951.
http://www.ncbi.nlm.nih.gov/pubmed/34590307?tool=bestpractice.com
[  ]
How do platelet-rich therapies affect outcomes in people with musculoskeletal soft tissue injuries?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.680/fullShow me the answer
]
How do platelet-rich therapies affect outcomes in people with musculoskeletal soft tissue injuries?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.680/fullShow me the answer
Reduced pain following botulinum toxin injection has been reported in people with lateral epicondylitis, but there was also a high risk of complications, including digital paresis and weakness.[100]Wong SM, Hui AC, Tong PY, et al. Treatment of lateral epicondylitis with botulinum toxin: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2005 Dec 6;143(11):793-7. http://www.ncbi.nlm.nih.gov/pubmed/16330790?tool=bestpractice.com [101]Kalichman LB, Bannuru RR, Severin M, et al. Injection of botulinum toxin for treatment of chronic lateral epicondylitis: systematic review and meta-analysis. Sem Arthritis Rheum. 2011 Jun;40(6):532-8. http://www.ncbi.nlm.nih.gov/pubmed/20822798?tool=bestpractice.com [102]Zhang T, Adatia A, Zarin W, et al. The efficacy of botulinum toxin type A in managing chronic musculoskeletal pain: a systematic review and meta analysis. Inflammopharmacology. 2011 Feb;19(1):21-34. http://www.ncbi.nlm.nih.gov/pubmed/21076878?tool=bestpractice.com [103]Lin YC, Wu WT, Hsu YC, et al. Comparative effectiveness of botulinum toxin versus non-surgical treatments for treating lateral epicondylitis: a systematic review and meta-analysis. Clin Rehabil. 2018 Feb;32(2):131-145. https://www.doi.org/10.1177/0269215517702517 http://www.ncbi.nlm.nih.gov/pubmed/28349703?tool=bestpractice.com
Hyaluronic acid injections have been shown to improve pain and grip strength in patients with chronic lateral epicondylitis when compared with placebo. No serious adverse effects were reported and improvement persisted after 1 year.[104]Petrella RJ, Cogliano A, Decaria J, et al. Management of tennis elbow with sodium hyaluronate periarticular injections. Sports Med Arthrosc Rehabilit Ther Technol. 2010 Feb 2;2:4. http://www.biomedcentral.com/1758-2555/2/4 http://www.ncbi.nlm.nih.gov/pubmed/20205851?tool=bestpractice.com However, few high-quality studies are available.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer