Approach
Prompt diagnosis and timely intervention affect the final outcomes and may prevent blindness. Practitioners should recognize their limitations and, where necessary, seek further advice or refer the patient to an ophthalmologist, especially for presentations with significant eye injury, eye pain, or periocular trauma.[30][31]
Evidence of potentially serious ocular pathology requiring specialty ophthalmic evaluation includes:
A suspicious mechanism of injury (e.g., projectile or intraocular foreign body after hammering metal on metal or using power tools)
Unexplained findings (e.g., an irregular pupil, asymmetrically low intraocular pressure, decreased vision)
Significant subconjunctival hemorrhage that precludes visualization of the sclera (due to the possibility of open globe injury).
When globe injury is suspected, stop the exam, cover the affected eye with a protective shield, and do not apply pressure. Refer the patient for complete evaluation and repair by an eye surgeon in the operating room.[30][31]
[Figure caption and citation for the preceding image starts]: The ABCs of ocular trauma evaluationAdapted from Kroesen CF et al. Mil Med 2020 Jan 7;185(suppl 1):448-53 [Citation ends].
History
Key risk factors for eye trauma include ages 18-45 years, male sex, lack of protective eyewear, workplace injuries, fireworks, and excessive exposure to ultraviolet light.
In older people, falls are an important cause of serious eye injuries, particularly in women.[9] Patients usually present with a history of trauma due to mechanical, chemical, or thermal injuries or radiation (ultraviolet or ionizing). Common symptoms include pain, decreased vision, swelling around the eye, and bleeding.
Establish:
If there are any systemic injuries
Whether there has been loss of consciousness
Any previous eye surgery
Tetanus prophylaxis status
Possible wound contamination.
For mechanical trauma, the mechanism of injury may suggest an open globe injury. For example, injury with a sharp object or a high-velocity projectile in patients without eye protection would raise concern for a laceration or rupture, respectively. Clinicians should have a high index of suspicion for an intraocular foreign body if the mechanism is suggestive, such as a high-velocity injury involving metal or wood, and should request appropriate imaging. Corneal abrasions may be caused by fingernails, animal claws, pieces of paper or cardboard, makeup applicators, hand tools, or foreign bodies lodged under the eyelid.
For chemical trauma (including exposure to radiation), determine the amount of exposure and the type of chemical agent/radiation.
Basic ophthalmologic exam
Adopt a systematic approach to the examination of the face, orbital area, eyelids, and the full eye. Topical anesthetics may aid exam.[32][33]
The following should be assessed:
External exam: face, orbital rim, ocular adnexa, conjunctiva, and sclera
Vision and intraocular pressure, if possible
Confrontation visual fields
Extraocular movements
Pupillary reactivity to light and presence of an afferent pupillary defect.
When globe injury is suspected, stop the exam, cover the affected eye with a protective shield, and do not apply pressure. Refer the patient for complete evaluation and repair by an eye surgeon in the operating room.[30][31]
Physical exam
The physical exam is essential in establishing the diagnosis and in guiding management.
Blunt trauma:
Usually presents with severe pain and decreased vision. Significant subconjunctival hemorrhage and limited ocular motility on exam may be present. The cornea is involved in >50% of all serious ocular traumas.[1] Slit-lamp exam may show corneal edema or abrasions.[34] In severe cases, there may be a rupture of the cornea or sclera.
Hyphema, traumatic mydriasis, or iridodialysis (iris separated from its root) may be present and indicate that the eye has suffered trauma with significant force. Dilated fundus examination should be performed to assess for posterior segment injuries.
A full ocular assessment is mandatory and should include the intraocular pressure (IOP), structures within the angle, clarity and stability of the lens, posterior pole, and peripheral retina.
Chemical, thermal, or radiation burns
These may present with eyelid involvement, conjunctival hyperemia and chemosis (edema of the conjunctiva), corneal epithelial defects, corneal clouding and edema, anterior chamber cells and flare, elevated IOP, or cataract.
Following exposure to radiation, symptoms occur within 5-12 hours and include photophobia, corneal pain, lacrimation, and blepharospasm.
Foreign bodies
Superficial foreign bodies in the cornea typically cause significant irritation, foreign-body sensation, and tearing. They can be visualized readily on slit-lamp exam.
For conjunctival foreign bodies, slit-lamp exam may show punctate epithelial erosions or linear vertical corneal abrasions in the upper part of the cornea. A painful eye with vertically linear corneal abrasions may indicate a foreign body embedded in the superior tarsal conjunctiva. Hyperemia and embedded material may also be present.
Eyelid eversion with careful examination of the tarsal conjunctiva should be performed.
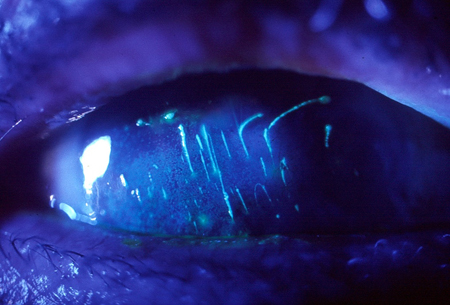
Dilated fundus exam should be performed to examine the vitreous and retina for possible foreign bodies.[Figure caption and citation for the preceding image starts]: Subtarsal foreign body. Vertical corneal abrasionsUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].
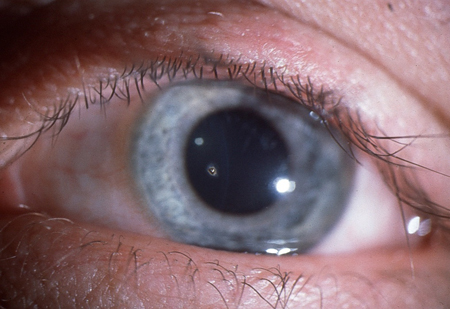
Following corneal abrasions, the pupil is typically small (reactive miosis). Slit-lamp exam may show a corneal foreign body. The depth of corneal involvement and possible penetration in the anterior chamber should be determined.[Figure caption and citation for the preceding image starts]: Corneal foreign bodyUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].
Conjunctival lacerations should raise the suspicion for injury to deeper structures and the presence of an open globe injury or intraocular foreign body. Patients may present with pain, red eye, foreign-body sensation, and a history of trauma. Slit-lamp exam shows fluorescein staining of the conjunctiva. Subconjunctival hemorrhages are often present with conjunctival lacerations.
Any suspicion of a penetrating foreign body suggests the need for imaging or a fully dilated fundus exam by an ophthalmologist to rule on the presence of an intraocular foreign body. Iris transillumination defects, irregular pupil, intraocular inflammation, vitreous hemorrhage, and decreased IOP may suggest ocular penetration. The lens should be examined for capsular integrity, cataract formation, or an embedded foreign body. Gonioscopy may be considered if no wound leak can be detected and the globe appears intact.[Figure caption and citation for the preceding image starts]: Penetrating corneal injury with iris prolapseUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].
 [Figure caption and citation for the preceding image starts]: Subconjunctival hemorrhageUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].
[Figure caption and citation for the preceding image starts]: Subconjunctival hemorrhageUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].
Open globe injuries
When globe injury is suspected, stop the exam, cover the affected eye with a protective shield, and do not apply pressure. Refer the patient for complete evaluation and repair by an eye surgeon in the operating room.[30][31]
Patients with damage to the integrity of the globe can present with decreased visual acuity, pain, and tearing. There may be subconjunctival hemorrhage and a peaked pupil (i.e., if the iris plugs the leak). Ecchymosis or other signs of damage to periorbital structures (e.g., lid lacerations) may be present. The most common areas of rupture are sites where the sclera is thinnest: the limbus (margin of the cornea where it meets the sclera), the sclera underneath the insertion of the rectus muscles, and the optic nerve head. Ruptures may also occur at sites of prior wounds, such as those from cataract surgery or corneal transplants.
A Seidel test can be used to investigate the possibility of an open globe injury.
Subconjunctival hemorrhage
This can occur following blunt trauma or following a Valsalva maneuver (e.g., coughing, sneezing, straining, or vomiting).[Figure caption and citation for the preceding image starts]: Subconjunctival hemorrhageUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].

Treatment is not required, and reassurance usually suffices. If recurrent, exclude systemic problems, such as an underlying bleeding disorder.[35]
Note that a large subconjunctival hemorrhage in the setting of significant trauma, especially if associated with other ocular findings, may be a sign of an open globe injury.
Complete eye exam
A complete eye exam should complement the general exam, although the choice will depend on the type of trauma. Exam may need to be performed under topical or general anesthesia.[30][31][32][33]
Slit-lamp exam
Eyes should be examined for possible eyelid lacerations; superficial or full-thickness lacerations to the cornea and sclera; and presence of foreign bodies. An irregular or peaked pupil may signal an open globe injury. The presence of hyphema indicates that the eye has suffered a significant injury. Close examination is required to identify injuries to other structures within the anterior and posterior segment.
Seidel test: only performed if there is suspicion for a leaking wound (omit if there is an obvious wound). To perform, apply a fluorescein strip with a few drops of sterile saline or topical proparacaine directly to the cornea and observe the effects under slit-lamp exam. Visualization of diluted dye under a blue light (a positive test) suggests an open globe injury. A corneal abrasion will show uptake in the area of missing epithelium, but it will not show dilution by aqueous.
Tonometry: used to determine intraocular pressure (IOP) by recording the resistance of the cornea. Slit lamp exam may include Goldmann applanation if there is no suspicion for an open globe injury. Handheld instruments are available (e.g., tonopen, iCare); their use will depend on the degree of eye injury. Tonometry is not performed when there is a lack of global integrity.
Gonioscopy: rarely performed as part of the initial evaluation of traumatized eyes in the emergency department. A goniolens can detect injuries to the drainage structures of the eye, such as angle recession, and may help to exclude suspected foreign body in the angle. Gonioscopy is not performed in the presence of open globe injuries.
Ophthalmoscopy
Direct ophthalmoscopy is rarely used after trauma. An ophthalmologist typically performs indirect ophthalmoscopy if a view is possible. Ophthalmoscopy can identify possible posterior segment damage, such as vitreous hemorrhage, retinal tears, commotio retinae, retinal detachment, choroidal rupture, posterior rupture, and intraocular foreign body. Dilated fundus exam, which uses mydriatic eye drops to dilate or enlarge the pupil, allows visualization of the vitreous, retina, and optic nerve.
[Figure caption and citation for the preceding image starts]: Corneal abrasion seen with fluorescein stainUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].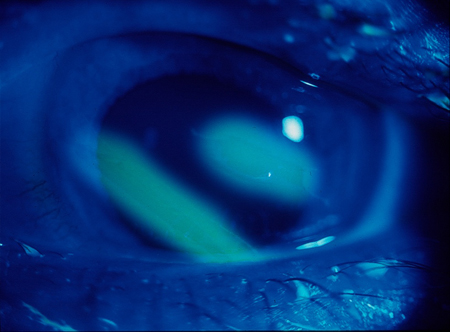
Imaging studies
The choice of imaging will depend on the clinical presentation and resource availability.[36][37][38]
Computed tomography (CT) scan orbit (without contrast)
Preferred imaging modality for evaluating orbital trauma.[36]
Indicated if intraocular or intraorbital foreign body or orbital-wall fractures are suspected, or to evaluate globe integrity.
Sensitive for detecting metallic or glass intraorbital foreign bodies.[39] However, wood is difficult to detect on CT scan.[40][41][42]
Perform thin-section axial CT with multiplanar reformation if orbital fracture or foreign body is suspected.[43]
CT scan head (without contrast)
Has a complementary role to orbital CT in the setting of concurrent head trauma and suspected intracranial abnormality, calvarial fracture, or orbital roof fracture.
Magnetic resonance imaging (MRI) scan of the head
Use supplementary to CT where greater soft tissue contrast is needed to evaluate orbital trauma and cranial injuries.
Contraindicated if a metallic intraocular foreign body is present or suspected.
May be helpful in detecting intraocular wooden foreign body.[44]
Not recommended if an open globe injury is suspected.
Other imaging
The choice of imaging will depend on the clinical presentation and resource availability.
Plain radiograph
Not recommended over CT or MRI.
Use is necessary where other imaging modalities are unavailable.
Can be used to detect foreign body or orbital-wall fracture. Intraocular foreign bodies composed of wood are particularly difficult to detect on plain radiographs.[44]
B-scan ultrasonography
Produces a two-dimensional (2D) cross-sectional view of the eye and orbit. Can be useful for evaluating the globe and its contents.
Indicated for evaluation of the posterior pole if the clarity of the ocular media does not permit a dilated fundus exam.
Useful in the identification and localization of intraocular foreign bodies.
Not recommended if an open globe injury is suspected (because tissue extrusion and contamination are a concern). However, it may be useful to detect occult open globe injuries.
Ultrasound biomicroscopy
Uses very high-frequency ultrasound to produce a 2D, cross-sectional view of the eye.
Indicated to evaluate anteriorly located foreign bodies, angle damage (e.g., cyclodialysis cleft), integrity of the lens capsule, and lens position after trauma.
Not recommended if an open globe injury is suspected.
[Figure caption and citation for the preceding image starts]: Coronal CT reconstruction with bone (a) and soft tissues (b) algorithms of an isolated orbital floor fracture. a Right orbital floor fracture with involvement of the medial aspect of the infraorbital groove (white arrow) and dislocation of a bony fragment into the maxillary sinus (empty arrow). b Mild swelling of the right inferior rectus muscle (arrowhead) partially herniated into the bony defect; huge herniation of the intraorbital fat through the fracture gap; within the herniated soft tissue, hematomas are recognizable (asterisks)Cellina M et al. Insights Imaging 2022 Jan 12;13(1):4; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Axial CT acquisition with bone (a) and soft tissues (b) algorithms in a patient with a current fracture of the right orbital medial wall (white arrow) and a previous fracture of the contralateral orbital medial wall (empty arrow). a Extensive discontinuation of the right lamina papyracea (white arrow). b The medial rectus muscle is swollen, displaced medially, and partially entrapped into the fracture (asterisk); presence of hemosinus, visible as a right posterior ethmoidal cell occupied by hyperdense material (blood) (arrow)Cellina M et al. Insights Imaging 2022 Jan 12;13(1):4; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Axial CT acquisition with bone (a) and soft tissues (b) algorithms in a patient with a current fracture of the right orbital medial wall (white arrow) and a previous fracture of the contralateral orbital medial wall (empty arrow). a Extensive discontinuation of the right lamina papyracea (white arrow). b The medial rectus muscle is swollen, displaced medially, and partially entrapped into the fracture (asterisk); presence of hemosinus, visible as a right posterior ethmoidal cell occupied by hyperdense material (blood) (arrow)Cellina M et al. Insights Imaging 2022 Jan 12;13(1):4; used with permission [Citation ends].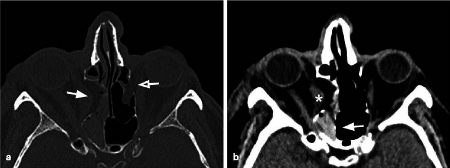
Ocular imaging
Perform ocular imaging in an ophthalmologist’s office, not in the emergency department. Studies may include:
Optical coherence tomography: for diagnosing macular pathology resulting from trauma, such as a macular hole.
Fluorescein angiography: identifies possible complications after trauma, such as choroidal neovascularization.
Fundus autofluorescence: a rapid, noninvasive technique that may help to predict the function of the retinal pigment epithelium after damage from blunt ocular trauma.
Laboratory tests
Toxicology screen may be useful, especially if surgery is indicated.
Sickle cell trait screen is indicated for people of African or Mediterranean ancestry who present with hyphema. Positive test may influence management and outcome.
Use of this content is subject to our disclaimer