Etiology
Causes of septic cavernous sinus thrombosis (CST):
Sinusitis: presently one of the most common predisposing conditions, representing an increase from 30% of all causes in the pre-antibiotic era.[2][7][8][9] The most common site of primary infection is the sphenoid sinus, followed by the ethmoid sinuses.[10][11][12][13] Infection is typically due to rare invasive and potentially resistant organisms. Early intervention improves prognosis.[12][13][14]
Facial infection (e.g., folliculitis): in the pre-antibiotic era, this was the most common cause of CST, representing approximately 60% of cases.[15]
Periorbital infection.
Mucormycosis (highly invasive fungal infection, which usually occurs in immunocompromised patients, especially those with diabetes mellitus or neutropenia): may be either rhinocerebral or otocerebral.[16][17]
Petrous apicitis (infection of the medial portion of the temporal bone at the base of the skull).[20]
Bacterial meningitis.[24]
Sepsis (other sources).
Oropharyngeal infection resulting in Lemierre syndrome, which is a syndrome of septic thrombophlebitis of the veins of the head and neck.[25]
Causes of aseptic CST:
Trauma (e.g., supraorbital, mandibular, or basilar skull fracture).[18][22][26]
Postsurgical causes (e.g., rhinoplasty, cataract extraction, skull base procedures, and dental extraction).[27][28][29]
Hypercoagulable state:
Owing to hematologic disorder (e.g., polycythemia rubra vera; sickle cell disease; acute lymphocytic leukemia; deficiencies of antithrombin III, protein C, or protein S; resistance to activated protein C; antiphospholipid antibody syndrome; thrombocytosis; elevated IgM).[22][30][31]
Owing to a nonhematologic disorder (e.g., nephrotic syndrome) or use of oral contraceptives.[32]
Malignancy (e.g., rhabdomyosarcoma and nasopharyngeal carcinoma).
Vascular abnormalities (e.g., carotid-cavernous fistula).[33]
Miscellaneous etiologies (e.g., ulcerative colitis, volume depletion, or heroin overdose).[22][34]
Idiopathic.[35]
Pathophysiology
The cavernous sinuses are trabeculated venous channels extending anteriorly from the superior orbital fissure and posteriorly to the petrous portion of the temporal bone.
[Figure caption and citation for the preceding image starts]: Anatomy of the cavernous sinus: (1) third ventricle, (2) pituitary gland, (3) oculomotor nerve, (4) trochlear nerve, (5) internal carotid artery, (6) abducens nerve, (7) ophthalmic branch of the trigeminal nerve, and (8) maxillary branch of the trigeminal nerveVisvanathan V, et al. Reminder of important clinical lesson: ocular manifestations of cavernous sinus thrombosis. BMJ Case Rep. 2010; doi:10.1136. Used with permission [Citation ends].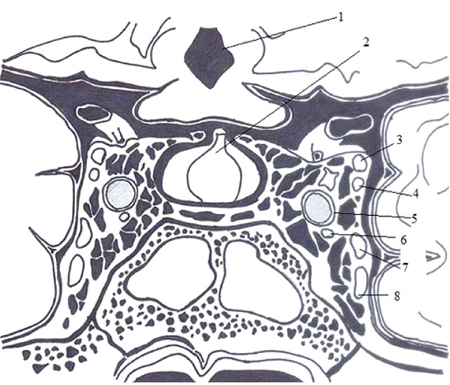
The cavernous sinuses are enclosed between the meningeal and periosteal layers of the dura. Coursing through the cavernous sinuses on each side are the internal carotid artery, cranial nerves III and IV (which lie in the lateral wall), the ophthalmic and maxillary branches of V (trigeminal nerve), and VI. These dural layers send trabeculae that give the sinuses a reticular pattern and can thereby trap bacteria, thrombi, or emboli. Bacteria also stimulate thrombogenesis by releasing toxins or by causing tissue damage.[35] Growth of the thrombus is thought to block antibiotic penetration in the cavernous sinuses. In that case, giving antibiotics will not be effective because the clot will prevent their penetration to the infected site where the bacteria are flourishing.[36][37]
The cerebral emissary veins together with the dural sinuses are valveless and thus enable blood to flow bidirectionally in accordance with the pressure gradient in the vascular system.[1] Hence, infections that spread to the cavernous sinuses from the nose, sinuses, and middle third of the face travel in an anterograde direction to the cavernous sinuses, whereas dental, lateral venous sinus, and otogenic infections travel in a retrograde direction to affect the sinuses.[38]
The mechanism of pathogenesis can also be divided into 3 types:[2]
Thrombophlebitis (vein inflammation related to a thrombus) with extension into the cavernous sinuses
Embolization of infectious material, usually after trauma, abscess, or infection
Phlebothrombosis (thrombosis of a vein without inflammation) or the aseptic form, which is differentiated from the other 2 by the absence of signs of sepsis or a primary source of infection.
Classification
Types of cavernous sinus thrombosis
Septic:
Acute septic thrombosis: a thrombophlebitic process arising from a primary source of infection. Rapidly progressive signs and symptoms, typically involving both eyes within 48 hours.
Subacute (sometimes termed chronic): similar to the acute form but with slower presentation and more subtle symptoms. Usually presents with isolated unilateral lateral gaze palsy.
Aseptic:
A thrombotic process that occurs in patients with hypercoagulable states or secondary to trauma. Presents subacutely with few or no signs and symptoms of sepsis.
Use of this content is subject to our disclaimer