Tests
1st tests to order
serum electrolytes
Test
Hypervolemic hyponatremia is common in severe heart failure due to expansion of extracellular volume.
Potassium levels are usually normal, but thiazide and loop diuretics may result in hypokalemia.
Result
hypervolemic hyponatremia; hypokalemia may be present
renal function tests
Test
Abnormal renal function tests may indicate presence of comorbidities, such as long-standing hypertension or diabetes, or other causes, such as amyloidosis.
Result
normal or increased creatinine, decreased estimated glomerular filtration rate
liver enzymes
Test
Marker of passive liver congestion.
Result
elevated aspartate transaminase, elevated alanine transaminase
B-natriuretic peptide (BNP)/N-terminal prohormone B-natriuretic peptide (NT-proBNP)
Test
BNP or NT-proBNP are raised in patients with heart failure, with concentrations rising in line with the severity of symptoms (New York Heart Association class). In patients presenting with dyspnea, natriuretic peptide biomarkers should be measured to help in the diagnosis of heart failure.[3][4]
Causes of elevated natriuretic peptides other than heart failure include left ventricular hypertrophy, myocardial ischemia, tachycardia, right ventricular overload, hypoxemia, renal dysfunction, sepsis, COPD, diabetes, age >70 years, and cirrhosis.
The presence of elevated natriuretic peptides (BNP ≥35 picograms/mL or NT-proBNP ≥125 picograms/mL) alongside other evidence of structural heart disease make the diagnosis of heart failure more likely. Higher cutoffs for natriuretic peptide levels are recommended in older people or in patients with atrial fibrillation or chronic kidney disease. Levels of BNP and NT-proBNP may be lower in patients with obesity; therefore, diagnostic sensitivity may be reduced in these patients.[2][3] Additionally, use of sacubitril/valsartan (angiotensin receptor-neprilysin inhibitor) may elevate levels of BNP, and use of NT-proBNP may be preferred in this case.[67] The presence of normal NP levels should not be used to exclude diagnosis.[11]
It is important to note the units for NT-proBNP especially when managing referrals from community settings, as some labs use picomoles/L (pmol/L) and others use picograms/mL (pg/mL). Conversation tables need to be used.
Result
elevated
CBC and iron studies
Test
Complete blood count with iron levels (transferrin saturation) and ferritin is recommended. Anemia can contribute to the patient's symptoms.
Trial data suggest that iron deficiency should be defined as ferritin <100 nanograms/mL, or 100-300 nanograms/mL if transferrin saturation is <20%.[71][72] The European Society of Cardiology recommends that all patients with heart failure should be screened for iron deficiency.[4]
Result
ferritin <100 ng/mL or 100-300 ng/mL if transferrin saturation is <20%
12-lead ECG
Test
Screening for comorbid cardiovascular disease. May reveal evidence of prior myocardial infarction, conduction defects, and arrhythmias common to HFpEF, such as atrial fibrillation. Increased QRS voltage may infer the presence of left ventricular hypertrophy; low QRS voltage can suggest infiltrative cardiomyopathy.
Result
left ventricular hypertrophy, atrial fibrillation, low voltage in infiltrative cardiomyopathy
blood glucose
Test
Screening for diabetes mellitus as a comorbid condition.
Result
elevated in diabetes
thyroid function tests
Test
Screening for comorbid hypo- or hyperthyroidism. Both can be a primary or contributory cause of heart failure.
Result
primary hypothyroidism: elevated thyroid-stimulating hormone (TSH), decreased free thyroxine (FT4); hyperthyroidism: decreased TSH, elevated free triiodothyronine, elevated FT4
blood lipids
Test
Screening for comorbid dyslipoproteinemias/metabolic syndrome.
Result
elevated in dyslipidemia; decreased in end-stage heart failure, especially in the presence of cardiac cachexia
CXR
Test
The finding of cardiomegaly is helpful in the diagnosis.
Chest x-ray also helps evaluate for pulmonary causes of dyspnea (e.g., pneumonia, pulmonary embolism, pneumothorax). In the presence of fluid overload, pulmonary edema or pleural effusion is a typical finding.
Result
cardiomegaly, pulmonary edema, pleural effusion
transthoracic echocardiography
Test
Echocardiography can be used to establish the structure and function of the left ventricle and whether there is any other pathology that might explain the patients’ presentation, such as valvular disease or pericardial disease.
Using echo, it is possible to measure whether there is left ventricular hypertrophy (LV wall thickness is normally 7-12 mm) and/or left atrial dilatation.
Echo can also be used to assess the filling pressures in the heart. The peak velocity across the mitral valve during early diastolic filling corresponds to the E wave. A is the transmitral flow during atrial contraction and corresponds to the A wave. The velocity of the E wave is determined by the balance between the rate of relaxation and the pressure gradient between the left atrium and the left ventricle in early diastole. In normal individuals, a typical E/A ratio is 1.0 to 1.5.
Tissue Doppler imaging (TDI) measures the change in velocity of the myocardial tissue itself during different phases of the cardiac cycle. Mitral annular velocity (E') has been used as a marker of diastolic function and is less preload-dependent than Doppler echocardiography.[68]
E/e' is the ratio of peak velocity across the mitral valve during early diastolic filling on routine Doppler echo and the mitral annular velocity on TDI. An E/e' ratio >15 is a reliable indicator of elevated left atrial pressure, whereas a ratio of <8 is generally found to be associated with normal filling pressure.[69]
Stage I or mild diastolic impairment: E/A ratio <1.0 due to impaired relaxation and significant contribution of atrial contraction to LV filling. Less filling of the LV in early diastole often results in enhanced contraction of the left atrium and an attendant increase in A velocity, reducing the E/A ratio. The E/e' ratio is generally normal.
Stage II or moderate diastolic impairment: E/A is normal, but E/A reversal (ratio <1.0) occurs with Valsalva maneuvers. Also called pseudo-normalization. This is due to reduced LV compliance, resulting in increased left atrial (LA) pressure. The E/e' ratio is intermediate-to-elevated in this situation.
Stage III or severe diastolic impairment: abnormal E/A ratio (>2.0), but changes with Valsalva maneuvers. Due to severe decrease in compliance, causing further increase in LA pressure. E/e' ratio is high (i.e., >15).
Stage IV (restrictive physiology): abnormal E/A ratio (>2.0) and remains fixed with Valsalva maneuvers. E/e' ratio is high (i.e., >15).
E- and A-wave velocities are affected by volume status, mitral valve dysfunction, and the presence of atrial fibrillation, so that their proper interpretation must take many of these factors into account.[69][Figure caption and citation for the preceding image starts]: Impaired relaxation: mitral inflow showing E/A reversalFrom the collection of Dr Jessica Webb; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Pseudonormalization of E/A mitral inflowFrom the collection of Dr Jessica Webb; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Pseudonormalization of E/A mitral inflowFrom the collection of Dr Jessica Webb; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Valsalva technique confirming impaired relaxationFrom the collection of Dr Marc Del Rosario [Citation ends].
[Figure caption and citation for the preceding image starts]: Valsalva technique confirming impaired relaxationFrom the collection of Dr Marc Del Rosario [Citation ends].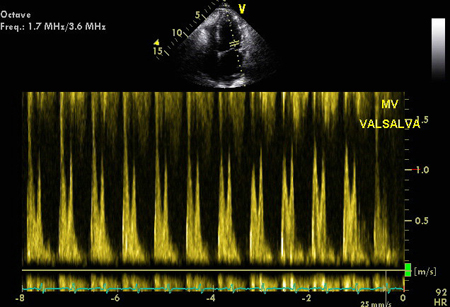 [Figure caption and citation for the preceding image starts]: Tissue Doppler imaging (TDI) of the basal LV showing increased E/E'From the collection of Dr Jessica Webb; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Tissue Doppler imaging (TDI) of the basal LV showing increased E/E'From the collection of Dr Jessica Webb; used with permission [Citation ends].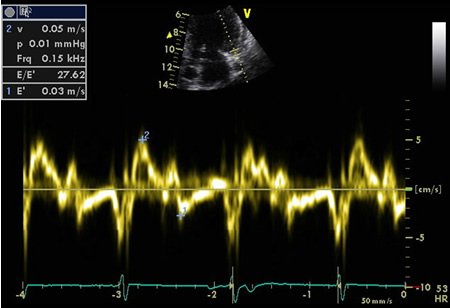 [Figure caption and citation for the preceding image starts]: Mitral inflow confirming restrictive fillingFrom the collection of Dr Jessica Webb; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral inflow confirming restrictive fillingFrom the collection of Dr Jessica Webb; used with permission [Citation ends].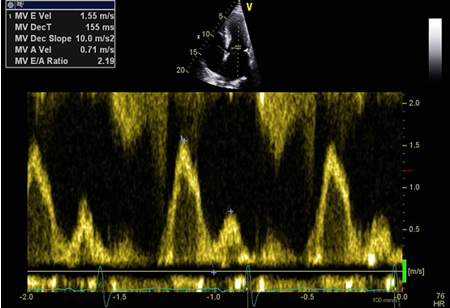
Result
assessment of LV structure and function; the presence of LV hypertrophy or left atrial dilatation; abnormal E/A ratio (normal E/A = 1.0 to 1.5); E/e’ ratio may be normal, intermediate, or high indicating the LV filling pressures
Tests to consider
cardiac magnetic resonance (CMR) imaging
Test
Gold standard for evaluating left ventricular chamber size and left ventricular mass, detecting right ventricular dysplasia, or recognizing the presence of pericardial disease. CMR can help define infiltrative causes of diastolic dysfunction, especially if employed with gadolinium contrast looking for delayed enhancement.[70]
Studies have shown that CMR has a high concordance with echocardiography in measuring mitral inflow velocities and myocardial tissue velocities, in both patients and controls.[73][74][Figure caption and citation for the preceding image starts]: CMR of patient with cardiac amyloid infiltration. Following injection of gadolinium contrast, in the late phase there is subendocardial basal ring in the left ventricle (4-chamber view)From the collection of Dr Jessica Webb; used with permission [Citation ends].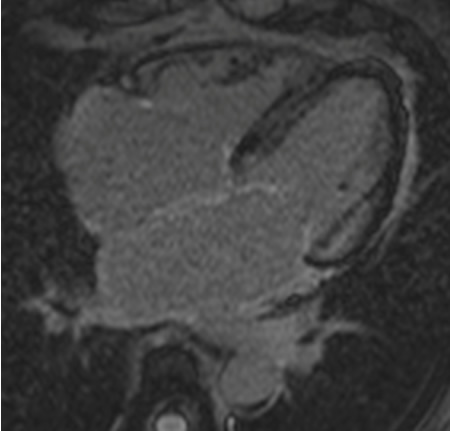 [Figure caption and citation for the preceding image starts]: CMR of patient with cardiac amyloid infiltration. Following injection of gadolinium contrast, in the late phase there is subendocardial basal ring in the left ventricle (short-axis basal image)From the collection of Dr Jessica Webb; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CMR of patient with cardiac amyloid infiltration. Following injection of gadolinium contrast, in the late phase there is subendocardial basal ring in the left ventricle (short-axis basal image)From the collection of Dr Jessica Webb; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CMR (cardiac magnetic resonance) imaging demonstrating restrictive cardiomyopathy with biatrial dilatation and mild concentric left ventricular hypertrophyFrom the collection of Dr Jessica Webb; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CMR (cardiac magnetic resonance) imaging demonstrating restrictive cardiomyopathy with biatrial dilatation and mild concentric left ventricular hypertrophyFrom the collection of Dr Jessica Webb; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CMR (cardiac magnetic resonance) imaging confirming left atrial enlargement and left ventricular hypertrophy (LVH)From the collection of Dr Jessica Webb; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CMR (cardiac magnetic resonance) imaging confirming left atrial enlargement and left ventricular hypertrophy (LVH)From the collection of Dr Jessica Webb; used with permission [Citation ends].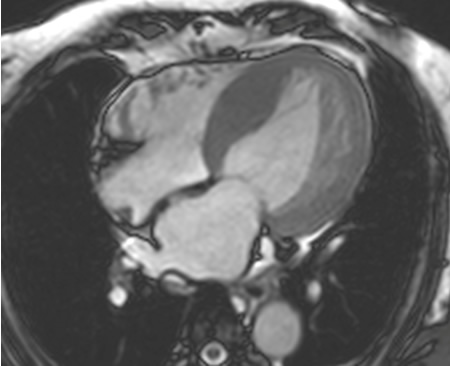
Result
abnormal cardiac systolic and diastolic function
CT angiography
Test
May be used to diagnose coronary artery disease (CAD); may be useful in evaluating chamber size and ventricular mass, detecting right ventricular dysplasia, or recognizing the presence of pericardial disease.
Result
may show CAD or pericardial disease
radionuclide ventriculography (MUGA scan)
Test
In patients where image quality is poor on echocardiography, radionuclide ventriculography can provide an assessment of left ventricular ejection fraction (EF). However, it is unable to directly assess valvular abnormalities and cardiac hypertrophy.
Result
normal EF >50%
stress testing
Test
Evaluation for ischemic heart disease and inducible myocardial ischemia is indicated in patients with HFpEF.[3][4]
May be done using exercise (e.g., treadmill, bicycle) or pharmacologic (e.g., adenosine, dobutamine) methods.
Depending on local expertise, stress echocardiography, cardiac magnetic resonance perfusion, or single photon emission computerized tomography can be used.
Result
ischemia
cardiopulmonary exercise testing (CPET)
cardiac catheterization and coronary angiography
Test
May be used to diagnose or exclude coronary artery disease (CAD).
Its invasive nature limits its clinical utility for exclusively diagnosing HFpEF in day-to-day clinical practice. However, it should be performed if the likelihood of CAD is high.
Decision to perform this test should be made by a cardiologist due to the risks of the procedure.
Result
CAD: abnormal diastolic parameters (relaxation time constant or tau, dP/dT, and LV diastolic pressure)
Use of this content is subject to our disclaimer