Tests
1st tests to order
CBC
Test
CBC with differential should be obtained on admission and at least daily. Toxic megacolon is accompanied by systemic manifestations including an elevated WBC count with left shift, although patients may present with neutropenia secondary to HIV/AIDS or sepsis. Acute blood loss or underlying chronic illness (ulcerative colitis) can cause anemia.
Result
elevated WBC count, decreased hematocrit
serum electrolytes
Test
Serum electrolytes should be obtained on admission and at least daily. Electrolyte abnormalities, especially hypomagnesemia and hypokalemia, are present as a result of significant diarrhea and volume loss.
Result
hypomagnesemia, hypokalemia
serum albumin levels
Test
Should be obtained on admission and at least daily. May be low as a result of significant diarrhea and volume loss.
Result
hypoalbuminemia
serum lactic acid
Test
Lactic acidosis may develop as a result of bowel ischemia.
Result
may be elevated
stool studies
Test
Stool samples should be sent for culture, sensitivity, and ova and parasite assay, including a Clostridium difficile assay. Wet preparations to detect fecal leukocytes, and cytomegalovirus polymerase chain reaction, should also be ordered. Rapid commercial assays, such as toxin enzyme immunoassays (EIA) and nucleic acid amplification tests (NAATs), serve as the primary diagnostic test for C difficile infection. However, toxin EIA performs poorly compared with the routine use of NAAT.
Result
may be positive for infectious organism
CT abdomen/pelvis
Test
Extremely useful in aiding the diagnosis of toxic megacolon and its complications.
Almost uniformly obtained in patients with this presentation.
Complications of toxic megacolon including perforation and abscess formation may be revealed.[25]
Do not use a protocol that involves contrast-enhanced CT acquisition in addition to unenhanced acquisition except in certain circumstances (such as gastrointestinal hemorrhage), as unenhanced images do not add diagnostic information.[26]
Result
diffuse colonic wall thickening, submucosal edema, pericolic fat stranding, colonic dilation, absence of normal haustral markings
abdominal x-ray
Test
Abdominal plain films will reveal the extent of colonic dilation and any free air under the diaphragm.[7] They are useful for monitoring and should be obtained on admission and at least daily thereafter until resolution or operative intervention.[27] An abdominal x-ray can be performed in the emergency department, and should be done in unstable patients who cannot be transported safely to the CT scanner. An upright chest x-ray can be helpful in a similar fashion.
An obstructive series including prone, supine, and upright films should be performed.
Colonic dilation >6 cm in the presence of a systemic infection is suspicious for toxic megacolon. The right and transverse colon are usually the most dilated. However, the segment of colon that is dilated may be positional; air tends to be sequestered in the transverse colon when the patient is supine due to its anterior and superior location, but in the prone position air will redistribute to the ascending and descending colon.
Patients in the upright position may demonstrate colonic air-fluid levels and the absence of normal haustral patterns. [Figure caption and citation for the preceding image starts]: Abdominal x-ray demonstrating colonic dilationUniversity of Chicago Medical Center; used with permission [Citation ends].
Result
massively dilated colon
chest x-ray
Test
An erect chest x-ray can demonstrate free air, which would indicate the need for urgent surgical intervention.
Result
free air under the diaphragm indicates perforation
Tests to consider
CRP
Test
Patients demonstrate evidence of systemic manifestations including an increased CRP, though this is not diagnostic of toxic colitis and toxic megacolon (TC/TM).
Result
elevated
erythrocyte sedimentation rate (ESR)
Test
Patients demonstrate evidence of systemic manifestations including an increased ESR, though this is not diagnostic of TC/TM.
Result
elevated
blood cultures
Test
Blood cultures should be taken in evaluation of sepsis.
Result
may be positive for pathogen
sigmoidoscopy
Test
Occasionally useful in the management of toxic colitis; used only with extreme care in toxic megacolon. May be helpful in patients presenting with pseudomembranous colitis or their first inflammatory bowel disease (IBD) flare (reserved for patients with presumed IBD or pseudomembranous colitis without a diagnosis of toxic megacolon).
Full sigmoidoscopy is contraindicated due to the risk of perforation; if performed, the scope should be passed to only 20 cm and with minimal insufflation (CO₂ preferred to air).
Endoscopic appearance varies depending on etiology. Diffuse ulcerations, raised mucosal nodules with characteristic pseudomembranes (yellowish-white plaques with normal intervening mucosa), and mucosal sloughing are typical of pseudomembranous colitis. Infectious colitis may present with thick greenish pus or yellow exudates covering the mucosal surface without the presence of ulcerations.
Result
mucosal inflammation
rectal biopsy
Test
A rectal biopsy is performed with care in those patients undergoing endoscopy.
Pseudomembranous colitis histology shows polymorphonuclear leukocytes extending into the lamina propria without destruction of deeper layers. Inclusion bodies are characteristic of cytomegalovirus colitis. These findings are characteristic of the underlying etiology and therefore may be present in the absence of toxic megacolon.[Figure caption and citation for the preceding image starts]: Histologic appearance of toxic megacolonUniversity of Chicago Medical Center; used with permission [Citation ends].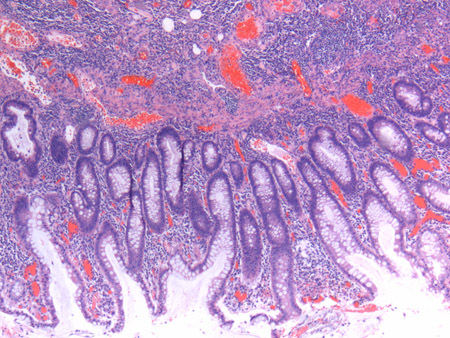
Result
histologic features typical of underlying etiology
surgical specimen
Test
Surgical specimen demonstrates extensive colonic ulceration with large areas of denuded mucosa and isolated islands of intact mucosa. [Figure caption and citation for the preceding image starts]: Gross pathology of toxic megacolonUniversity of Chicago Medical Center; used with permission [Citation ends].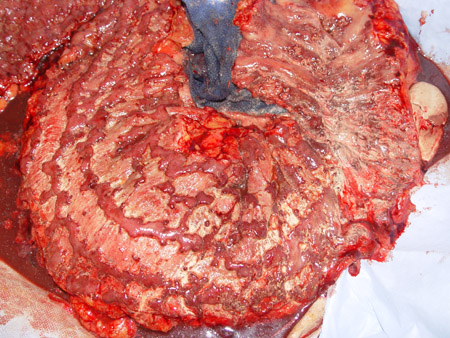
Result
colonic ulceration
Use of this content is subject to our disclaimer