Approach
Folate deficiency in the classic form presents as anemia with decreased reticulocyte numbers and oval macrocytosis (mean corpuscular volume [MCV] >100 femtoliters). Severe folate deficiency can present as pancytopenia (anemia, neutropenia, and thrombocytopenia).
Neurologic signs and symptoms are not typically seen in patients with folate deficiency.
Alternative explanations, such as coexisting vitamin B12 (cobalamin) deficiency, thiamine deficiency, or alcohol-use disorder, should be considered in cases of macrocytic anemia with neurologic signs and symptoms.
Risk groups
Certain patient groups are at increased risk for developing folate deficiency. The following groups should be considered on enquiry of medical history:
Low socioeconomic groups with poor nutrition
Older people with poor dietary intake
People who misuse alcohol (producing a sharp decline in serum folate within a few days)
Pregnant and lactating women and preterm infants (increased demand)
People with chronic hemolytic anemia or chronic exfoliative dermatitis (increased cell turnover increases folate requirement)
People taking drugs that interfere with folate absorption and metabolism, including sulfasalazine, trimethoprim, pyrimethamine, methotrexate, and anticonvulsants (e.g., phenytoin, phenobarbital)
People with hereditary folate malabsorption and inborn errors of folate metabolism, often manifesting in early life
People with chronic diarrheal states and other intestinal disorders (can cause poor absorption of folate)
Chronic peritoneal dialysis patients (folate is water soluble and lost in the dialysis fluid)
Infants who are fed goats' milk exclusively, and children with inborn errors of metabolism given a synthetic diet.
Symptoms and signs
Megaloblastic anemia is the hallmark of folate deficiency.
Severe folate deficiency presents as symptomatic macrocytic anemia and pancytopenia; nonsevere folate deficiency includes signs of macrocytosis without anemia.
Symptomatic enquiry should cover symptoms associated with anemia, including fatigue, palpitations, shortness of breath, dizziness, headaches, jaundice, loss of appetite, and weight loss. Patients may complain of painful swallowing, inflammation of the tongue (glossitis), and discomfort at the corners of the mouth (angular stomatitis) in severe folate deficiency.[Figure caption and citation for the preceding image starts]: Angular cheilitisFrom the collection of Dr Wanda C. Gonsalves; patient consent obtained [Citation ends].
Symptoms of underlying disease should also be elucidated, such as chronic diarrhea and weight loss, or failure to thrive in intestinal disorders.
A complete physical exam should be performed, looking for signs of anemia (pallor, tachycardia, tachypnea, heart murmurs, signs of heart failure, jaundice) and underlying disease (e.g., signs of chronic alcohol misuse, hemolytic anemia, exfoliative dermatitis). Petechiae may be present in those with thrombocytopenia.
Neurologic dysfunction, although rarely reported, is not typically present. The exceptions are children with inborn errors of folate absorption and metabolism, who often have severe myelopathy and neurologic dysfunction.
Initial tests
All patients with suspected folate deficiency should have a complete blood count with peripheral blood smear and reticulocyte count.
Hematologic findings
In the classic case of severe folate deficiency, the patient presents with severe anemia, oval macrocytosis (MCV >100 femtoliters), and elevated mean corpuscular hemoglobin. Corrected reticulocyte counts are decreased. As anemia advances, poikilocytes and teardrop cells appear. In extremely severe anemia, receding macrocytosis has been reported, a probable effect of poikilocytosis and red blood cell (RBC) fragmentation.[37]
Classic findings may not always be present, or may be altered:
In early folate deficiency states, the hemoglobin and MCV are normal. As the deficiency progresses, there is an increase in MCV, followed by reduced hemoglobin.
Macrocytosis can be masked by coexisting iron deficiency or thalassemia. Iron studies may not reveal deficiency initially; the true iron status becomes evident several days after initiating folic acid therapy.
Transfusion of infants with pancytopenia can lead to neutropenia and thrombocytopenia as the only hematologic features.
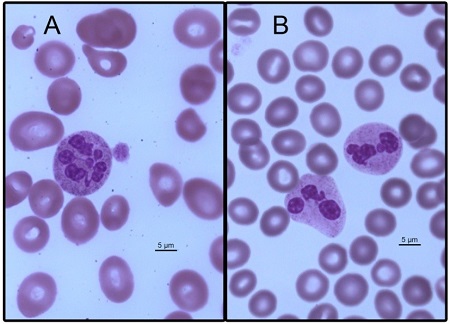
The presence of hypersegmented neutrophils is a characteristic feature of folate deficiency. It is defined as the presence of 5 lobes in >5% of neutrophils, or the presence of 1 or more neutrophils with 6 or more lobes. Hypersegmentation often precedes anemia, but is not found in subclinical vitamin deficiencies. It can also be present in patients receiving medications that inhibit DNA synthesis (e.g., 5-fluorouracil, hydroxyurea) and, rarely, in patients with myelofibrosis, chronic myelogenous leukemia, or a benign hereditary condition.[Figure caption and citation for the preceding image starts]: Megaloblastic macrocytic anemia: A. Peripheral blood smear of a patient with megaloblastic anemia. B. Peripheral blood smear of healthy individualPhotomicrograph from Mark J. Koury, MD; used with permission [Citation ends].
Neutropenia and thrombocytopenia are present in advanced folate deficiency.
Confirmatory tests
Serum folate concentration is the preferred test used in suspected folate deficiency.
Serum folate <3 ng/mL (7 nmol/L) indicates folate deficiency and often leads to morphologic features (megaloblastic changes in bone marrow and macrocytic anemia).[51] A folate level between 3 ng/mL and 5 ng/mL (7 nmol/L and 11 nmol/L) can cause metabolic changes (elevated plasma homocysteine), and should raise suspicion of folate and/or vitamin B12 deficiency.
Serum folate level depends on intake, and falls rapidly into the deficient range during deprivation.[1][52] False-negative serum folate test results (i.e., falsely elevated) can be found after recent folate intake. False-positive low serum folate test results may be found in patients with anorexia, alcohol consumption, normal pregnancy, and in patients on anticonvulsant medications.[53]
Approximately 5% of patients who have folate deficiency will have normal serum folate levels.[51][54] In addition, when vitamin B12 deficiency is also present, or there is active hemolysis, the serum folate concentration can be falsely elevated.[55]
When serum folate levels are borderline-low or normal, in the presence of a strong clinical suspicion and an absence of vitamin B12 deficiency, plasma homocysteine levels may be obtained to aid diagnosis (>15 micromol/L may be indicative of folate deficiency).[51][53]
In some patients, such as those with macrocytic anemia, empiric treatment with folate supplementation may be considered instead of serum folate testing.[56]
The RBC folate concentration correlates with an individual’s liver folate level and is considered a good reflection of the concentration of folate in tissue; RBC folate decreases more slowly during the 3- to 4-month turnover period of RBCs. It is particularly useful in the research setting when a single method for measurement is used. A variety of test kits are available to clinicians to measure RBC folate in different geographical settings; however, many of these kits have not been sufficiently clinically validated and a significant variation in results has been reported. RBC folate tests are not recommended in routine clinical practice.[56]
Contributory tests
Further testing should include bilirubin, liver function tests, lactate dehydrogenase (LDH), haptoglobin, and serum iron studies.
Biochemical tests
The laboratory signs of ineffective erythropoiesis and hemolysis coexist with macrocytosis and anemia; these include elevated LDH, increased unconjugated bilirubin, and low haptoglobin. Serum iron, ferritin, and transferrin receptor levels are elevated.[37]
Bone marrow aspirate and biopsy
Examination of bone marrow shows megaloblastic erythropoiesis. The morphologic hallmark of megaloblastic anemia are erythroblasts that are larger than expected based on cytoplasmic appearance, with large, uncondensed nuclei. Late-stage erythroblasts may have lobulated nuclei. Giant band cells and metamyelocytes are seen. [Figure caption and citation for the preceding image starts]: Megaloblastic marrow cellsPhotomicrograph from Mark J. Koury, MD; used with permission [Citation ends].

Bone marrow exam is not necessary to confirm the diagnosis of folate deficiency, although it can be used to exclude important causes of macrocytic anemia and pancytopenia, such as myelodysplasia or aplastic anemia.
Differential diagnosis
Underlying vitamin B12 deficiency should be ruled out before implementing therapy with folic acid, because such therapy may resolve the hematologic manifestations of vitamin B12 deficiency but allow the neurologic complications of untreated vitamin B12 deficiency to progress. However, it is important to note that vitamin B12 deficiency and folate deficiency can coexist in certain patients.
Vitamin B12 deficiency can cause megaloblastic anemia with similar symptoms and signs as those of folate deficiency.[8] Neurologic signs are, however, absent in folate deficiency (with the exception of children with inborn errors of folate absorption and metabolism, or those who have experienced severe prenatal folate deficiency).
Plasma or serum methylmalonic acid levels rise in vitamin B12 deficiency, but are normal in folate deficiency. Homocysteine levels rise in both vitamin B12 deficiency and folate deficiency.[57][58] Levels of methylmalonic acid and homocysteine can be affected by renal function.
Evaluating underlying etiology
Once folate deficiency is diagnosed, recognition of the underlying precipitating cause is important to prevent ongoing folate deficiency states.
Use of this content is subject to our disclaimer