Approach
Diagnosis of colorectal polyps can be made during endoscopy or radiologic imaging. Colonoscopy, flexible sigmoidoscopy, and computed tomography (CT) virtual colonoscopy are the primary diagnostic tools.
Resection and histologic examination of the polyp is essential to confirm the diagnosis.
Clinical evaluation
Many patients with polyps are asymptomatic and are diagnosed after investigation of a positive screening fecal immunochemical test or from a screening colonoscopy.[22]
Symptoms and signs prompting investigation that may lead to a diagnosis of colorectal polyps are those that may also lead to a diagnosis of colorectal cancer, such as rectal bleeding, iron-deficiency anemia, change in bowel habit, tenesmus, mucus discharge, fatigue, and unexplained weight loss. Most patients with bowel symptoms will not be found to have polyps or cancer.[23]
Familial polyposis syndromes should be considered if many polyps are found, particularly in younger patients.
Endoscopy
Colonoscopy or flexible sigmoidoscopy may be indicated.
Colonoscopy
The most powerful single diagnostic test, allowing full assessment of the bowel and subsequent polypectomy for histologic examination.
Colonoscopy is indicated if there is a suspicion of colorectal polyp or cancer (e.g., anemia, rectal bleeding, positive fecal immunochemical test, or change in bowel habit). It requires full mechanical bowel preparation and often necessitates sedation.
Colonoscopy is superior to CT colonography in the detection of smaller polyps.[24] Colonoscopy is associated with a 6% to 11% miss rate for large (>10 mm) polyps; miss rates are higher for smaller polyps.[25][26]
The risk of perforation is 0.58 per 1000 colonoscopies, and the risk of bleeding is 2.4 per 1000 colonoscopies.[27]
Flexible sigmoidoscopy
Flexible sigmoidoscopy is indicated if there is a suspicion of colorectal polyp or cancer in the presence of isolated fresh red rectal bleeding. The principal advantage of flexible sigmoidoscopy is the simpler bowel preparation and lack of sedation required for the test; however, it is limited in scope because the examiner cannot inspect the entire colon.
Flexible sigmoidoscopy should only be used in patients with a lower risk of proximal polyps, such as younger patients with left-sided symptoms (i.e., bright red rectal bleeding and/or tenesmus). In one retrospective observational cohort study, factors associated with increased polyp detection during flexible sigmoidoscopy included increasing age, male sex, utilization of any bowel preparation, and the maximum distance the scope is inserted during the procedure.[28]
Patients with an identified polyp on flexible sigmoidoscopy should proceed to colonoscopy (unless the presence of proximal polyps has already been excluded by another modality).
Flexible sigmoidoscopy may be performed to resect or take biopsies from polyps in the descending/sigmoid colon or rectum that have been identified using CT colonography.
Endoscopy adjuncts
Chromoendoscopy aids in the determination of hyperplastic or adenomatous polyps during colonoscopy and is useful in the assessment of flat adenomas. The colonic mucosa is dye-sprayed with indigo carmine and is viewed by magnification endoscopy, which produces different patterns according to the likely histologic subtype. Evidence suggests that chromoscopy enhances the detection of neoplasia in the colon and rectum.[29][30][31][32][33]
[  ]
]
[Figure caption and citation for the preceding image starts]: Sessile serrated lesion in white light (arrows indicate locations of margin)BMJ 2021;374:n1855 [Citation ends]. [Figure caption and citation for the preceding image starts]: Same sessile serrated lesion with chromoendoscopyBMJ 2021;374:n1855 [Citation ends].
[Figure caption and citation for the preceding image starts]: Same sessile serrated lesion with chromoendoscopyBMJ 2021;374:n1855 [Citation ends].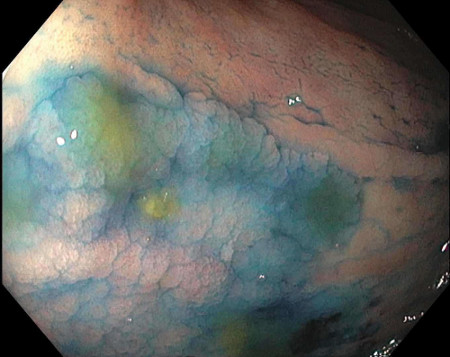
Virtual chromoendoscopy techniques such as narrow band imaging, flexible spectral imaging color enhancement, and i-scan can be used during colonoscopy to determine whether small polyps are adenomatous or hyperplastic, thus removing the need for subsequent histologic classification.[34][35][36] These technologies allow high-contrast imaging of the mucosal surface without using dyes and other equipment. Further research and endoscopic training is required to permit guidance on their optimal use.[34][37][38]
Computed tomographic colonography
Computed tomographic colonography (CTC) is a CT technique that uses air insufflation via the rectum and fecal tagging with a radiopaque contrast agent in the bowel-prepared patient. CTC provides 2D and 3D images of the site, size, and density of any suspicious lesions (including polyps). No sedation is required and the procedure takes around 10 minutes.
CTC has reasonable sensitivity and specificity for detecting larger polyps but may not be as reliable for detecting smaller polyps. In one meta-analysis, the pooled per-patient sensitivity of CTC was higher for polyps greater than 10 mm (0.82, 95% CI 0.76 to 0.88) compared with polyps 6 to 10 mm (0.63, 95% CI 0.52 to 0.75) and polyps 0 to 5 mm (0.56, 95% CI 0.42 to 0.70).[24] The perforation rate associated with CTC is very low, estimated at 0.04% in one meta-analysis.[39]
The majority of evidence suggests that CTC is an acceptable alternative to colonoscopy, particularly in patients who are either unwilling or unable to undergo colonoscopy.[1][40] The detection of significant polyps prompts endoscopic examination.[Figure caption and citation for the preceding image starts]: Virtual colonoscopy polypFrom the personal collection of Dr G. Malietzis; used with permission [Citation ends].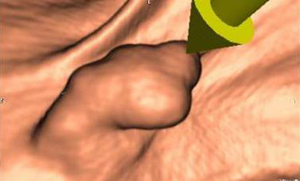
Histology
Histologic examination is the definitive test to describe morphology, dysplasia, and any evidence of invasive carcinoma in resected polyps. Representative polyp excision biopsies would be undertaken if there are many polyps (>10); however, in patients with few polyps (≤10), all polyps would be removed.
[Figure caption and citation for the preceding image starts]: This image shows a transition from areas of low-grade dysplasia (left) to high-grade dysplasia (right)Shutterstock [Citation ends].
Use of this content is subject to our disclaimer