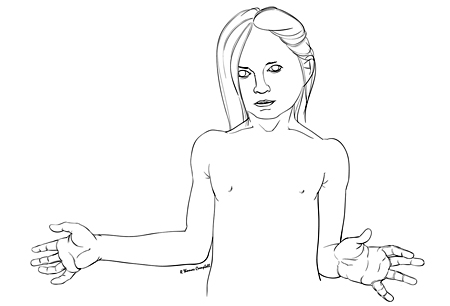
Brachial plexus birth injury presents in a newborn with decreased movement of the involved arm, most commonly in the "waiter tip" position.
Around 70% to 80% of children recover fully. Children without full recovery by 3 months are likely to have some residual impairment, most commonly to the shoulder, elbow, or forearm.
Early referral to a brachial plexus birth injury clinic is imperative for oversight of the infant’s care. This facilitates serial exams and timely surgical intervention if recovery is inadequate.
Physical or occupational therapy, including home exercises, is recommended for all children with brachial plexus birth injuries to maintain motion and prevent contracture while the nerves reinnervate muscles affected by the initial injury.
Nerve or musculoskeletal reconstruction may be needed to improve function in babies or children with incomplete recovery.
Brachial plexus birth injury (BPBI) is a paralysis of the upper extremity due to an injury at the time of birth to the nerves that control movement and sensation to the upper extremity. BPBI is often associated with delivery complicated by shoulder dystocia.[1]American College of Obstetricians and Gynecologists. Neonatal brachial plexus injury. 2014 [internet publication].
https://www.acog.org/clinical/clinical-guidance/task-force-report/articles/2014/neonatal-brachial-plexus-palsy
[2]Abzug JM, Mehlman CT, Ying J. Assessment of current epidemiology and risk factors surrounding brachial plexus birth palsy. J Hand Surg Am. 2019 Jun;44(6):515.e1-515.e10.
http://www.ncbi.nlm.nih.gov/pubmed/30266479?tool=bestpractice.com
[3]Royal College of Obstetricians and Gynaecologists. Shoulder dystocia: green-top guideline no 42. March 2012 [internet publication].
https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_42.pdf
Alternative terms include neonatal brachial plexus palsy, obstetric brachial plexus palsy, and obstetric brachial plexus injury.[4]Phua PD, Al-Samkari HT, Borschel GH. Is the term "obstetrical brachial plexus palsy" obsolete? An international survey to assess consensus among peripheral nerve surgeons. J Plast Reconstr Aesthet Surg. 2012;65(9):1227-32.
http://www.ncbi.nlm.nih.gov/pubmed/22512941?tool=bestpractice.com
The most common type of BPBI is Erb palsy (C5 to C6 nerve involvement), accounting for about 45% of cases of BPBI.[5]Erb W. Uber eine eigentumliche lokalisation von lahmungen im plexusbrachialis. Naturhist Med Vehr Heidelberg Vehr. 1874;2:130-6.[6]Smith NC, Rowan P, Benson LJ, et al. Neonatal brachial plexus palsy: outcome of absent biceps function at three months of age. J Bone Joint Surg Am. 2004 Oct;86-A(10):2163-70.
http://www.ncbi.nlm.nih.gov/pubmed/15466724?tool=bestpractice.com
An additional injury to C7, referred to as extended Erb palsy, is discovered in roughly 20% to 30% of cases of BPBI.[6]Smith NC, Rowan P, Benson LJ, et al. Neonatal brachial plexus palsy: outcome of absent biceps function at three months of age. J Bone Joint Surg Am. 2004 Oct;86-A(10):2163-70.
http://www.ncbi.nlm.nih.gov/pubmed/15466724?tool=bestpractice.com
[7]Heise CO, Zaccariotto M, Martins RS, et al. Self-biting behavior in patients with neonatal brachial plexus palsy. Childs Nerv Syst. 2022 Sep;38(9):1773-6.
http://www.ncbi.nlm.nih.gov/pubmed/35723725?tool=bestpractice.com
Total plexus involvement (C5 to T1), or global plexus palsy, represents about 20% of cases of BPBI.[6]Smith NC, Rowan P, Benson LJ, et al. Neonatal brachial plexus palsy: outcome of absent biceps function at three months of age. J Bone Joint Surg Am. 2004 Oct;86-A(10):2163-70.
http://www.ncbi.nlm.nih.gov/pubmed/15466724?tool=bestpractice.com
[8]Abid A. Brachial plexus birth palsy: Management during the first year of life. Orthop Traumatol Surg Res. 2016 Feb;102(1 suppl):S125-32.
https://www.doi.org/10.1016/j.otsr.2015.05.008
http://www.ncbi.nlm.nih.gov/pubmed/26774906?tool=bestpractice.com
Klumpke palsy (C8 to T1) is the least common, comprising less than 1% of cases of BPBI.[7]Heise CO, Zaccariotto M, Martins RS, et al. Self-biting behavior in patients with neonatal brachial plexus palsy. Childs Nerv Syst. 2022 Sep;38(9):1773-6.
http://www.ncbi.nlm.nih.gov/pubmed/35723725?tool=bestpractice.com
[9]al-Qattan MM, Clarke HM, Curtis CG. Klumpke's birth palsy: does it really exist? J Hand Surg Br. 1995 Feb;20(1):19-23.
http://www.ncbi.nlm.nih.gov/pubmed/7759926?tool=bestpractice.com